You searched for:"Miriam da Silva Wanderley"
We found (10) results for your search.Abstract
Revista Brasileira de Ginecologia e Obstetrícia. 2010;32(1):55-56
Abstract
Revista Brasileira de Ginecologia e Obstetrícia. 2017;39(2):86-89
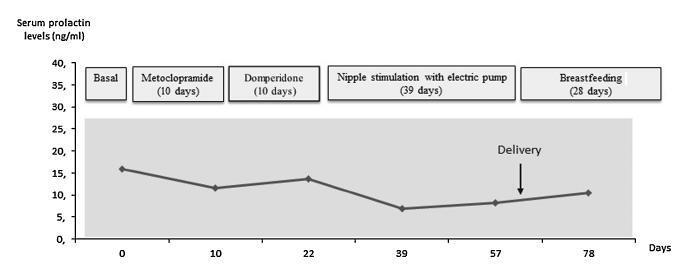
Case report of a 39-year-old intended mother of a surrogate pregnancy who underwent induction of lactation by sequential exposure to galactagogue drugs (metoclopramide and domperidone), nipple mechanical stimulation with an electric pump, and suction by the newborn. The study aimed to analyze the effect of each step of the protocol on serum prolactin levels, milk secretion and mother satisfaction, in the set of surrogacy. Serum prolactin levels and milk production had no significant changes. Nevertheless, themother was able to breastfeed for four weeks, and expressed great satisfaction with the experience. As a conclusion, within the context of a surrogate pregnancy, breastfeeding seems to bring emotional benefits not necessarily related to an increase in milk production.
Abstract
Revista Brasileira de Ginecologia e Obstetrícia. 2000;22(3):147-152
DOI 10.1590/S0100-72032000000300005
Purpose: to assess the commonest vulvovaginal complaints and vaginal discharge etiology in the Child and Teenager Gynecologic Outpatient Clinic of the University Hospital of Brasília (AGIP/HUB). Methods: we evaluated retrospectively 210 charts of patients, younger than 19 years old, who attended AGIP/HUB with vulvovaginal complaints. Results: the average age of the 210 patients was 12 ± 2.3 years, and the vaginal discharge and vulvar pruritus were the commonest complaints. Unspecific inflammatory conditions were observed in 147 (70%) of these patients and their treatment consisted of appropriate clothing, daily activities and hygienic orientation. Antibiotic treatment was necessary in 63 patients, where specific etiologic agents were found. Gardnerella, Trichomonas, HPV and syphilis were observed only in sexually active patients. They had had their first sexual intercourse when they were 14.1 ± 1.6 years old. Twenty patients also presented vulvar complaints that were easy to handle. Conclusion: Hygiene, clothing and adequate orientation for these patients and their families are fundamental to treat vulvovaginitis, almost always avoiding the use of antibiotics.
Abstract
Revista Brasileira de Ginecologia e Obstetrícia. 2018;40(4):188-195
To analyze the association between the indirect methods of evaluating insulin resistance (IR) and blood pressure, anthropometric and biochemical parameters in a population of polycystic ovary syndrome (PCOS) patients.
Cross-sectional study performed at the Hospital Universitário de Brasília (HUB, in the Portuguese acronym) involving PCOS patients diagnosed from January 2011 to January 2013. Four indirect methods, namely, fasting blood insulin level, fasting glucose/insulin ratio (G/I), homeostatic model-assessment-insulin resistance (HOMA-IR), and the quantitative insulin sensitivity check index (QUICKI), were used to obtain the IR diagnosis. The data were analyzed using the test of proportions, the Chisquare test, and Fisher exact test, when indicated.
Out of the 83 patients assessed, aged 28.79 ± 5.85, IR was found in 51.81- 66.2% of them using the G/I ratio and the QUICKI, respectively. The test of proportions did not show a significant difference between the methods analyzed. The proportion of IR diagnoses was statistically higher in obese women than in women with normal body mass index (BMI). We observed a statistically significant association between all the methods for diagnosing IR and BMI, waist circumference (WC) and lipid accumulation product (LAP). With regards to arterial hypertension (AH), we observed a significant association according to three methods, with the exception of the ratio G/I.
Insulin resistance prevalence varied according to the diagnostic method employed,with no statistical difference between them. The proportion of IR diagnoses was statistically higher in obese women than in women with normal BMI.We observed a significant association between IR andWC, BMI, LAP, as well as dyslipidemia and AH in a high proportion of patients.
