You searched for:"Carlos Augusto Alencar Júnior"
We found (20) results for your search.Summary
Rev Bras Ginecol Obstet. 2017;39(2):53-59
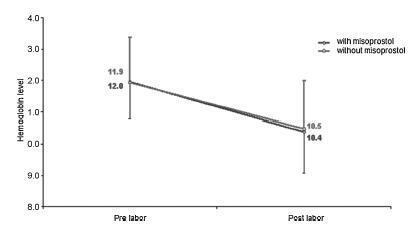
To evaluate blood loss during misoprostol-induced vaginal births and during cesarean sections after attempted misoprostol induction.
We conducted a prospective observational study in 101 pregnant women indicated for labor induction; pre- and postpartum hemoglobin levels were measured to estimate blood loss during delivery. Labor was induced by administering 25 μg vaginal misoprostol every 6 hours (with a maximum of 6 doses). The control group included 30 patients who spontaneously entered labor, and 30 patients who underwent elective cesarean section. Pre- and postpartum hemoglobin levels were evaluated using the analysis of variance for repeated measurements, showing the effects of time (pre- and postpartum) and of the group (with and withoutmisoprostol administration).
Therewere significant differences between pre- and postpartum hemoglobin levels (p < 0.0001) with regard to misoprostol-induced vaginal deliveries (1.6 ± 1.4 mg/dL), non-induced vaginal deliveries (1.4 ± 1.0 mg/dL), cesarean sections after attempted misoprostol induction (1.5 ± 1.0 mg/dL), and elective cesarean deliveries (1.8 ± 1.1 mg/dL). However, the differences were proportional between the groups with and without misoprostol administration, for both cesarean (p = 0.6845) and vaginal deliveries (p = 0.2694).
Labor induction using misoprostol did not affect blood loss during delivery.
Summary
Rev Bras Ginecol Obstet. 2004;26(7):535-541
DOI 10.1590/S0100-72032004000700005
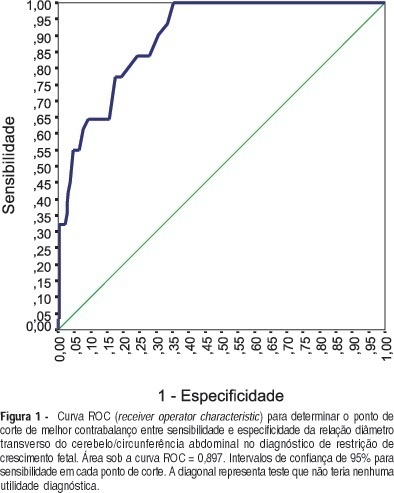
PURPOSE: to evaluate the validity of transverse cerebellar diameter (TCD)/abdominal circumference (AC) ratio in the diagnosis of fetal growth restriction (FGR), determining its best cutoff value and accuracy in symmetric and asymmetric FGR. METHOD: a prospective cross-sectional study, carried out in 250 pregnant women with singleton pregnancies, gestational age between 20 and 42 weeks, with ultrasound confirmation. The TCD measurement was obtained by placing the calipers at the outer margins of the cerebellum, after its localization in the posterior fossa, and slightly rotating the transducer below the plane of the thalami. The abdominal circumference was measured at the on junction of the left portal and umbilical veins. The best TCD/AC cutoff ratio was established by the receiver operator characteristic (ROC) curve. Neonates with TCD/AC ratio greater than the cutoff value were diagnosed as having FGR. We classified as gold standard for FGR the newborn infants who presented birth weight below the 10th percentile. Neonates showing FGR and Rohrer ponderal index between 2.2 and 3 were labeled as symmetric and below 2.2, asymmetric. RESULTS: the cutoff value calculated by the ROC curve for TCD/AC ratio was 16.15. The sensitivity, specificity, accuracy, positive and negative predictive values, and likelihood ratio for positive and negative tests were 77.4, 82.6, 38.7, 96.3, 82, 4.5 and 3.7%, respectively. In the symmetric FGR, sensitivity and specificity were 80.8 and 81.7%, respectively. In the asymmetric FGR, sensitivity and specificity were 60 and 75%, respectively. CONCLUSION: TCD/AC ratio is an effective method in symmetric and asymmetric FGR diagnosis.
