You searched for:"Wellington de Paula Martins"
We found (15) results for your search.Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2016;38(9):436-442
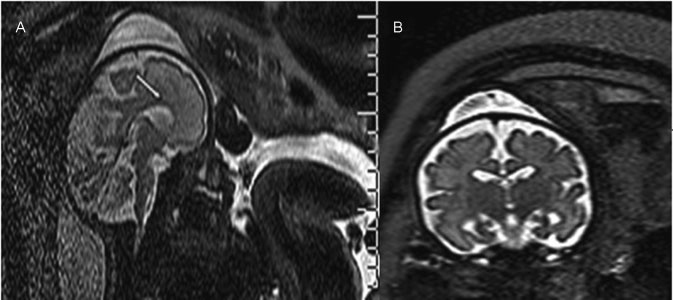
Ventriculomegaly (VM) is one the most frequent anomalies detected on prenatal ultrasound. Magnetic resonance imaging (MRI) may enhance diagnostic accuracy and prediction of developmental outcome in newborns.
The aim of this study was to assess the correlation between ultrasound and MRI in fetuses with isolated mild and moderate VM. The secondary aim was to report the neurodevelopmental outcome at 4 years of age.
Fetuses with a prenatal ultrasound (brain scan) diagnosis of VM were identified over a 4-year period. Ventriculomegaly was defined as an atrial width of 10- 15 mm that was further divided as mild (10.1-12.0 mm) and moderate (12.1-15.0 mm). Fetuses with VM underwent antenatal as well as postnatal follow-ups by brain scan and MRI. Neurodevelopmental outcome was performed using the Griffiths Mental Development Scales and conducted, where indicated, until 4 years into the postnatal period.
Sixty-two fetuses were identified. Ventriculomegaly was bilateral in 58% of cases. A stable dilatation was seen in 45% of cases, progression was seen in 13%, and regression of VM was seen in 4.5% respectively. Fetal MRI was performed in 54 fetuses and was concordant with brain scan findings in 85% of cases. Abnormal neurodevelopmental outcomes were seen in 9.6% of cases.
Fetuses in whom a progression of VM is seen are at a higher risk of developing an abnormal neurodevelopmental outcome. Although brain scan and MRI are substantially in agreement in defining the grade of ventricular dilatation, a low correlation was seen in the evaluation of VM associated with central nervous system (CNS) or non-CNS abnormalities.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2010;32(9):447-453
DOI 10.1590/S0100-72032010000900006
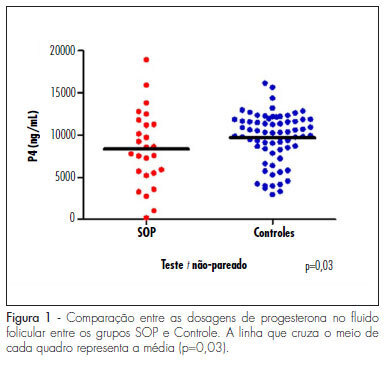
PURPOSE: to evaluate the concentration of steroid hormones in follicular fluid (FF) of small (10-14 mm) and large (> 18 mm) follicles of women with polycystic ovary syndrome (PCOS) submitted to controlled ovarian hyperstimulation (COH) and in vitro fertilization (IVF) cycles. METHODS: a case-control study was conducted on 13 infertile women with PCOS (17 cycles) and 31 infertile women due to male factor - Control Group (31 cycles). FF was aspirated individually and divided into four groups: G1 (FF of small follicles of the Control Group), G2 (FF of small follicles of the PCOS group), G3 (FF of large follicles of the Control Group) and G4 (FF of large follicles of the PCOS group). Estrogen, progesterone and β-hCG were determined by chemiluminescence, and testosterone and androstenedione by radioimmunoassay. The unpaired t-test was used to compare the hormone determinations in the FF of the PCOS and Control Groups, and the four groups were compared by ANOVA. Fisher's exact test was used to compare the pregnancy rates. RESULTS: the small follicles of the two groups had lower progesterone levels (8,435±3,305 ng/mL) than large follicles (10,280±3,475 ng/mL), p-value <0.01. The progesterone levels of all follicles of group PCOS (8,095±4,151 ng/mL) were lower than Control (9,824±3,128 ng/mL), p-value =0.03. Testosterone differed between G1 (326.6±124.4 ng/dL) and G3 (205.8±98.91 ng/dL), p-value <0.001, and between G3 (205.8±98.91 ng/dL) and G4 (351.10±122.1ng/dL), p-value <0.001. Small follicles had higher testosterone levels (508.9±266 ng/dL) than large follicles (245.10±123 ng/dL), p-value <0.0001. The pregnancy rates did not differ between the PCOS (5/13, 38.5%) and the Control groups (9/31, 40.9%), p-value =072. CONCLUSIONS: women with PCOS had high testosterone concentrations in the FF, regardless of the stage of follicle development, and reduced progesterone levels, suggesting that paracrine factors may inhibit the secretion of the latter by follicular cells. The pregnancy rates showed that treatment with COH and IVF is a good option for women with infertility secondary to PCOS.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2016;38(9):465-470
Infertility has a high prevalence in the general population, affecting 5 to 15% of couples in reproductive age. The assisted reproduction techniques ( ART ) include in vitro manipulation of gametes and embryos and are an important treatment indicated to these couples. It is well accepted that the implantation rate is positively influenced by the morphology of transferred embryos. However, we question if, apart from the assessment of embryo morphology, the number of produced embryos per cycle is also related to pregnancy rates in the first fresh transfer cycle.
