You searched for:"Jurandyr Moreira de Andrade"
We found (21) results for your search.Summary
Rev Bras Ginecol Obstet. 2012;34(9):395-396
Summary
Rev Bras Ginecol Obstet. 1999;21(7):415-418
DOI 10.1590/S0100-72031999000700008
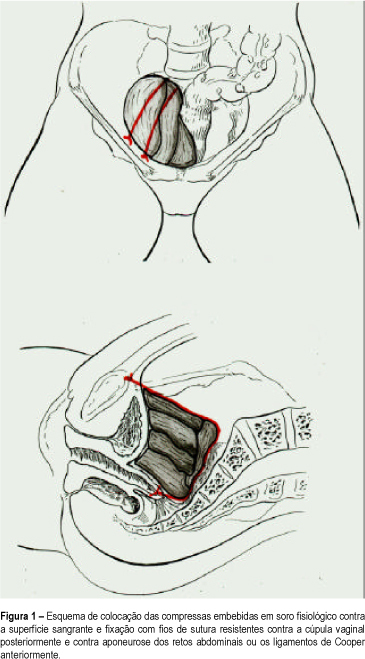
Purpose: to introduce the use of the hemostatic pack, a tampon consisting of compresses tied to the bleeding surface and left in place for 48 to 72 h and which is one of the therapeutic alternatives to be used in this situation. Patients and Methods: we evaluated 3 cases of massive bleeding during surgery, with the exchange, on average, of 1.4 blood volumes (1.2-2.4), in terms of hemostatic effectiveness of the pack and of some patient parameters such as age and amount and type of volume infused. Results: the mean age of the patients was 57 years (51, 56 and 64). Only one had been previously irradiated. The bleeding was of venous origin, from the fossa of the obturator nerve, the iliac plexus and the presacral plexus. The volume expander most often used was 0.9% physiological saline solution, followed by blood derivatives and by Ringer lactate. Two patients were submitted to ligation of the hypogastric vein during surgery, with no improvement. The use of hemostatic synthetic material was inefficient in all three cases. In one of the patients, the use of nonabsorbable sutures to close the bleeding area led to a considerable reduction of bleeding, but did not eliminate it completely. One patient died before 24 h had elapsed, with signs and symptoms of heart failure. The other two patients developed acute renal failure and one of them developed aspirative pneumonia during surgical reexploration. Conclusion: massive bleeding is related to high morbidity and mortality. Among the emergency measures used for hemostasis, the pack seems to be the most adequate.
Summary
Rev Bras Ginecol Obstet. 1999;21(1):47-54
DOI 10.1590/S0100-72031999000100008
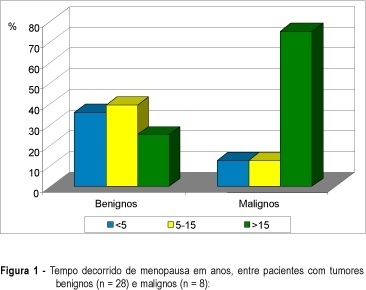
Purpose: to evaluate clinical and ultrasonic findings in patients with pelvic tumors at postmenopause and to correlate them with the final diagnosis. Patients and Methods: thirty-six postmenopausal women with pelvic tumor diagnosis were prospectively evaluated through clinical examination and endovaginal ultrasonography. Clinical follow-up with no surgical procedures was indicated for anechoic cystic tumors with or without thin unique septation and volume under 50 cm³. Needle aspiration was indicated for tumors with the same aspect, and volume of 50 to 100 cm³, whereas exploratory laparotomy was performed in the remaining patients. Diagnosis defined two groups of patients: benign (28) and malignant (8) pathologies. Results: anechoic cystic tumor with or without a thin septum indicates benignity (p = 0.0091). Tumors with solid areas indicate malignancy (p = 0.0024). Ascites correlates with malignancy (p = 0.0278). Heterogeneity, thick capsule, thick septa, and papillary projections predominated in malignancies but without no statistical significance (p > 0,05). Tumor volume indicates malignancy, with a median of 85.2 cm³ in benign tumors and 452.5 cm³ in malignancies (p = 0.0048), with a cutoff at 295 cm³ (sensitivity = 83.3% and specificity = 85.2%). Following this protocol, all malignancies were submitted to surgery and 11 benign tumor patients were treated with a conservative protocol (39.3% of all benign patients). Conclusion: conservative management is an adequate protocol for women with anechoic pelvic tumors with low volume, with or without single thin septum and without ascites. Differentiation between benign and malignant of complex and/or high volume tumors requires complementary investigation.
