You searched for:"Mary Angela Parpinelli"
We found (26) results for your search.Summary
Revista Brasileira de Ginecologia e Obstetrícia. 1999;21(9):519-525
DOI 10.1590/S0100-72031999000900004
Purpose: to present the perinatal outcomes resulting from the use of a protocol for assistance to diabetic pregnant women used at the Center for Integral Assistance to Women's Health (CAISM), of the University of Campinas. Methods: ninety diabetic pregnant women, who were assisted at the institution with this protocol, were compared with two control grups: the first consisted of 180 pregnant women with equal number of gestations and same age (control A) and the second consisted of 180 randomly selected pregnant women (control B). The study variables were route of delivery, indication for cesarean section, gestational age, Apgar score at first and fifth minute, weight, adequacy of weight for gestational age and perinatal morbidity and mortality. For the statistical analysis Student's t-test and the chi2 test were used. Results: there was a higher incidence of cesarean sections, prematures and large to gestational age (LGA) babies among diabetic women, as well as higher occurrence of neonatal morbidity such as hypoglycemia, hypocalcemia, hyperbilirubinemia, respiratory distress and neonatal depression. The incidence of low Apgar score and perinatal mortality was significantly higher than in the randomly selected group, but the same as in the group matched regarding age and number of pregnancies. Conclusions: although this protocol intends to obtain a perfect metabolic control among diabetic pregnant women, the perinatal outcomes are still unfavorable in comparison to nondiabetic pregnant women.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2004;26(7):579-582
DOI 10.1590/S0100-72032004000700011
Paroxysmal nocturnal hemoglobinuria is a rare disease caused by an acquired gene mutation of the hematopoietic system, with 16-18% of the cases diagnosed during pregnancy. We describe two cases of pregnancy in women with paroxysmal nocturnal hemoglobinuria. Maternal mortality reaches 8-10%, mainly due to thromboembolism and, less frequently, to leukemic transformation. Fetal losses may reach 30%. These two cases illustrate a serious and extremely complex situation, which is the obstetrical management of a patient with a very rare, serious and potentially fatal hematological condition. Using a multidisciplinary approach in tertiary care centers, it is possible to attain good maternal and perinatal outcomes.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 1999;21(10):579-584
DOI 10.1590/S0100-72031999001000003
Purpose: to evaluate the accuracy of maternal perception of fetal movements (MPFM) in diabetic pregnant women, using Apgar score at the 1st and 5th min of life, intrapartum fetal distress and neonatal hypoxia as parameters. Methods: two hundred and nine diabetic women evaluated at the High Risk Prenatal Care Clinic of the Women's Hospital (CAISM) were analyzed retrospectively between June 1988 and May 1996. All patients had MPFM records within three days before delivery, fetal heart rate recordings during labor, gestational age greater than 30 weeks and a complete neonatal evaluation. MPFM was classified as normal if seven movements were recorded in 60 min. Results: the sensitivity of the test was 23 and 29% for Apgar score <7 at the 5th min and intrapartum fetal distress, respectively, and close to 50% for neonatal hypoxia (45.5%). Specificity was near 95% for the three standards, and the negative predictive value (NPV) was 80% for fetal distress, increasing to 97 and 98% for Apgar >7 at 5 min and neonatal hypoxia. Conclusions: MPFM is a useful test to identify diabetic women needing fetal evaluation with more complex techniques, given the high NPV, that indicates the capacity to separate the cases where the fetus is in good condition.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2000;22(9):579-584
DOI 10.1590/S0100-72032000000900007
Purpose: to evaluate the avoidable mortality among women in reproductive age, living in Campinas, SP, comparing two five-year periods: 1985-89 and 1990-94. Methods: death certificates of 3.086 women aged 10 to 49 years were studied, representing the total number of deaths during the period from January 1985 through December 1994. The criteria for avoidance were applied to these deaths using preventive, sanitary, early diagnosis and treatment, and mixed measures. The deaths were also classified as: with hardly avoidable causes, not well-defined causes and other causes. The specific mortality coefficient for each period of five years and the ratio between these coefficients were calculated. Results: there was a 20% increase in the avoidable mortality rate from the first to the second period. The main failure was observed among the group of avoidable causes by preventive and sanitary measures. The main increase in death causes by preventive measures resulted from AIDS. Among the causes of death avoidable by mixed measures, the increase of 50% in maternal mortality caused by abortion, as well as causes due to violence specially homicides, are emphasized. Conclusion: there was an increase in the proportion of avoidable death causes. Measures to prevent AIDS, abortion and to reduce violent deaths, specially homicides, should be political and social priorities in our Country.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2017;39(11):622-631
Preeclampsia, a multifactorial disease with pathophysiology not yet fully understood, is a major cause of maternal and perinatal morbidity and mortality, especially when preterm. The diagnosis is performed when there is an association between arterial hypertension and proteinuria or evidence of severity. There are unanswered questions in the literature considering the timing of delivery once preterm preeclampsia has been diagnosed, given the risk of developingmaternal complications versus the risk of adverse perinatal outcomes associated with prematurity. The objective of this systematic review is to determine the best timing of delivery for women diagnosed with preeclampsia before 37 weeks of gestation.
