You searched for:"Edward Araujo Júnior"
We found (59) results for your search.Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2017;39(2):53-59
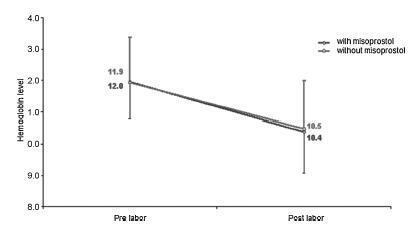
To evaluate blood loss during misoprostol-induced vaginal births and during cesarean sections after attempted misoprostol induction.
We conducted a prospective observational study in 101 pregnant women indicated for labor induction; pre- and postpartum hemoglobin levels were measured to estimate blood loss during delivery. Labor was induced by administering 25 μg vaginal misoprostol every 6 hours (with a maximum of 6 doses). The control group included 30 patients who spontaneously entered labor, and 30 patients who underwent elective cesarean section. Pre- and postpartum hemoglobin levels were evaluated using the analysis of variance for repeated measurements, showing the effects of time (pre- and postpartum) and of the group (with and withoutmisoprostol administration).
Therewere significant differences between pre- and postpartum hemoglobin levels (p < 0.0001) with regard to misoprostol-induced vaginal deliveries (1.6 ± 1.4 mg/dL), non-induced vaginal deliveries (1.4 ± 1.0 mg/dL), cesarean sections after attempted misoprostol induction (1.5 ± 1.0 mg/dL), and elective cesarean deliveries (1.8 ± 1.1 mg/dL). However, the differences were proportional between the groups with and without misoprostol administration, for both cesarean (p = 0.6845) and vaginal deliveries (p = 0.2694).
Labor induction using misoprostol did not affect blood loss during delivery.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2010;32(12):573-578
DOI 10.1590/S0100-72032010001200002
PURPOSE: to establish reference values for the length and area of the fetal corpus callosum between the 20th and 33rd weeks of gestation using three-dimensional ultrasound (3DUS). METHODS: this cross-sectional study involved 70 normal pregnancies with gestational age between 20 and 33 weeks. An Accuvix XQ instrument with a convex volumetric transducer (3 to 5 MHz) was used. To assess the corpus callosum, a transfrontal plane was obtained using the metopic suture as an acoustic window. Length was obtained by measuring the distance between the proximal and distal extremities of the corpus callosum. Area was obtained by manual tracing of the external corpus callosum surface. The means, medians, standard deviations, and maximum and minimum values were calculated for the corpus callosum length and area. Scatter graphs were created to analyze the correlation between corpus callosum length and area and gestational age and biparietal diameter, the quality adjustments was verified according to the determination coefficient (R²). The intraclass correlation coefficient (ICC) was used to assess the intraobserver variability. RESULTS: mean corpus callosum length increased from 21.7 (18.6 - 25.2 mm) to 38.7 mm (32.6 - 43.3 mm) between 20 and 33 weeks of pregnancy, respectively. Mean corpus callosum area increased from 55.2 (41.0 - 80.0 mm²) to 142.2 mm² (114.0 - 160.0 mm²), between 20 to 33 weeks of pregnancy, respectively. There was a strong correlation between corpus callosum length and area and gestational age (R² = 0.7 and 0.7, respectively) and biparietal diameter (R² = 0.7 and 0.6, respectively). Intraobserver variability was appropriate, with an ICC of 0.9 and 0.9 for length and area, respectively. CONCLUSIONS: reference values for corpus callosum length and area were established for fetuses between 20 and 33 weeks gestation. Intraobserver variability was appropriate.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2017;39(12):647-652
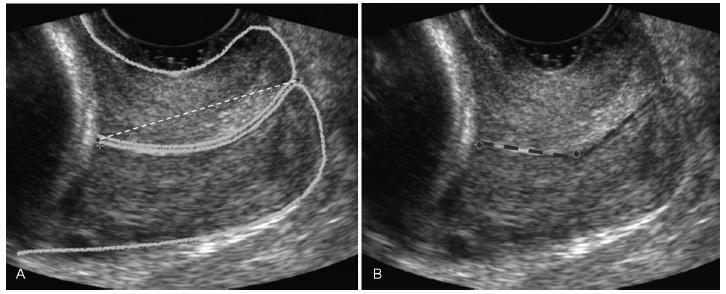
To determine cervical biometry in pregnant women between 18 and 24 weeks of gestation and the ideal mode of measurement of cervical length in cases of curved and straight cervical morphology.
