You searched for:"Marcos Dias de Moura"
We found (13) results for your search.Summary
Rev Bras Ginecol Obstet. 2005;27(2):64-68
DOI 10.1590/S0100-72032005000200004
PURPOSE: to determine the frequency of Mycoplasma hominis and Ureaplasma urealyticum infection, and relate it to the associated clinical variables of infertile women. METHODS: transversal study involving 322 infertile women, submitted to collection of endocervix swab for research of Mycoplasma hominis and Ureaplasma urealyticum infecction, from October 2002 to May 2004. All patients were submitted to a basic infertility investigation protocol. As control, a historical series of 51 non-pregnant women previously investigated as for the studied infectious agents, was used. RESULTS: the frequency of Mycoplasma hominis and Ureaplasma urealyticum infection was 4.9% in the infertile women and 13.8% in the control group. Among the infertile patients, a relationship between the presence of the two agents and changes in the histerosalpingography result (OR: 3.20; IC 95%: 1.05-9.73), presence of dyspareunia (OR: 10.72; IC 95%: 3.21-35.77) and vaginal discharge (OR: 8.5; IC 95%: 2.83-26.02), besides endocervical culture positive for Escherichia coli (OR: 6.09; IC 95%: 4.95-52.25) was observed. CONCLUSION: Mycoplasma hominis and Ureaplasma urealyticum infection rate is low in infertile patients and is associated with reproductive sequels.
Summary
Rev Bras Ginecol Obstet. 2006;28(11):643-651
DOI 10.1590/S0100-72032006001100003
PURPOSE: literature reports show that there are no conclusive data about the association between endometriosis and the concentrations of hormones involved in the control of reproduction. Thus, the present study was undertaken to determine FSH, LH, estradiol (E), progesterone (P), and histamine (Hi) concentrations in serum, peritoneal fluid and follicular fluid of women with and without endometriosis. METHODS: the extent of the disease was staged according to the revised American Fertility Society classification (1997). For the collection of serum and peritoneal fluid, 28 women with endometriosis undergoing diagnostic laparoscopy were selected (18 infertile women with endometriosis I-II and ten infertile women with endometriosis III-IV). For the control group, 21 fertile women undergoing laparoscopy for tubal sterilization were selected. Follicular fluid was obtained from 39 infertile women undergoing in vitro fertilization (21 women with endometriosis and 18 women without endometriosis). RESULTS: FSH and LH levels in serum, peritoneal fluid and follicular fluid did not differ significantly between groups. On the other hand, E and P concentrations in the peritoneal fluid were significantly lower in infertile women with endometriosis (E: 154.2±15.3 for stages I-II and 89.3 ng/mL±9.8 ng/mL for stages III-IV; P: 11.2±1.5 for stages I-II and 7.6 ng/mL±0.8 for stages III-IV) in comparison with control women (E: 289.1 ng/mL±30.1; P: 32.8±4.1 ng/mL) (Kruskal-Wallis/Dunn tests; p<0.05). In serum, estradiol and progesterone concentrations followed the same pattern. In the follicular fluid, E and Hi concentrations were significantly lower in women with endometriosis (E: 97.4±11.1 pg/mL; Hi: 6.6±0.9 ng/mL) in comparison to women without endometriosis (E: 237.5±28.5 pg/mL; Hi: 13.8±1.3 ng/mL) (Student t-test; p<0.05), while progesterone levels revealed no significant difference between groups. CONCLUSIONS: our results indicate ovary dysfunction in women with endometriosis, with reduction on E, P and Hi concentrations, which may contribute to the subfertility often associated with the disease.
Summary
Rev Bras Ginecol Obstet. 2004;26(9):727-733
DOI 10.1590/S0100-72032004000900009
PURPOSE: to evaluate the results of ovulation hyperinduction followed by in vitro fertilization (IVF) in women with polycystic ovary syndrome (POS), as compared to normal cycle women. METHODS: a controlled retrospective study conducted on 36 women with POS (POS group) and on 44 women with infertility due to mild male factor (control group), submitted to IVF from 1997 to 2003. Subject ages ranged from 18 to 36 years. Ovulation hyperinduction was obtained with recombinant follicle-stimulating hormone and a gonadotrophin-releasing hormone agonist. The analyzed variables were the follicles with a mean diameter of 14 to 17 mm and the follicles with diameters of 18 mm or above on the day of human chorionic gonadotrophin administration, percentage of follicles >18 mm, the number of retrieved oocytes, fertilization rate, cleavage rate, incidence of ovarian hyperstimulation syndrome (OHS), clinical pregnancy rate, and abortion rate. The variables were analyzed by the unpaired t test, Fisher exact test and Mann-Whitney test, with level of significance set at p<0.05. RESULTS: the POS group presented a larger number of retrieved follicles, most of them measuring 14 to 17 mm in diameter, compared to the control group (64.8 vs 53.9%), a lower fertilization rate (59.43 vs 79.57%) and a higher incidence of OHS (38.9 vs 9.1%). The number of retrieved oocytes, cleavage rates, pregnancy rates per embryo transfer, abortion rates and live born rates did not differ between groups. CONCLUSION: the success of IVF is impaired in women with POS due to their larger number of retrieved follicles of reduced diameter, reduced fertilization rate and high OHS rates.