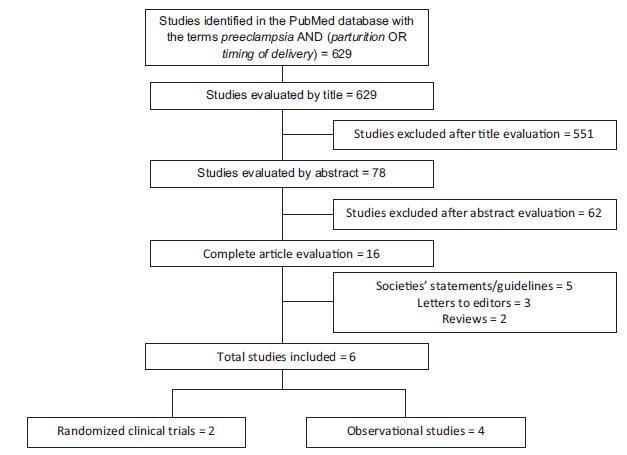
Systematic literature review, performed in the PubMed database, using the terms preeclampsia, parturition and timing of delivery to look for studies conducted between 2014 and 2017. Studies that compared the maternal and perinatal outcomes of women who underwent immediate delivery or delayed delivery, in the absence of evidence of severe preeclampsia, were selected.
A total of 629 studies were initially retrieved. After reading the titles, 78 were selected, and their abstracts, evaluated; 16 were then evaluated in full and, in the end, 6 studies (2 randomized clinical trials and 4 observational studies) met the inclusion criteria. The results were presented according to gestational age range (< 34 weeks and between 34 and 37 weeks) and by maternal and perinatal outcomes, according to the timing of delivery, considering immediate delivery or expectant management. Before 34 weeks, thematernal outcomeswere similar, but the perinatal outcomes were significantly worse when immediate delivery occurred. Between 34 and 37 weeks, the progression to severe maternal disease was slightly higher among women undergoing expectant management, however, with better perinatal outcomes.
When there is no evidence of severe preeclampsia or impaired fetal wellbeing, especially before 34 weeks, the pregnancy should be carefully surveilled, and the delivery, postponed, aiming at improving the perinatal outcomes. Between 34 and 37 weeks, the decision on the timing of delivery should be shared with the pregnant woman and her family, after providing information regarding the risks of adverse outcomes associated with preeclampsia and prematurity.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2005;27(10):627-634
DOI 10.1590/S0100-72032005001000010
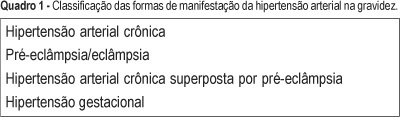
Arterial hypertension is one of the most frequent causes of maternal death. The most important types found in pregnancy are gestational hypertension, clinically defined by increased arterial pressure after the 20th week of pregnancy, and preeclampsia associated with proteinuria. In the initial phase, the disease is asymptomatic, but when not treated or when the pregnancy is not interrupted, it naturally progresses to serious forms such as eclampsia and HELLP syndrome. Eclampsia is defined by one or more generalized tonic-clonic seizures or coma in a pregnant woman with gestational hypertension or preeclampsia, and without neurological disease. It may occur during pregnancy, labor, and immediately after delivery. It is often preceded by signs and symptoms of imminent eclampsia (central nervous system, visual and gastric disorders). Its association with hemolysis, low platelet count, and hepatic dysfunction had already been reported in the literature of the 1950's. In 1982, Weinstein grouped these alterations as a syndrome under the acronym of HELLP, meaning hemolysis (H), elevated liver enzyme levels (EL), and low platelet (LP) count. The literature differs in relation to the parameter values that define the syndrome. Sibai et al. (1986) proposed a system of laboratory and biochemical diagnosis standards which has been adopted by the Brazilian Health Ministry. Clinical manifestations are sometimes imprecise; common complaints are epigastric pain, general malaise, loss of appetite, nausea, and vomiting. Early diagnosis is exclusively by laboratory tests and should be systematically investigated in women with serious preeclampsia/eclampsia or pain in the superior right abdominal quadrant. Differentiating HELLP syndrome from others with similar clinical or laboratory manifestations is not easy. Differential diagnosis is particularly difficult regarding diseases such as thrombotic thrombocytopenic purpura, hemolytic-uremic syndrome, or acute fatty liver of pregnancy, due to poor clinical history, and similar physiopathological aspects. An understanding of preeclampsia physiopathology, early diagnosis, and precise action at the right moment in situations complicated by eclampsia or HELLP syndrome, allows a better maternal and perinatal prognosis.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2003;25(9):639-646
DOI 10.1590/S0100-72032003000900004
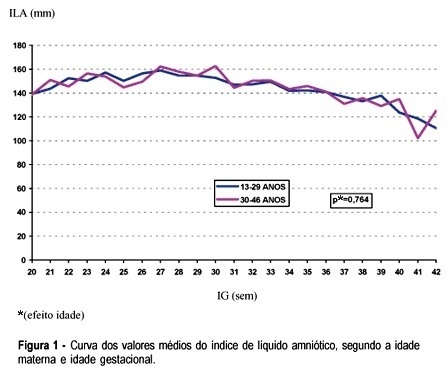
PURPOSE: to evaluate the association between the variability of amniotic fluid index (AFI) values with gestational age and some sociodemographic and obstetric variables among low-risk pregnant women. METHOD: a comparative study was carried out including 2868 low-risk pregnant women who had routine obstetric ultrasound examination, including fetal biometry and the measurement of AFI, from 20 to 42 weeks of gestation. The data were analyzed using Student's t test, analysis of variance of mean AFI values along gestational ages, according to other control variables, and also by multiple linear regression analysis. RESULTS: there was no significant variation of mean AFI values during the time of pregnancy neither when separately evaluating its association with maternal age, color, education, smoking habit, parity, and the presence of previous cesarean section scars, nor when the evaluation was performed through multivariate analysis. In this situation only the increase in gestational age showed to be associated with the decrease of AFI. Generally speaking, the mean AFI values fluctuated between 140 and 180 mm between the 20th and the 36th week, then showing values below 140 mm in a progressive decrease after this limit of gestational age. CONCLUSIONS: AFI values do not show a significant variation during pregnancy regarding the studied sociodemographic and obstetric variables.