The uterine cervices of 752 low-risk pregnant women were assessed using transvaginal ultrasound in a prospective cross-sectional study. In women with straight uterine cervices, cervical biometry was performed in a continuous manner. In women with curved uterine cervices, the biometry was performed using both the continuous and segmented techniques (in segments joining the cervical os). Polynomial regression models were created to assess the correlation between the cervical length and gestational age. The paired Student t-test was used to comparemeasuring techniques.
The cervical biometry results did not vary significantly with the gestational age and were best represented by linear regression (R2 = 0.0075 with the continuous technique, and R2 = 0.0017 with the segmented technique). Up to the 21st week of gestation, there was a predominance of curved uterine cervix morphology (58.9%), whereas the straight morphology predominated after this gestational age (54.2%). There was a significant difference between the continuous and the segmented measuring methods in all the assessed gestational ages (p < 0.001).
Cervical biometry in pregnant women between 18 and 24 weeks was represented by a linear regression, independently of the measuring mode. The ideal measuring technique was the transvaginal ultrasound performed at a gestational age 21 weeks.
Summary
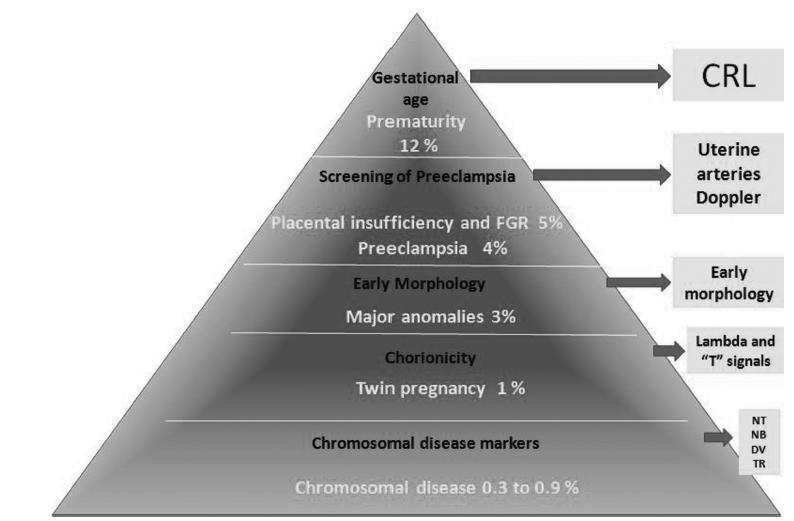
Revista Brasileira de Ginecologia e Obstetrícia. 2018;40(10):650-651
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2019;41(12):688-696
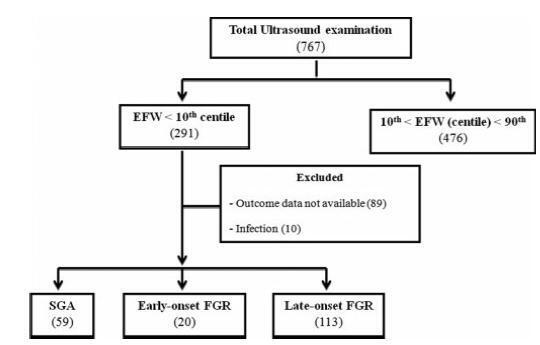
To evaluate the association between early-onset fetal growth restriction (FGR), late-onset FGR, small for gestational age (SGA) and adequate for gestational age (AGA) fetuses and adverse perinatal outcomes.
This was a retrospective longitudinal study in which 4 groups were evaluated: 1 - early-onset FGR (before 32 weeks) (n=20), 2 - late-onset FGR (at or after 32 weeks) (n=113), 3 - SGA (n=59), 4 - AGA (n=476). The Kaplan-Meier curve was used to compare the time from the diagnosis of FGR to birth. Logistic regression was used to determine the best predictors of adverse perinatal outcomes in fetuses with FGR and SGA.
