-
Review Article
Efficacy, Safety, and Acceptability of Misoprostol in the Treatment of Incomplete Miscarriage: A Systematic Review and Meta-analysis
Revista Brasileira de Ginecologia e Obstetrícia. 2023;45(12):808-817
01-11-2023
Summary
Review ArticleEfficacy, Safety, and Acceptability of Misoprostol in the Treatment of Incomplete Miscarriage: A Systematic Review and Meta-analysis
Revista Brasileira de Ginecologia e Obstetrícia. 2023;45(12):808-817
01-11-2023Views264See moreAbstract
Objective
To assess the efficacy, safety, and acceptability of misoprostol in the treatment of incomplete miscarriage.
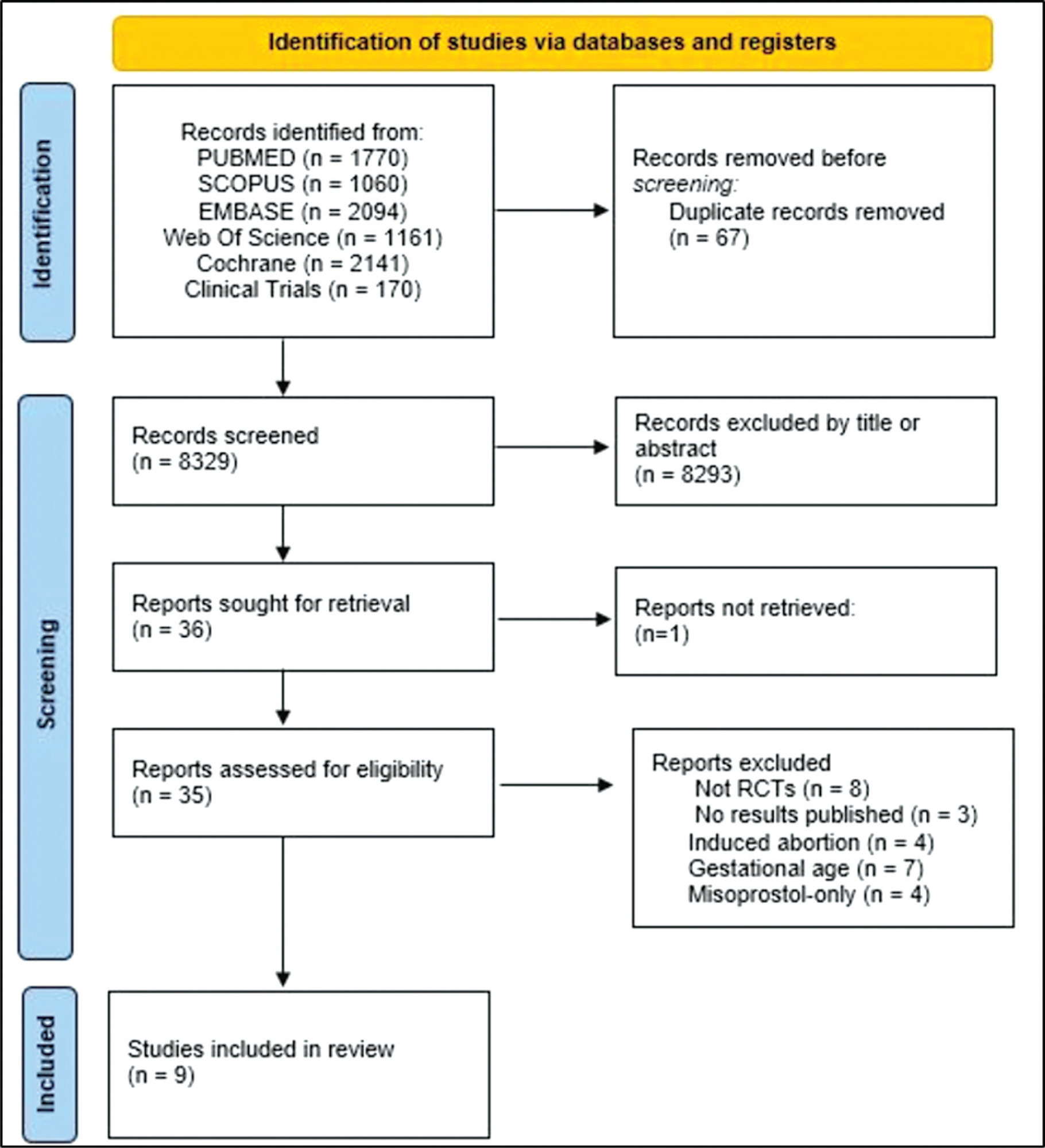
Data sources
The PubMed, Scopus, Embase, Web of Science, Cochrane Library, and Clinical Trials databases (clinicaltrials.gov) were searched for the relevant articles, and search strategies were developed using a combination of thematic Medical Subject Headings terms and text words. The last search was conducted on July 4, 2022. No language restrictions were applied.