To evaluate the clinical pregnancy rate according to the number of formed embryos and the transfer of top quality embryos ( TQEs ).
In a retrospective cohort study, between January 2011 and December 2012 , we evaluated women who underwent intracytoplasmic sperm injection (ICSI), aged < 40 years, andwith at least 1 formed embryo fresh transferred in cleavagestage. These women were stratified into 3 groups according to the number of formed embryos (1 embryo, 2-3 and ≥ 4 embryos). Each group was divided into 2 subgroups according to the presence or not of at least 1 transferred TQE (1 with TQE; 1 without TQE; 2-3 with TQE, 2-3 without TQE; ≥4with TQE; ≥4withoutTQE). The clinicalpregnancy rateswerecomparedineach subgroup based on the presence or absence of at least one transferred TQE.
During the study period, 636 women had at least one embryo to be transferred in thefirst fresh cycle (17.8% had 1 formed embryo [32.7% with TQEversus 67.3% without TQE], 42.1% of women had 2-3 formed embryos [55.6% with TQE versus 44.4% without TQE], and 40.1%ofpatientshad ≥4 formedembryos[73.7%withTQEversus26.3%withoutTQE]).The clinical pregnancy rate was significantly higher in the subgroup with ≥4 formed embryos with at least 1 transfered TQE (45.2%) compared with the subgroup without TQE (28.4%).
Having at least two available embryos and at least one TQE for embryo transfer are predictors of the pregnancy rates.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2008;30(10):494-498
DOI 10.1590/S0100-72032008001000003
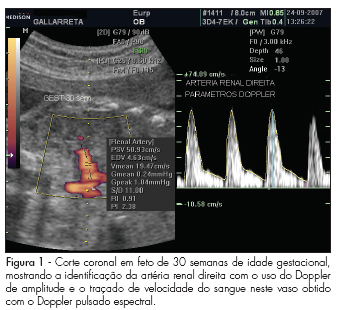
PURPOSE: to describe values found for the resistance index (RI), pulsatility index (PI) and the systole/diastole (S/D) ratio of fetal renal arteries in non-complicated gestations between the 22nd and the 38th week, and to evaluate whether those values vary along that period. METHODS: observational study, where 45 fetuses from non-complicated gestations have been evaluated in the 22nd, 26th, 30th and 38th weeks of gestational age. Doppler ultrasonography has been performed by the same observer, using a device with 4 to 7 MHz transducer. For the acquisition of the renal arteries velocity record, a 1 mm to 2 mm probe has been placed in the mean third of the renal artery for the evaluation through pulsed Doppler ultrasonography. The measurement of RI, PI and S/D ratio from three consecutive waves was performed with the automatic mode. To detect significant differences in the indexes' values along gestation, we have compared values obtained at the different gestational ages, through repeated measures ANOVA, followed by Tukey's post-hoc test. RESULTS: There were no significant differences between the right and left renal arteries, when the RI, IP and S/D ratio were compared. Nevertheless, a change in the values of these parameters has been observed between the 22nd week (RI=0.9 ± 0.02; PI=2.4 ± 0.02; S/D ratio=11.6 ± 2.2; mean ± standard deviation of the combined mean values of the right and left renal artery) and the 38th week (RI=0.8 ± 0.03; PI=2.1 ± 0.2; S/D ratio=8.7 ± 2.3) of gestation. CONCLUSIONS: the parameters evaluated (RI, PI and S/D ratio) have presented decreasing values between the 22nd and 38th, with no difference between the fetus's right and left sides.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2017;39(10):523-528
To assess cases of labor induction with vaginal 25-μg tablets of misoprostol and maternal outcomes in a tertiary hospital in southeastern Brazil.
