-
Original Article
Gastrin-releasing peptide receptor: a promising new biomarker to identify cervical precursor lesions and cancer
Revista Brasileira de Ginecologia e Obstetrícia. 2025;47:e-rbgo4
03-18-2025
Summary
Original ArticleGastrin-releasing peptide receptor: a promising new biomarker to identify cervical precursor lesions and cancer
Revista Brasileira de Ginecologia e Obstetrícia. 2025;47:e-rbgo4
03-18-2025Views78Abstract
Objective:
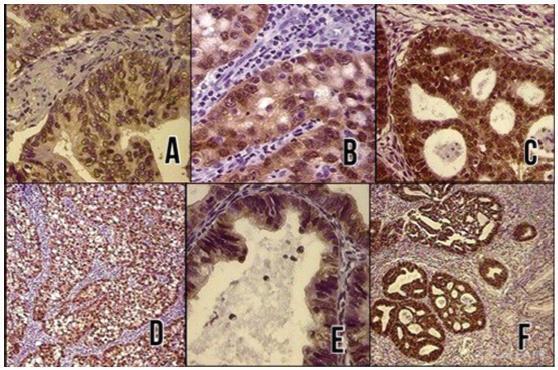
This study aimed to verify the relation between gastrin-releasing peptide receptor (GRPR), oncogenic Human Papillomavirus (HPV) and cervical lesions severity.
Methods:
GRPR mRNA levels were evaluated in cervical cancer-derived cell lines and in primary keratinocytes expressing HPV16 oncogenes by RT-PCR. GRPR protein expression was assessed by immunohistochemistry in organotypic cell cultures derived from keratinocytes transduced with HPV16 oncogenes and in 208 cervical samples, including 59 non-neoplastic tissue, 28 cervical intraepithelial neoplasia grade 3 (CIN3), 44 squamous cell carcinomas (SCC) and 77 adenocarcinomas (ADC). Generic primers (GP5+/GP6+) were used to identify HPV infection in tissue samples. Experiments involving cell lines were analyzed through non-parametric tests (Kruskal Wallis), and Fisher's Exact Test for human tissues samples. All statistical tests were considered significant at p <0.05. Immunohistochemical evaluation was conducted independently and blindly by two observers (AD- LO). Any discordant findings were resolved through discussion to reach a consensus score.
Results:
GRPR mRNA levels were not increased in cells expressing HPV16 or HPV18 oncogenes. However, at the protein level, GRPR was upregulated in organotypic cell cultures containing HPV oncogenes. Besides, it was identified an association between GRPR expression and cervical lesion severity (p < 0.0001). The detection rate of high-risk HPV DNA was directly correlated with cervical disease. Nonetheless, HPV infection was not directly associated with GRPR in cervical samples.
Conclusion:
GRPR expression is highly predictive of cervical lesion severity, irrespective of HPV infection and might contribute to improving patient's therapeutic management as well as being used a marker of disease progression.
Key-words AdenocarcinomaCarcinoma, squamous cellGastrin-releasing peptide receptorHuman papillomavirusOncogenesPapillomavirus infectionsUterine cervical dysplasiaUterine cervical neoplasmsSee more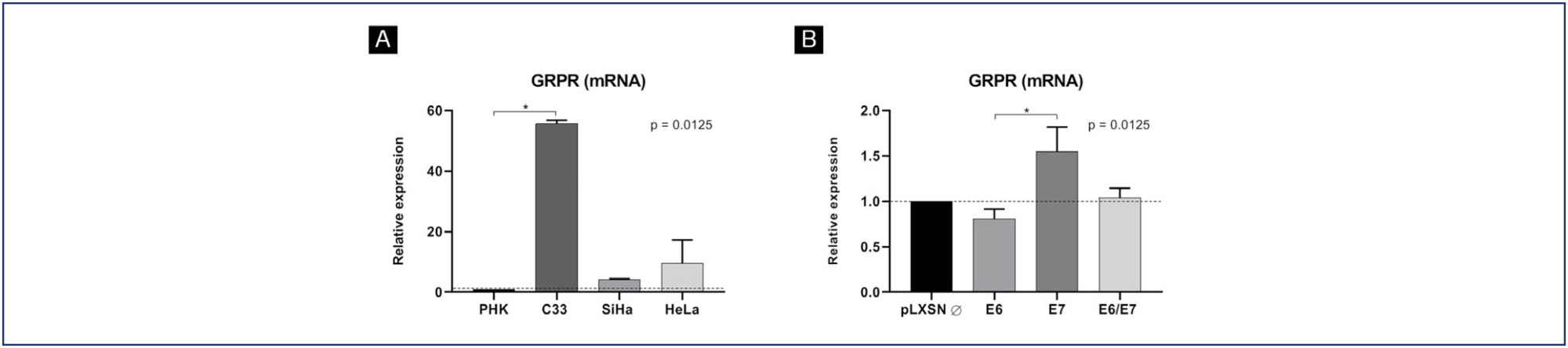
-
Original Articles
Immunohistochemical Expression of the Tumor Suppressor Protein p16 INK4a in Cervical Adenocarcinoma
Revista Brasileira de Ginecologia e Obstetrícia. 2017;39(1):21-25
01-01-2017
Summary
Original ArticlesImmunohistochemical Expression of the Tumor Suppressor Protein p16 INK4a in Cervical Adenocarcinoma
Revista Brasileira de Ginecologia e Obstetrícia. 2017;39(1):21-25
01-01-2017Views136See moreABSTRACT
Objective:
To evaluate the diagnostic utility of the p16ink4a protein expression as a marker for adenocarcinoma of the cervix.