Selection of studies
Randomized clinical trials with patients of gestational age up to 6/7 weeks with a diagnosis of incomplete abortion and who were managed with at least 1 of the 3 types of treatment studied were included. A total of 8,087 studies were screened.
Data collection
Data were synthesized using the statistical package Review Manager V.5.1 (The Cochrane Collaboration, Oxford, United Kingdom). For dichotomous outcomes, the odds ratio (OR) and 95% confidence interval (CI) were derived for each study. Heterogeneity between the trial results was evaluated using the standard test, I2 statistic.
Data synthesis
When comparing misoprostol with medical vacuum aspiration (MVA), the rate of complete abortion was higher in the MVA group (OR = 0.16; 95%CI = 0.07–0.36). Hemorrhage or heavy bleeding was more common in the misoprostol group (OR = 3.00; 95%CI = 1.96–4.59), but pain after treatment was more common in patients treated with MVA (OR = 0.65; 95%CI = 0.52–0.80). No statistically significant differences were observed in the general acceptability of the treatments.
Conclusion
Misoprostol has been determined as a safe option with good acceptance by patients.
-
Original Article
The Impact of the COVID-19 Pandemic on the Care of Women Experiencing Abortion in a University Hospital in Brazil
Revista Brasileira de Ginecologia e Obstetrícia. 2023;45(3):113-120
07-10-2023
Summary
Original ArticleThe Impact of the COVID-19 Pandemic on the Care of Women Experiencing Abortion in a University Hospital in Brazil
Revista Brasileira de Ginecologia e Obstetrícia. 2023;45(3):113-120
07-10-2023Views140Abstract
Objective
To evaluate the impact of the coronavirus disease 2019 (COVID-19) pandemic on the care of patients with miscarriage and legal termination of pregnancy in a university hospital in Brazil.
Methods
A cross-sectional study of women admitted for abortion due to any cause at Hospital da Mulher Prof. Dr. J. A. Pinotti of Universidade Estadual de Campinas (UNICAMP), Brazil, between July 2017 and September 2021. Dependent variables were abortion-related complications and legal interruption of pregnancy. Independent variables were prepandemic period (until February 2020) and pandemic period (from March 2020). The Cochran-Armitage test, Chi-squared test, Mann-Whitney test, and multiple logistic regression were used for statistical analysis.
Results
Five-hundred sixty-one women were included, 376 during the prepandemic period and 185 in the pandemic period. Most patients during pandemic were single, without comorbidities, had unplanned pregnancy, and chose to initiate contraceptive method after hospital discharge. There was no significant tendency toward changes in the number of legal interruptions or complications. Complications were associated to failure of the contraceptive method (odds ratio [OR] 2.44; 95% confidence interval [CI] 1.23–4.84), gestational age (OR 1.126; 95% CI 1.039–1.219), and preparation of the uterine cervix with misoprostol (OR 1.99; 95% CI 1.01–3.96).
