You searched for:"Julio Cesar Teixeira"
We found (21) results for your search.Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2024;46:e-FPS10
•The negative impact of infectious diseases and their immunoprevention during the different stages of a woman’s life requires a broad approach including adolescence, adulthood, pregnancy and the postmenopausal phase.
•Immunization of pregnant women should be a priority for the protection of the maternal-fetal dyad, especially in regions with high rates of infections preventable by immunization.
•Brazil has one of the most comprehensive vaccination programs in the world – the National Immunization Program (Programa Nacional de Imunizações, PNI) – that serves all age groups: newborns, children, adolescents, adults, pregnant women and older adults, as well as groups with special needs, such as adolescents, pregnant and older adult women.
•However, vaccination coverage remains below ideal for all available vaccines, especially among adolescents and pregnant women, and Febrasgo is committed to collaborating with the PNI to combat vaccine hesitancy.
•The gynecologist/obstetrician is the reference physician for women, therefore the access to information and updates regarding all vaccines recommended for their patients is extremely important for this professional, aiming at the greatest possible protection.
•The objective of this Febrasgo Position Statement is to bring an update to women’s vaccination schedule, covering some vaccines that are available, including new approved vaccines and those in the commercialization phase.
•This work is a compilation of the First Febrasgo Scientific Immunization Forum held in the city of São Paulo in October 2023 with the objective to update recommendations for vaccines in use and new innovative vaccines soon to be available.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2024;46:e-rbgoedt2
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2024;46:e-rbgo44
To describe Top-hat results and their association with margin status and disease relapse in a referral facility in Brazil.
A retrospective study of 440 women submitted to LEEP to treat HSIL, in which 80 cases were complemented immediately by the top hat procedure (Top-hat Group - TH). TH Group was compared to women not submitted to Top-hat (NTH). The sample by convenience included all women that underwent LEEP from January 2017 to July 2020. The main outcome was the histological result. Other variables were margins, age, transformation zone (TZ), depth, and relapse. The analysis used the Chi-square test and logistic regression.
The TH Group was predominantly 40 and older (NTH 23.1% vs. TH 65.0%, p<0.001). No difference was found in having CIN2/CIN3 as the final diagnosis (NTH 17.0% vs. TH 21.3%, p=0.362), or in the prevalence of relapse (NTH 12.0% vs. TH 9.0%, p=0.482). Of the 80 patients submitted to top hat, the histological result was CIN2/CIN3 in eight. A negative top hat result was related to a negative endocervical margin of 83.3%. A CIN2/CIN3 Top-hat result was related to CIN2/CIN3 margin in 62.5% (p=0.009). The chance of obtaining a top hat negative result was 22.4 times higher (2.4-211.0) when the endocervical margin was negative and 14.5 times higher (1.5-140.7) when the ectocervical margin was negative.
The top hat procedure did not alter the final diagnosis of LEEP. No impact on relapse was observed. The procedure should be avoided in women of reproductive age.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2023;45(1):21-30
To evaluate the rates of precancerous lesions, colposcopy referral, and positive predictive value (PPV) by age groups of a population-based screening with DNA-HPV testing.
The present demonstration study compared 16,384 HPV tests performed in the first 30 months of the program with 19,992 women tested in the cytology screening. The colposcopy referral rate and PPV for CIN2+ and CIN3+ by age group and screening program were compared. The statistical analysis used the chi-squared test and odds ratio (OR) with 95% confidence interval (95%CI).
The HPV tests were 3.26% positive for HPV16-HPV18 and 9.92% positive for 12 other HPVs with a 3.7 times higher colposcopy referral rate than the cytology program, which had 1.68% abnormalities. Human Papillomavirus testing detected 103 CIN2, 89 CIN3, and one AIS, compared with 24 CIN2 and 54 CIN3 detected by cytology (p < 0.0001). The age group between 25 and 29 years old screened by HPV testing had 2.4 to 3.0 times more positivity, 13.0% colposcopy referral, twice more than women aged 30 to 39 years old (7.7%; p < 0.0001), and detected 20 CIN3 and 3 early-stage cancer versus 9 CIN3 and no cancer by cytology screening (CIN3 OR= 2.10; 95%CI: 0.91 -5.25; p = 0.043). The PPV of colposcopy for CIN2+ ranged from 29.5 to 41.0% in the HPV testing program.