Summary
Rev Bras Ginecol Obstet. 1999;21(2):85-90
DOI 10.1590/S0100-72031999000200005
Purpose: to present a profile of endometriosis, stages and results of treatment among the patients seen in our Service. Methods: the medical records of 155 patients with endometriosis treated during the period from 1991 to 1996 according to a preestablished protocol were examined. Results: mean patient age was 31 years, most patients were white, with regular menstrual cycles. The most frequently observed symptoms were dysmenorrhea, pelvic pain and infertility and were mild in most of the cases. The diagnostic methods utilized were laparoscopy or echography. There was agreement between echography and laparoscopy in 96% of cases. Laparotomy was required in 28% of cases for diagnostic elucidation and/or treatment. Endometrioma was detected in 37% of the cases and endometriosis was confirmed in only 74% of the biopsies from the lesion by anatomopathological examination. There was a significant improvement with clinical treatment regardless of the drug used, with improved symptoms in approximately 50% of the patients. Assisted fertilization was performed in 34 patients, consisting of in vitro fertilization (IVF) for 80% of them, with a 27% pregnancy/transfer rate. Conclusions: the diagnostic method of choice should be laparoscopy, although echography presented a high rate of agreement. Anatomopathological examination of the lesions should be used as an adjuvant method in the diagnosis since it is not confirmatory in all of the cases. Clinical treatment with assisted reproductive technologies is a good therapeutic option, especially with the use of IVF.
Summary
Rev Bras Ginecol Obstet. 2000;22(2):89-94
DOI 10.1590/S0100-72032000000200005
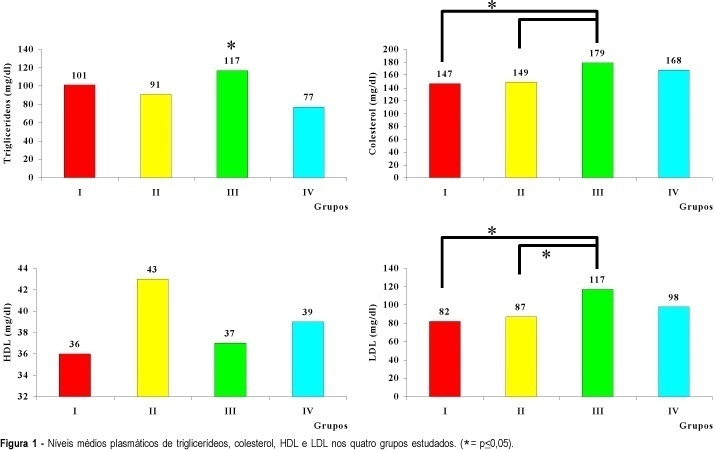
Purpose: to evaluate the lipid profile (cholesterol, triglycerides, HDL and LDL) of women with polycystic ovary syndrome (PCO) and compare it to that of women with ovulatory menstrual cycles. Methods: the patients were divided into two groups, obese and nonobese, based on body mass index, so that it would be possible to determine the joint effect of PCO and obesity on the lipid metabolism of the studied women. We studied 117 women divided into 4 groups: group I (PCO--obese), n = 33; group II (PCO--nonobese), n = 27; group III (control--obese), n = 28; group IV (control--nonobese), n = 29. Results: cholesterol levels were elevated (179 mg/dl) in obese patients with ovulatory cycles (group III) compared to group I (147 mg/dl) and group II (149 mg/dl), as also were triglyceride levels (117 mg/dl) compared to group IV (77 mg/dl) and LDL levels (117 mg/dl) compared to group I (82 mg/dl). Conclusion: these data suggest that alterations in lipid profile are related to obesity only.