Conclusion
There were no significant differences in duration of symptoms, transportation to the hospital, or tendency of reducing the number of legal abortions and increasing complications. The patients’ profile probably reflects the impact of the pandemic on family planning.
Key-words AbortionCLAP MUSA networkCOVID-19EviSIPperinatal information systempopulation surveillanceSee more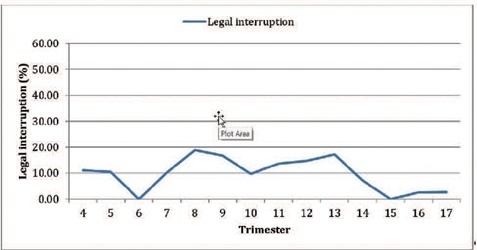
-
Original Article
Legal Pregnancy Interruption due to Sexual Violence in a Public Hospital in the South of Brazil
Revista Brasileira de Ginecologia e Obstetrícia. 2022;44(10):945-952
01-23-2022
Summary
Original ArticleLegal Pregnancy Interruption due to Sexual Violence in a Public Hospital in the South of Brazil
Revista Brasileira de Ginecologia e Obstetrícia. 2022;44(10):945-952
01-23-2022Views114See moreAbstract
Objective
To analyze the cases of all women who attend to a service of legal termination of pregnancy in cases of sexual violence in a public reference hospital and to identify the factors related to its execution.
Methods
Cross-sectional observational study with information from medical records from January 2014 to December 2020. A total of 178 cases were included, with an evaluation of the data referring to the women who attended due to sexual violence, characteristics of sexual violence, hospital care, techniques used, and complications. The analysis was presented in relative and absolute frequencies, medians, means, and standard deviation. Factors related to the completion of the procedure were assessed using binary logistic regression.
Results
Termination of pregnancy was performed in 83.2% of the cases; in 75.7% of the cases, the technique used was the association of transvaginal misoprostol and intrauterine manual aspiration. There were no deaths, and the rate of complications was 1.4%. Gestational age at the time the patient's sought assistance was the determining factor for the protocol not being completed. Pregnancies up to 12 weeks were associated with a lower chance of the interruption not occurring (odds ratio [OR]: 0.41; 95% confidence interval [CI]: 0.12–0.88), while cases with gestational age > 20 weeks were associated with a greater chance of the interruption not happening (OR: 29.93; 95%CI: 3.91–271.50).
Conclusion
The service studied was effective, with gestational age being the significant factor for resolution.
-
Original Article
Factors Associated with Abortion Complications after the Implementation of a Surveillance Network (MUSA Network) in a University Hospital
Revista Brasileira de Ginecologia e Obstetrícia. 2021;43(7):507-512
10-18-2021
Summary
Original ArticleFactors Associated with Abortion Complications after the Implementation of a Surveillance Network (MUSA Network) in a University Hospital
Revista Brasileira de Ginecologia e Obstetrícia. 2021;43(7):507-512
10-18-2021Views142See moreAbstract
Objective
To evaluate the factors associated with abortion complications following the implementation of the good-practice surveillance network Mujeres en Situación de Aborto (Women Undergoing Abortion, MUSA, in Spanish).
Methods
A cross-sectional study withwomen who underwent abortion due to any cause and in any age group at UNICAMP Women’s Hospital (part of MUSA network), Campinas, Brazil, between July 2017 and Agust 2019. The dependent variable was the presence of any abortion-related complications during hospitalization. The independent variables were clinical and sociodemographic data. The Chi-square test, the Mann-Whitney test, and multiple logistic regression were used for the statistical analysis.
Results
Overall, 305 women were enrolled (mean±standard deviation [SD] for age: 29.79±7.54 years). The mean gestational age was 11.17 (±3.63) weeks. Accidental pregnancy occurred in 196 (64.5%) cases, 91 (29.8%) due to contraception failure. At least 1 complication was observed in 23 (7.54%) women, and 8 (34.8%) of them had more than 1. The most frequent complications were excessive bleeding and infection. The factors independently associated with a higher prevalence of complications were higher gestational ages (odds ratio [OR]: 1.22; 95% confidence interval [95%CI]: 1.09 to 1.37) and contraceptive failure (OR: 3.4; 95%CI: 1.32 to 8.71).