Summary
Rev Bras Ginecol Obstet. 1998;20(10):571-576
DOI 10.1590/S0100-72031998001000005
Purpose: to evaluate the advantages of the laparoscopic approach for conversion of abdominal hysterectomies in vaginal hysterectomies in patients with indication of concomitant adnexectomy, being considered the safety and the additional costs of the procedure. Patients and Methods: cases: 9 patients submitted to Laparoscopically Assisted Vaginal Hysterectomy (LAVH) associated with adnexectomy. Controls:18 patients submitted to Abdominal Hysterectomy (AH) associated with adnexectomy. Both groups were compared regarding preoperative characteristics and the results of the procedure. The patients submitted to LAVH and AH are similar concerning age, parity, cesarean deliveries, previous surgeries and body mass index. Results: the average surgery time was 163.9 minutes for patients submitted to LAVH and 142.8 minutes for patients submitted to AH. No patient in the LAVH group presented postoperative complications, while in the AH group 2 patients presented suture deiscence and there was 1 case of incisional hernia. The median of hospital stay was 1 day in the LAVH group and 2 days in the AH group, those of convalescence periods were 2 and 4 weeks, respectively. 55.6% of the patients in the LAVH group and 100% in the AH group needed analgesics in the postoperative period. Conclusions: LAVH was shown to be advantageous in relation to AH in terms of better recovery and lower incidence of complications in the postoperative period. The procedure is feasible and safe in a University Hospital, and without additional costs.
Summary
Summary
Rev Bras Ginecol Obstet. 2011;33(2):63-67
Summary
Rev Bras Ginecol Obstet. 2019;41(11):633-635
Summary
Rev Bras Ginecol Obstet. 2008;30(2):67-74
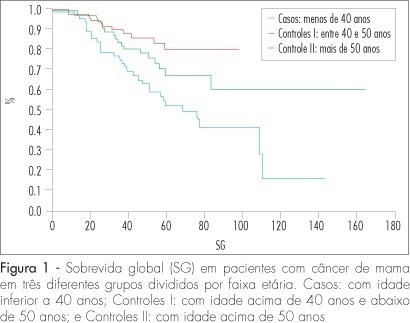
DOI 10.1590/S0100-72032008000200004
PURPOSE: to compare the epidemiologic and clinical characteristics, and the follow-up of breast cancer in women diagnosed under and over 40 years of age. METHODS: a retrospective study, case-control type, with analysis of information obtained from medical records of patients attended from January 1994 to June 2004. Cases of intraductal carcinoma and at stage IV were excluded. Three groups were formed: patients under 40 years old at the diagnosis (n=72); patients between 40 and 50 (n=68) and patients over 50 (n=75). Data about age at the moment of diagnosis, lesion largest diameter, clinical stage, type, histological grade, presence of hormonal receptors and state of the lymph nodes were collected and analyzed. The chi2 test was used for qualitative variables. For quantitative variables without normal distribution (such as number of axillary nodes with metastasis and follow-up duration), the Kruskal-Wallis' test was used. For delineating the curves of free-of-disease and global survival, the log-rank test was used. RESULTS: there was no difference among the groups in the stage distribution, concerning the tumoral differentiation grade or in the distribution of histological types, and in the estrogen receptor and c-erb-B2 expression. Difference was found in the RP expression, which was less frequent in the group of patients under 40, than in the group of patients over 50 (36.2% versus 58.4%) respectively. There was no difference among the groups in the mean tumoral diameter (5.1, 4.7 and 5 cm, respectively). There was also no difference among the groups, concerning the rate of axillary lymph node metastasis (63.9, 46.9 and 50%, respectively). The average follow-up was 54 months for all the groups. Disease recurrence occurred in 22.6% of patients under 40 years old, in 60% of patients between 40 and 50, and in 22.6% of patients over 50, with a significant difference among groups (p<0.0001). Death caused by the disease was higher among patients under 40 (46.9%) than among patients between 40 and 50 (26.9%) and over 50 (22.6%), p=0.0019. The logistic analysis showed that "age under 40" and the "presence of more than one metastatic axillary node" were independent death risk factors. CONCLUSIONS: age under 40 is an independent risk factor for breast cancer. The traditional prognostic indicators, such as stage, tumoral diameter, axillary involvement and presence of hormonal receptors are not associated with the disease evolution.