Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2021;43(10):789-792
Abnormal uterine bleeding is more frequent in adolescence. Although, most commonly, it has a non-structural etiology, it may be due to any cause described.
A 12-year-old adolescent, with no relevant personal history, menarche 1 month before, was observed in the emergency department for severemenstrual bleeding with progressive worsening, and hemodynamic repercussion in need of transfusion support. Physiological ovulatory dysfunction associated with possible previously unknown coagulopathy was considered to be the most likely diagnosis and medical treatment was initiated. Without response, the patient was submitted to sedated observation and uterine aspiration, which ultimately led to the diagnosis of a Burkitt Lymphoma.
Although structural causes, and particularly malignancy, whether gynecological or not, are a rare cause of abnormal uterine bleeding in this age group, they must be considered, thus enhancing the fastest and most appropriate treatment.

Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2017;39(7):358-368
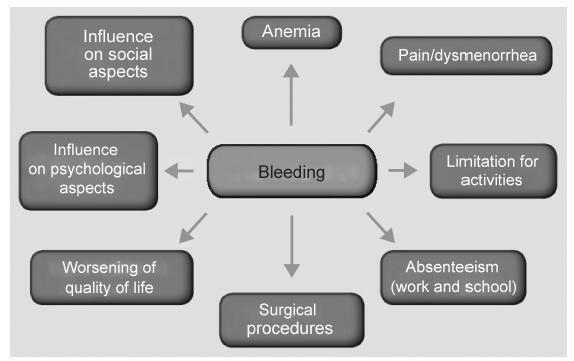
Abnormal uterine bleeding is a frequent condition in Gynecology. It may impact physical, emotional sexual and professional aspects of the lives of women, impairing their quality of life. In cases of acute and severe bleeding, women may need urgent treatment with volumetric replacement and prescription of hemostatic substances. In some specific cases with more intense and prolonged bleeding, surgical treatment may be necessary. The objective of this chapter is to describe the main evidence on the treatment of women with abnormaluterinebleeding, both acuteand chronic.Didactically,thetreatmentoptions were based on the current International Federation of Gynecology and Obstetrics (FIGO) classification system (PALM-COEIN). The etiologies of PALM-COEIN are: uterine Polyp (P), Adenomyosis (A), Leiomyoma (L), precursor and Malignant lesions of the uterine body (M), Coagulopathies (C), Ovulatory dysfunction (O), Endometrial dysfunction (E), Iatrogenic (I), and Not yet classified (N). The articles were selected according to the recommendation grades of the PubMed, Cochrane and Embase databases, and those in which the main objective was the reduction of uterine menstrual bleeding were included. Only studies written in English were included. All editorial or complete papers that were not consistent with abnormal uterine bleeding, or studies in animal models, were excluded. The main objective of the treatment is the reduction of menstrual flow and morbidity and the improvement of quality of life. It is important to emphasize that the treatment in the acute phase aims to hemodynamically stabilize the patient and stop excessive bleeding, while the treatment in the chronic phase is based on correcting menstrual dysfunction according to its etiology and clinical manifestations. The treatment may be surgical or pharmacological, and thelatterisbasedmainlyonhormonaltherapy,anti-inflammatorydrugsandantifibrinolytics.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2001;23(6):371-376
DOI 10.1590/S0100-72032001000600005
Purpose: to evaluate the results of the first 104 hysteroscopic polypectomies in a teaching hospital. Methods: a retrospective descriptive study was designed. Medical records of the first 136 operative hysteroscopies - 104 of which polypectomies - were reviewed. Patient characteristics such as age, parity, period of reproductive function and symptoms; number and size of polyps and results concerning complications and symptom relief were evaluated. Results: the average age of patients was 52.7 years. Three quarters of them were multiparous. Fifty-seven percent of the patients were menopaused. About half of the patients had symptoms related to polyps. Abnormal bleeding was the most frequent symptom (47.1%). In 16.3% of the patients more than 1 polyp were detected and 84% of the polyps were larger than 1 cm. The only immediate complication was a uterine perforation. Late complications were rare and mild. The follow-up period was 9 months on average. In 82% of teh patients the symptoms were controlled. Hysterectomy was necessary in 8.2% of the patients, all of them with other uterine diseases such as leiomyomas, adenomyosis and atypical endometrial hyperplasia in one patient). Conclusion: hysteroscopic polypectomy is a simple, safe and effective method for the treatment of endometrial polyps. Selection of patients must be rigorous to avoid further operative procedures.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2001;23(7):445-448
DOI 10.1590/S0100-72032001000700006
Purpose: to evaluate the results of 64 hysteroscopic endometrial ablations using a resectoscope in women with abnormal uterine bleeding of benign etiology and nonresponsive to clinical measures and to describe the failures and their associated conditions. Methods: sixty-four patients with abnormal uterine bleeding were submitted to the intervention between April 1994 and February 2000. The mean age was 42.9 years and the mean parity, 2.6 deliveries. Diagnostic hysteroscopy and endometrial biopsy were performed preoperatively. Before surgery, two women received gestrinone, six danazol and 44 GnRH analogue. During the surgery electric cauterization of the fundus uteri and cornual regions was made. Afterwards, with a resectoscope, the endometrium was removed as far as 1 cm above the internal ostium, and as deep as 2 to 3 mm into the myometrium. The uterine distension was obtained with 1.5% glycine and since two years ago with 3% manitol. The average follow-up was 11.5 months. After six months of endometrial ablation, the patients with persistence of symptoms were submitted to hysterectomy. Results: amenorrhea occurred in 31.2% of the patients and hypomenorrhea in 45.3%. The abnormal bleeding was maintained in 23.5%. There was one uterine perforation during the dilatation of the cervix. Results were better in the higher age and parity ranges and in the women who received GnRH analogues (p=0.03). Where the method was not successful there was a statistically significant frequency of submucous myoma (p=0.04) and a nonsignificant increase of secretory endometrium (p=0.12). Conclusions: the method is useful for the management of abnormal uterine bleeding of benign etiology. Previous administration of GnRH analogue is recommended. We suggest a special follow-up for the younger, low parous women, and those with submucous myoma, because they are the group with the poorest results.