Conclusion
Higher gestational age and contraceptive failure were associated with a higher prevalence of complications. This information obtained through the surveillance network can be used to improve care, particularly in women more susceptible to unfavorable outcomes.
-
Original Article
Disease Progression and Obstetric Outcomes of Women with Multiple Sclerosis at a Reference Center in Northeastern Brazil
Revista Brasileira de Ginecologia e Obstetrícia. 2021;43(3):165-171
05-24-2021
Summary
Original ArticleDisease Progression and Obstetric Outcomes of Women with Multiple Sclerosis at a Reference Center in Northeastern Brazil
Revista Brasileira de Ginecologia e Obstetrícia. 2021;43(3):165-171
05-24-2021Views165See moreAbstract
Objective
To describe the obstetric outcomes of patients withmultiple sclerosis (MS) and the impact of pregnancy and the postpartum period on the progression of the disease.
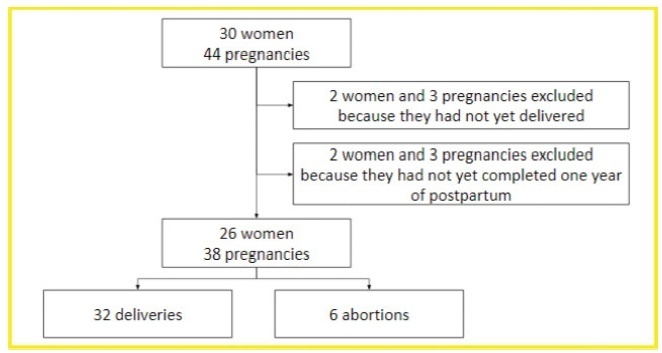
Methods
A case series study performed between December 2019 and February 2020, reporting pregnancies occurred between 1996 and 2019. The subjects included were women with MS undergoing follow-up at an MS referral center in Northeastern Brazil, and who had at least one pregnancy after the onset of MS symptoms, or who had their first relapse in the first year after delivery.
Results
In total, 26 women and 38 pregnancies were analyzed - 32 of them resulted in delivery, and the remaining 6, in miscarriages. There was a significant increase in the prevalence of relapse during the postpartum period when compared with the gestational period. In 16 (42.1%) of the pregnancies, there was exposure to diseasemodifying therapies (DMTs) - 14 (36.8%), to interferon β, and 2 (5.3%), to fingolimod. Higher rates of abortion, prematurity and low birth weight were reported in the group was exposed to DMT when compared with the one who was not.
Conclusion
In the sample of the present study, there was a significant increase in the rate of MS relapse during the postpartum period when compared with the gestational period. Additionally, it seems that exposure to DMTs during pregnancy may affect the obstetric outcomes of the patients.
-
Original Article
Advantages and Disadvantages of Medical Abortion, According to Brazilian Residents in Obstetrics and Gynaecology
Revista Brasileira de Ginecologia e Obstetrícia. 2020;42(12):793-799
01-11-2020
Summary
Original ArticleAdvantages and Disadvantages of Medical Abortion, According to Brazilian Residents in Obstetrics and Gynaecology
Revista Brasileira de Ginecologia e Obstetrícia. 2020;42(12):793-799
01-11-2020Views190See moreAbstract
Objective
To find out which was the opinion of residents in obstetrics and gynecology about the advantages and disadvantages of medical abortion as compared with surgical procedures.
Method
Cross-sectional multicenter study among residents in obstetrics and gynecology from 21 maternity hospitals located in 4 different geographical regions of Brazil, using a self-responded questionnaire with 31 questions related to their opinion and experience on providing abortion services.