Summary
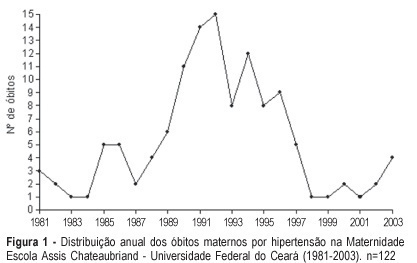
Rev Bras Ginecol Obstet. 2005;27(9):548-553
DOI 10.1590/S0100-72032005000900008
PURPOSE: to study maternal mortality caused by hypertension during pregnancy, determining the mortality rate and the profile of those patients. METHODS: a retrospective study of maternal mortality caused by hypertension at the Maternidade Escola Assis Chateaubriand of the Universidade Federal do Ceará, from 1981 to 2003. General maternal mortality rate (MMR) and specific maternal mortality rate due to hypertension were evaluated, as well as these patients' epidemiological and clinical data. RESULTS: two hundred and ninety six cases of maternal death and 184,672 of live births were recorded, with a MMR of 160.28/100.000 live births. The most frequent cause of death was hypertension (41.2%); with 122 cases and an annual average of 5.3 deaths, and hypertension MMR of 60.10/100,000 live births. The women's age range varied from 13 to 42 years with an average of 26 years. Most of the patients came from the interior of the state. Deaths occurred predominantly in the first 24 hours after admission to the hospital (50.9%). Deaths were predominant in the first pregnancy (40.3%) and in women with 31 to 38 weeks gestational age (48.2%). Eclampsia occurred in 73 patients (64.1%) and was predominant along the gestational period (53.4%). There were 101 deaths in the puerperium. Cesarean section (62.3%) and general anesthesia (45.1%) prevailed. A high percentage of patients (61.4%) had no prenatal care. CONCLUSIONS: General MMR and hypertension MMR were high, the latter being the main cause of death in our maternity hospital.
Summary
Rev Bras Ginecol Obstet. 2007;29(12):639-646
DOI 10.1590/S0100-72032007001200007
PURPOSE: to compare the effectiveness of low doses of vaginal misoprostol (12.5 versus 25 µg) for induction of labor. METHODS: a double-blind, randomized, controlled clinical trial was performed in Santa Casa de Misericórdia de Sobral, from May 2005 to April 2006. Sixty-two term pregnant women, with intact membranes and with indication for labor induction, were included. They randomly received 25 µg (32) or 12.5 µg (30) of vaginal misoprostol each four hours, until the maximum of eight doses. Mode of delivery, time between induction and delivery, perinatal complications, and maternal side effects were studied. The control variables were maternal and gestational ages, parity and Bishop score. The statistical tests used were average calculations, shunting line-standards and Student t-test (numerical continuous variables), chi2 (categorical variables) and Mann-Whitney test (discrete variables). RESULTS: the two groups, 12.5 and 25 µg, did not differ in relation to the interval of time between the induction onset and delivery (1524 versus 1212 min, p=0.333), in the frequency of vaginal delivery (70 versus 71.8%, p=0.720), Apgar scores below seven at the fifth minute (3,3 versus 6,25%, p=0.533) and tachysystole frequency (3.3 versus 9.3%, p=0.533). The average of total dose administered was significantly higher in the 25 µg group (40 versus 61.2 µg, p=0.03). CONCLUSIONS: vaginal misoprostol in the dose of 12.5 µg was efficient, with collateral effects similar, to the 25 µg of vaginal misoprostol, for induction of labor at term.