There was a significant increase in detections of cervix precancerous lesions in a short period of screening with HPV testing. In women < 30 years old, the HPV testing exhibited more positivity, high colposcopy referral rate, similar colposcopy PPV to older women, and more detection of HSIL and early-stage cervical cancer.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2022;44(6):631-635
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2022;44(6):567-572
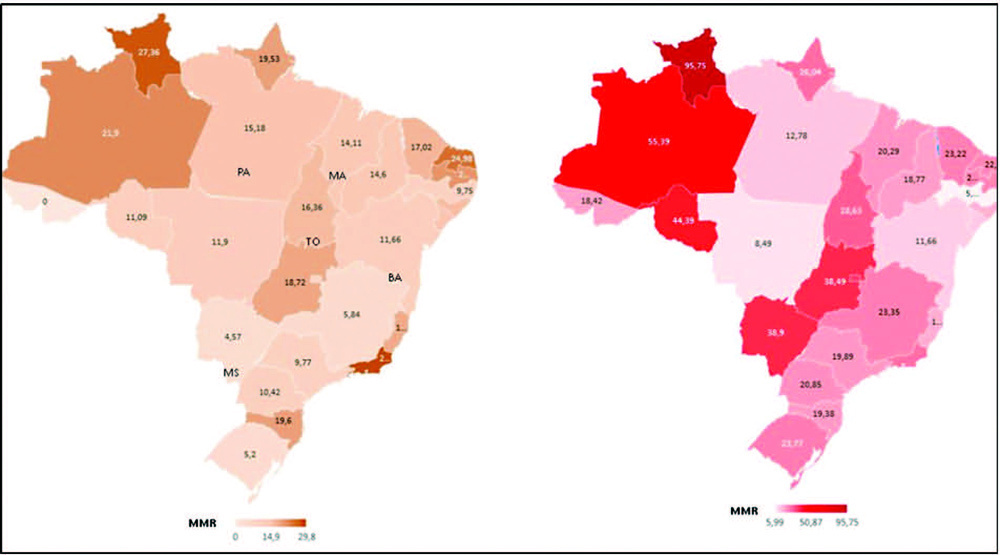
To compare death rates by COVID-19 between pregnant or postpartum and nonpregnant women during the first and second waves of the Brazilian pandemic.
In the present population-based evaluation data from the Sistema de Informação da Vigilância Epidemiológica da Gripe (SIVEP-Gripe, in the Portuguese acronym), we included women with c (ARDS) by COVID-19: 47,768 in 2020 (4,853 obstetric versus 42,915 nonobstetric) and 66,689 in 2021 (5,208 obstetric versus 61,481 nonobstetric) and estimated the frequency of in-hospital death.
We identified 377 maternal deaths in 2020 (first wave) and 804 in 2021 (second wave). The death rate increased 2.0-fold for the obstetric (7.7 to 15.4%) and 1.6-fold for the nonobstetric groups (13.9 to 22.9%) from 2020 to 2021 (odds ratio [OR]: 0.52; 95% confidence interval [CI]: 0.47–0.58 in 2020 and OR: 0.61; 95%CI: 0.56– 0.66 in 2021; p < 0.05). In women with comorbidities, the death rate increased 1.7-fold (13.3 to 23.3%) and 1.4-fold (22.8 to 31.4%) in the obstetric and nonobstetric groups, respectively (OR: 0.52; 95%CI: 0.44–0.61 in 2020 to OR: 0.66; 95%CI: 0.59–0.73 in 2021; p <0.05). In women without comorbidities, the mortality rate was higher for nonobstetric (2.4 times; 6.6 to 15.7%) than for obstetric women (1.8 times; 5.5 to 10.1%; OR: 0.81; 95%CI: 0.69–0.95 in 2020 and OR: 0.60; 95%CI: 0.58–0.68 in 2021; p <0.05).
There was an increase in maternal deaths from COVID-19 in 2021 compared with 2020, especially in patients with comorbidities. Death rates were even higher in nonpregnant women, with or without comorbidities.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2022;44(3):264-271
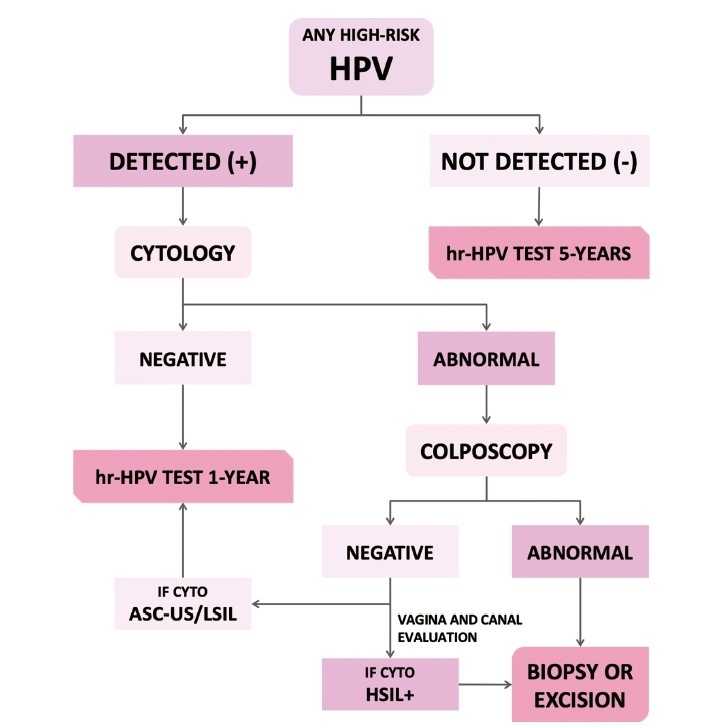
The present update is a reassessment of the 2018 ‘Guidelines for HPV-DNA Testing for Cervical Cancer Screening in Brazil’ (Zeferino et al.)9, according to the changes observed in new international guidelines and knowledge updates. The most relevant and recent guidelines were assessed. Questions regarding the clinical practice were formulated, and the answers considered the perspective of the public and private sectors of the Brazilian health system. The review addressed risk-based strategies regarding age to start and stop screening, the use of cytology and colposcopy to support management decisions, treatment, follow-up strategies, and screening in specific groups, including vaccinated women. The update aims to improve the prevention of cervical cancer and to reduce overtreatment and the misuse of HPV testing.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2021;43(12):885-886