Abstract
Revista Brasileira de Ginecologia e Obstetrícia. 2007;29(5):230-234
DOI 10.1590/S0100-72032007000500002
PURPOSE: to analyze the factors associated with the reproductive future of patients wishing to become pregnant after having being submitted to tubal ligation (TL), attended at a public service. METHODS: a prospective study including 98 patients previously submitted to TL, who came to the Human Reproduction Center of the University Hospital of Brasilia (HUB), from January 1996 to January 2004, wishing to become pregnant again These patients were followed up from their first appointment till the end of the study, when they answered a structured questionnaire about the social demographic aspects at both the moment they asked for the TL and the reversion of the procedure. RESULTS: the patients’ average age at the TL procedure was 25 years old. Among them, 55.1% were younger than 25, 46.9% had three or more children, and ten of them had only one child. The most common reasons for the TL procedure were: contraception (48%), financial difficulties (25.5%) and marital problems (15.3%). The major causes for wishing a new pregnancy were: a new relationship/marriage (80.6%), the desire of having another child with the same partner (8.2%), and the death of a child (6.1%). The regret time informed by most of the patients was between two and four years, and the search for reversion was between six and ten years. About 83.6% of the sample referred lack of information about the procedure and the difficulties of reversion. Twenty patients were submitted to TL reversal procedure; from the ten who became pregnant, only six delivered babies, after a full-term pregnancy. Eight patients were referred to in vitro fertilization treatment, four of them became pregnant and two delivered healthy babies. CONCLUSIONS: TL in young vulnerable women, not informed about the definitive condition of the method, may increase the search for attended reproduction services and impair their reproductive future, as far as only 8.1% of the sample delivered babies and reached their goal.
Abstract
Revista Brasileira de Ginecologia e Obstetrícia. 2019;41(8):485-492
Themoment of admission for deliverymay be inappropriate for offering an intrauterine device (IUD) to women without prenatal contraception counseling. However, in countries with high cesarean rates and deficient prenatal contraception counseling, this strategy may reduce unexpected pregnancies and repeated cesarean sections.
This was a prospective cohort study involving 100 women without prenatal contraception counseling. Postplacental IUD was offered after admission for delivery and placed during cesarean. The rates of IUD continuation, uterine perforation, and endometritis were assessed at 6 weeks and 6 months, and the proportion of women continuing with IUD at 6 months was assessed with respect to the number of previous cesareans.
Ninety-seven women completed the follow-up. The rate of IUD continuation was 91% at 6 weeks and 83.5% at 6 months. The expulsion/removal rate in the first 6 weeks was not different from that between 6 weeks and 6 months (9 vs 9.1%, respectively). There were 2 cases of endometritis (2.1%), and no case of uterine perforation. Among 81 women continuing with intrauterine device after 6-months, 31% had undergone only the cesarean section in which the IUD was inserted, 44% had undergone 2 and 25% had undergone 3 or more cesarean sections.
Two thirds of the women who continued with IUD at 6 months had undergone 2 ormore cesarean sections. Since offering trial of labor is unusual after 2 or more previous cesareans, we believe that offering IUD after admission for delivery may reduce the risk of repeated cesarean sections and its inherent risks.
Abstract
Revista Brasileira de Ginecologia e Obstetrícia. 2016;38(10):506-511
To evaluate the accuracy of transvaginal ultrasonography, hysteroscopy and uterine curettage in the diagnosis of endometrial polyp, submucous myoma and endometrial hyperplasia, using as gold standard the histopathological analysis of biopsy samples obtained during hysteroscopy or uterine curettage.
Cross-sectional study performed at the Hospital Universitário de Brasília (HUB). Data were obtained from the charts of patients submitted to hysteroscopy or uterine curettage in the period from July 2007 to July 2012.
One-hundred and ninety-one patients were evaluated, 134 of whom underwent hysteroscopy, and 57, uterine curettage. Hysteroscopy revealed a diagnostic accuracy higher than 90% for all the diseases evaluated, while transvaginal ultrasonography showed an accuracy of 65.9% for polyps, 78.1% for myoma and 63.2% for endometrial hyperplasia. Within the 57 patients submitted to uterine curettage, there was an accuracy of 56% for polyps and 54.6% for endometrial hyperplasia.
Ideally, after initial investigation with transvaginal ultrasonography, guided biopsy of the lesion should be performed by hysteroscopy, whenever necessary, in order to improve the diagnostic accuracy and subsequent clinical management.
Abstract
Revista Brasileira de Ginecologia e Obstetrícia. 2019;41(10):613-620
To evaluate the association between the acceptance on the part of the patients and their reasons to consent to or refuse medical student attendance during gynecological outpatient care, considering the participants’ demographic characteristics, consultation experience, and gender bias or lack thereof.
Face-to-face interviews with patients waiting for gynecological consultations that had been scheduled in advance at Hospital Universitário de Brasília. Contingency analyses were used to determine the levels of association among the patient variables. The accepted significance level was values of p<0.05.
We interviewed 469 patients. The comfort level with the presence of a student was strongly related to the number of students present during the consultation (Cramér V=0.671). The inclination to grant consent (a series of reasons to consent to or refuse student attendance) was significantly related (p<0.001) to the overall receptivity to student participation (ρ=0.482), the positive appraisal of student-doctor demeanor in previous consultations (ρ=0.253, N=408), and to greater levels of schooling (ρ=0.158). The patients’ receptivity was significantly related (p<0.001) to the lack of bias regarding the gender of the physician (CramérV=0.388), previous experience with students (Cramér V=0.235) and awareness of the fact that they would be present (Cramér V=0.217), older age (ρ=0.136, p=0.003), and multiparity (ρ=0.102, p=0.027).
Greater receptivity to student participation related significantly to five conditions in decreasing order of strength of association: lack of bias regarding the gender of the Ob-Gyn, previous experience with student involvement, awareness of the presence of students, older age, and multiparity. We also found that a more positive inclination to consent to student attendance correlated positively with a greater receptivity to student participation and to a suitable student-doctor demeanor.