This was a retrospective cohort study of 412 pregnant women with indication for labor induction. Labor induction was performed with vaginal 25-μg tablets ofmisoprostol in pregnant women with Bishop scores < 6. Stepwise regression analysis was used to identify the factors present at the beginning of induction that could be used as predictors of successful labor induction.
A total of 69% of the pregnant women who underwent labor induction progressed to vaginal delivery, and 31% of the women progressed to cesarean section. One or two misoprostol tablets were used in 244 patients (59.2%). Of the 412 patients, 197 (47.8%) required oxytocin later on in the labor process, after induction with misoprostol. The stepwise regression analysis showed that only Bishop scores of 4 and 5 and previous vaginal delivery were independent factors with statistical significance in the prediction of successful vaginal labor induction (β = 0.23, p < 0.001, for a Bishop score of 4 and 5, and β = 0.22, p < 0.001, for previous vaginal delivery).
Higher Bishop scores and previous vaginal delivery were the best predictors of successful labor induction with vaginal 25-μg tablets of misoprostol.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2016;38(11):552-558
Whether preconception elevated concentrations of thyroid-stimulating hormone (TSH) compromises reproductive outcomes in patients undergoing assisted reproduction techniques (ARTs) remains unclear. This study therefore compared the reproductive outcomes in patients with TSH concentrations of < 2.5 mIU/L, 2.5-4.0 mIU/L, and 4.0-10.0mIU/L undergoing controlled ovarian stimulation (COS) for in vitro fertilization (IVF)/intracytoplasmic sperm injection (ICSI).
This retrospective cohort study evaluated the medical records of all women with measured TSH concentrations who underwent IVF/ICSI between January 2011 and December 2012. The patients were divided into three groups: TSH < 2.5mIU/L (group 1); THS ≥2.5 and < 4.0 mIU/L (group 2); and THS ≥4 mIU/L and < 10.0 mIU/L (group 3). Patients who were administered levothyroxine for treating hypothyroidism were excluded from the analysis. The primary endpoints were clinical pregnancy,miscarriage, live birth and multiple pregnancy rates.
During the study period, 787 women underwent IVF/ICSI. Sixty were excluded because their TSH concentrations were unavailable, and 77 were excluded due to their use of levothyroxine. The prevalence of patients presenting elevated concentrations of TSHwas of 5.07% (using a TSH threshold of 4.0 mIU/L) and of 29.99% (using a TSH threshold of 2.5 mIU/L). Patient characteristics, type of COS, and response to COS did not differ among the three groups, and there were no differences in clinical pregnancy (24.4% versus 25.9% versus 24.2%, p = 0.93); miscarriage (17.1% versus 14.3% versus 12.5%, p = 0.93); live birth (20.2% versus 22.2% versus 21.2%, p = 0.86); and multiple pregnancy rates (27.0% versus 21.4% versus 25.0%, p = 0.90) respectively.
Response to COS, live birth, and miscarriage rates were not altered in women with elevated concentrations of TSH undergoing IVF/ICSI, regardless of using a TSH threshold of 2.5mIU/L or 4.0mIU/L. These findings reinforce the uncertainties related to the impact of subclinical hypothyroidism on reproductive outcomes in women undergoing COS for ARTs.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2006;28(12):715-720
DOI 10.1590/S0100-72032006001200005
PURPOSE: to investigate the effects of previous bilateral tubal sterilization on the outcome of in vitro fertilization. METHODS: retrospective study of 98 consecutive in vitro fertilization cycles. Fifty-five women with previous tubal sterilization without any other infertility factor (TL group) were compared with 43 women with infertility due only to mild male factor (MI group. Age, cancellation rate per induction cycle, response to ovulation induction (number of days of ovulation induction, total amount of gonadotrophin units used, number of follicles and oocytes retrieved), fertilization and cleavage rates, number of transferred embryos and clinical pregnancy per transfer cycle were the variables considered. RESULTS: the cycle discontinuation rate due to poor response, results of ovulation induction, fertilization and cleavage rates, number of transferred embryos and the occurrence of clinical pregnancy were similar in both groups. Considering solely the variable age in TL group, we observed that patients older than 35 years required higher gonadotrophin doses during ovulation induction (2445 versus 2122 IU), presented lower response with fewer follicular growth (11.3 versus 15.8) and less oocytes retrieved (6.1 versus 8.5) compared to younger women (34 years old or less). CONCLUSIONS: tubal sterilization did not interfere with in vitro fertilization outcomes. We observed a worse response to ovulation induction in women older than 35 years, who had previous tubal sterilization.