Methods:
In a cross-sectional study, p16ink4a expression was evaluated in 30 cervical biopsies from patients diagnosed with invasive adenocarcinoma from 2 reference clinics in Brazil, and compared with 18 biopsies of endocervical polyps (control cases). The performance of the tests for p16ink4a was evaluated using a conventional contingency table, and the Kappa (k) index was used to evaluate the agreement of the marker with the tissue diagnosis.
Results:
In total, 66% of the invasive adenocarcinoma cases were positive for p16ink4a. All of the adenomatous polyps cases used as negative controls were shown to be negative for p16ink4a. The marker showed a high sensitivity and a high negative predictive value. The Kappa index was good for p16ink4a (k 1/4 0.6).
Conclusion:
Considering the strong association between the p16ink4a marker and the cervical adenocarcinoma, its use represents an important tool for reducing incorrect diagnoses of adenocarcinoma and thereby avoiding overtreatment.
-
Artigos Originais
Villoglandular adenocarcinoma of the uterine cervix
Revista Brasileira de Ginecologia e Obstetrícia. 2007;29(11):575-579
02-27-2007
Summary
Artigos OriginaisVilloglandular adenocarcinoma of the uterine cervix
Revista Brasileira de Ginecologia e Obstetrícia. 2007;29(11):575-579
02-27-2007DOI 10.1590/S0100-72032007001100005
Views75See morePURPOSE: the villoglandular adenocarcinoma (VGA) of the cervix has been identified as a variant of cervical adenocarcinoma that occurs in young women, which has an excellent prognosis. Considering the scarcity of studies related to the subject, we report six cases of VGA of the cervix. METHODS: we followed the development of six cases of VGA in the period from 1995 to 2006 at Hospital São Lucas of Pontifícia Universidade Católica do Rio Grande do Sul (PUC-RS). We collected clinical and histologic information of the patients and submitted all the surgical specimens to histological review. RESULTS: mean age at diagnosis was 43.5 years (range 27-61 years). Four patients were submitted to Wertheim-Meigs radical hysterectomy and bilateral pelvic lymphadenectomy, one to conization and subsequent radiotherapy and one to pelvic lymphadenectomy followed by radiotherapy. All the patients were alive and well at the time of this writing, without evidence of recurrence. CONCLUSIONS: the implications of therapy are discussed. We propose here the inclusion of the study of the pattern of lymphovascular involvement in determining the diagnosis of VGA. Thus, in referring to this diagnosis, we will be able to opt, with caution, for conservative therapy, except for particularities of each case.
-
Trabalhos Originais
The relationship between endometrial adenocarcinoma staging and angiogenesis
Revista Brasileira de Ginecologia e Obstetrícia. 2003;25(6):396-401
10-07-2003
Summary
Trabalhos OriginaisThe relationship between endometrial adenocarcinoma staging and angiogenesis
Revista Brasileira de Ginecologia e Obstetrícia. 2003;25(6):396-401
10-07-2003DOI 10.1590/S0100-72032003000600003
Views100See morePURPOSE: to evaluate the significance of neoangiogenesis for the prognosis of endometrial carcinoma, by quantifying and comparing the vessels with the grade of histologic differentiation and tumor staging. METHODS: the 56 studied cases consisted of 11 atrophic endometria, 10 proliferative endometria, 10 GI, 13 GII and 12 GIII adenocarcinomas. Two histologic sections were obtained for each case: one was stained with hematoxylin-eosin and the other was sent for a immunohistochemical study with anti-CD34. The utilized histometric method was vessel counting at the tumoral growth interface with the adjacent stroma, and in the control group, at the endometrial gland interface with the stroma. Couting was done by a KS300, evaluating 10 fields at 100X magnification. RESULTS: the counted vessel means were 11.6 for atrophic endometria, 13.2 for proliferative endometria, 15.3 for GI adenocarcinoma, 19 for GII adenocarcinoma, and 22.7 for GIII adenocarcinoma. In the group of stage I patients, it was observed that the mean number of vessels (18.6) was similar to that observed in stages II, III and IV (20.9) computed together. CONCLUSION: less differentiated adenocarcinomas were more angiogenic than well-differentiated carcinomas and normal endometrium. Vessel counting was not influenced by the disease stage as an isolated factor.