A longer timebetween the diagnosis and birthwas observed forAGAthan for late FGR fetuses (p<0.001). The model including the type of FGR and the gestational age at birth was significant in predicting the risk of hospitalization in the neonatal intensive care unit (ICU) (p<0.001). The model including only the type of FGR predicted the risk of needing neonatal resuscitation (p<0.001), of respiratory distress (p<0.001), and of birth at<32, 34, and 37 weeks of gestation, respectively (p<0.001).
Fetal growth restriction and SGA were associated with adverse perinatal outcomes. The type of FGR at the moment of diagnosis was an independent variable to predict respiratory distress and the need for neonatal resuscitation. The model including both the type of FGR and the gestational age at birth predicted the risk of needing neonatal ICU hospitalization.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2020;42(11):717-725
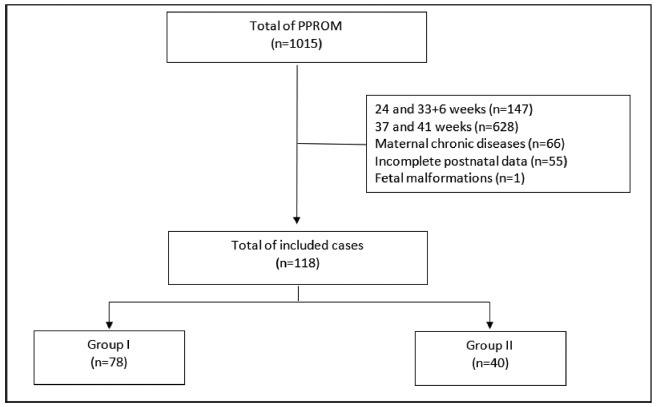
To compare the type of management (active versus expectant) for preterm premature rupture of membranes (PPROM) between 34 and 36 + 6 weeks of gestation and the associated adverse perinatal outcomes in 2 tertiary hospitals in the southeast of Brazil.
In the present retrospective cohort study, data were obtained by reviewing the medical records of patients admitted to two tertiary centers with different protocols for PPROM management. The participants were divided into two groups based on PPROM management: group I (active) and group II (expectant). For statistical analysis, the Student t-test, the chi-squared test, and binary logistic regression were used.
Of the 118 participants included, 78 underwent active (group I) and 40 expectant management (group II). Compared with group II, group I had significantly lower mean amniotic fluid index (5.5 versus 11.3 cm, p = 0.002), polymerase chain reaction at admission (1.5 versus 5.2 mg/dl, p = 0.002), time of prophylactic antibiotics (5.4 versus 18.4 hours, p < 0.001), latency time (20.9 versus 33.6 hours, p = 0.001), and gestational age at delivery (36.5 versus 37.2 weeks, p = 0.025). There were no significant associations between the groups and the presence of adverse perinatal outcomes. Gestational age at diagnosis was the only significant predictor of adverse composite outcome (x2 [1] = 3.1, p = 0.0001, R2 Nagelkerke = 0.138).
There was no association between active versus expectant management in pregnant women with PPROM between 34 and 36 + 6 weeks of gestation and adverse perinatal outcomes.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2021;43(1):72-73
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2020;42(2):74-80
To evaluate the impact of the presence of criteria for severe maternal morbidity and maternal near miss associated with hypertensive disorders on maternal and perinatal outcomes in a maternity school.
The present is a sub-analysis of a larger study involving 27 centers in Brazil that estimated the prevalence of serious maternal morbidity and near miss. It is an analytical and cross-sectional study with a quantitative approach, involving 928 women who were cared for at Maternidade Escola Assis Chateaubriand (MEAC, in Portuguese), Universidade Federal do Ceará (UFC, in Portuguese), from July 2009 to June 2010. The women were diagnosed with near miss according to the World Health Organization (WHO) criteria. The sample was divided into 2 groups: patients with (n = 827) and without hypertension (n = 101). The results were considered statistically significant when p < 0.05. The Pearson chi-squared and Fisher Exact tests were used for the categorical variables, and the Mann–Whitney U test was used for the continuous variables.
In total, 51 participants with maternal near miss criteria were identified, and 36 of them had hypertensive disorders. Of these, 5 died and were obviously excluded from the near miss final group. In contrast, we observed 867 cases with non-near miss maternal morbidity criteria. During this period, there were 4,617 live births (LBs) in the institution that was studied.
In the severe morbidity/maternal near miss population, the presence of hypertensive complications was prevalent, constituting a risk factor for both the mother and the fetus.