Results
Most residents agreed that “being less invasive” (94.7%), “does not require anesthesia” (89.7%), “can be accompanied during the process” (89.1%), “prevents physical trauma” (84.4%) were the main advantages of medical abortion.
Conclusion
Residents perceived both clinical and personal issues as advantages of medical abortion.
-
Review Article
Abortion in Cases of Zika Virus Congenital Infection
Revista Brasileira de Ginecologia e Obstetrícia. 2018;40(7):417-424
07-01-2018
Summary
Review ArticleAbortion in Cases of Zika Virus Congenital Infection
Revista Brasileira de Ginecologia e Obstetrícia. 2018;40(7):417-424
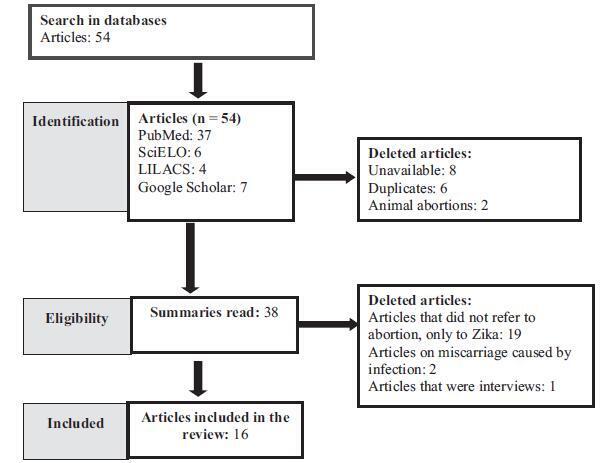
07-01-2018Views89See moreAbstract
The emergency in international public health caused by the Zika virus gave rise to the discussion about abortion in cases of congenital Zika virus syndrome (CZS). Therefore, we propose to carry out a bibliographic review on abortion in these cases. Five databases were searched using the following terms: abortion, miscarriage, and zika, with the interposition of the Boolean operator “AND.” In the selected literature, we found references to the lack of information concerning the risks and severity of CZS, to the great psychological distress suffered by pregnant women, and to the risk of unsafe abortions as a justification for abortion in cases of CZS. However, it is necessary to have available tests that could diagnose, in the first trimester of pregnancy, that the fetus has been affected by the virus, and that it may have important limitations, in order to subsidize the qualified discussion about abortion in these cases.
-
Original Article
Abortion in the Structure of Causes of Maternal Mortality
Revista Brasileira de Ginecologia e Obstetrícia. 2018;40(6):309-312
06-01-2018
Summary
Original ArticleAbortion in the Structure of Causes of Maternal Mortality
Revista Brasileira de Ginecologia e Obstetrícia. 2018;40(6):309-312
06-01-2018Views147See moreAbstract
Objective
To study the structure ofmaternalmortality caused by abortion in the Tula region.
Methods
The medical records of deceased pregnant women, childbirth, and postpartum from January 01, 2001, to December 31, 2015, were analyzed.
Results
Overall, 204,095 abortion cases were recorded in the Tula region for over 15 years. The frequency of abortion was reduced 4-fold, with 18,200 in 2001 to 4,538 in 2015. The rate of abortions per 1,000 women (age 15-44 years) for 15 years decreased by 40.5%, that is, from 46.53 (2001) to 18.84 (2015), and that of abortions per 100 live births and stillbirths was 29.5%, that is, from 161.7 (2001) to 41.5 (2015). Five women died from abortion complications that began outside of the hospital, which accounted for 0.01% of the total number. In the structure of causes of maternal mortality for 15 years, abortion represented 14.3% of the cases. Lethality mainly occurred in the period from 2001 to 2005 (4 cases). Among thematernal deaths, many women died in rural areas after pregnancy termination at 18 to 20 weeks of gestation (n = 4). In addition, three women died from sepsis and two from bleeding.
Conclusion
The introduction of modern, effective technologies of family planning has reduced maternal mortality due to abortion.


