You searched for:"Ana Katherine Gonçalves"
We found (10) results for your search.Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2024;46:e-rbgo38
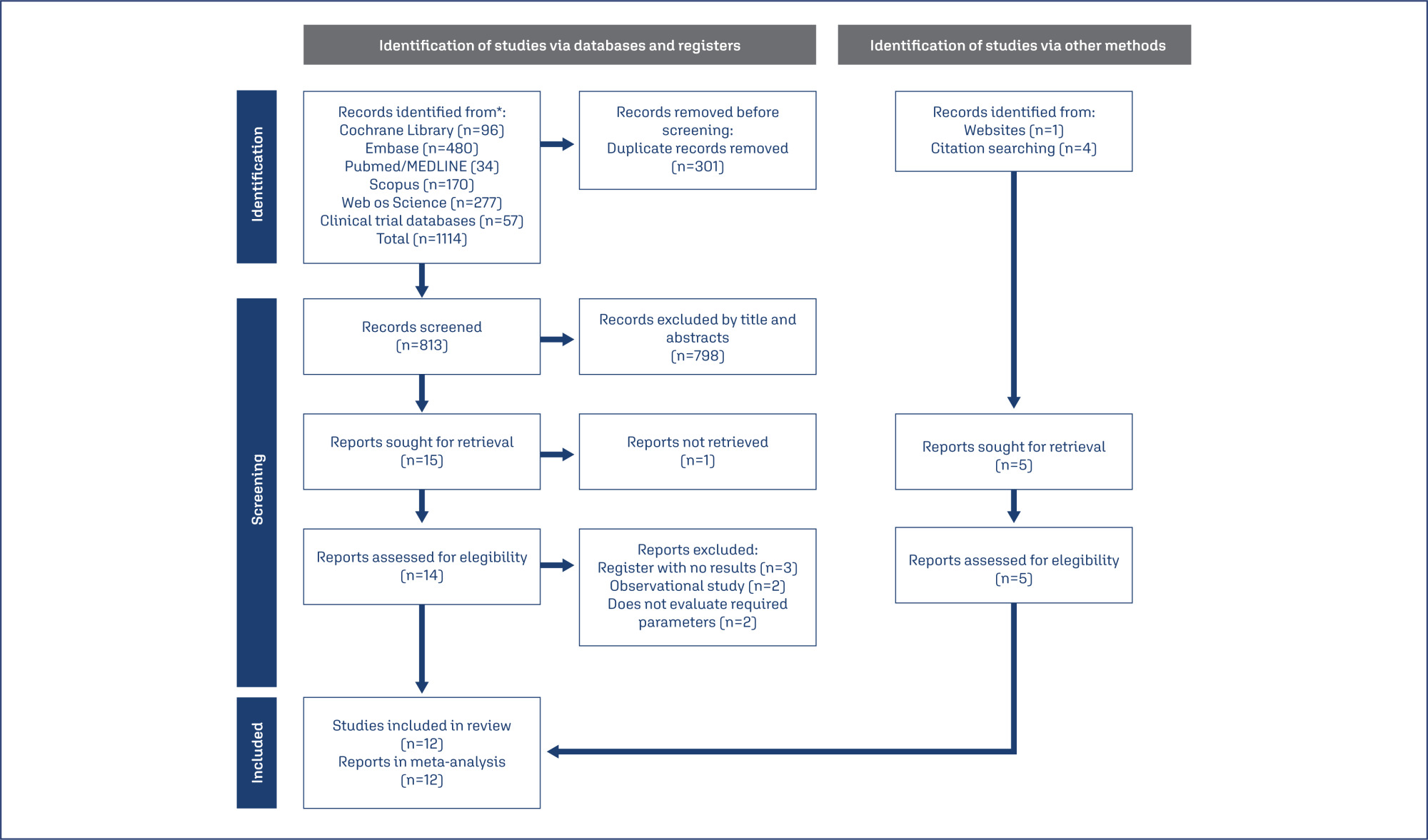
This meta-analysis of randomized controlled trials (RCTs) aimed to update evidence on the effectiveness and safety of laser therapy for treating genitourinary syndrome of menopause (GSM).
Manuscripts published until May 2023 were systematically searched in PubMed; Embase; Scopus; Web of Science; CENTRAL; CINAHL; and clinical trial databases (www.trialscentral.org, www.controlled-trials.com, and clinicaltrials.gov), with no language and year of publication restriction.
RCTs with women diagnosed with GSM, and the intervention was vaginal laser therapy (CO2-laser or Er: YAG-laser) comparing with placebo (sham therapy), no treatment or vaginal estrogen therapy.
Two authors evaluated the publications for inclusion based on the title and abstract, followed by reviewing the relevant full-text articles. Disagreements during the review process were addressed by consensus, with the involvement of a third author.
Twelve RCTs, representing a total of 5147 participants, were included in this review. Vaginal health index (VHI) significantly improved in the carbon dioxide laser (CO2-laser) therapy group (MD=2.21; 95% CI=1.25 to 3.16), while dyspareunia (MD=−0.85; 95% CI=−1.59 to −0.10), dryness (MD=−0.62; 95% CI=−1.12 to −0.12) and burning (MD= −0.64; 95% CI=−1.28 to −0.01) decreased. No serious adverse effects were reported.
CO2-laser increases VHI score and decreases dyspareunia, dryness and burning, especially when compared to sham-laser. However, the certainty of the evidence is low, thus preventing the recommendation of laser therapy for GSM management.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2023;45(12):808-817
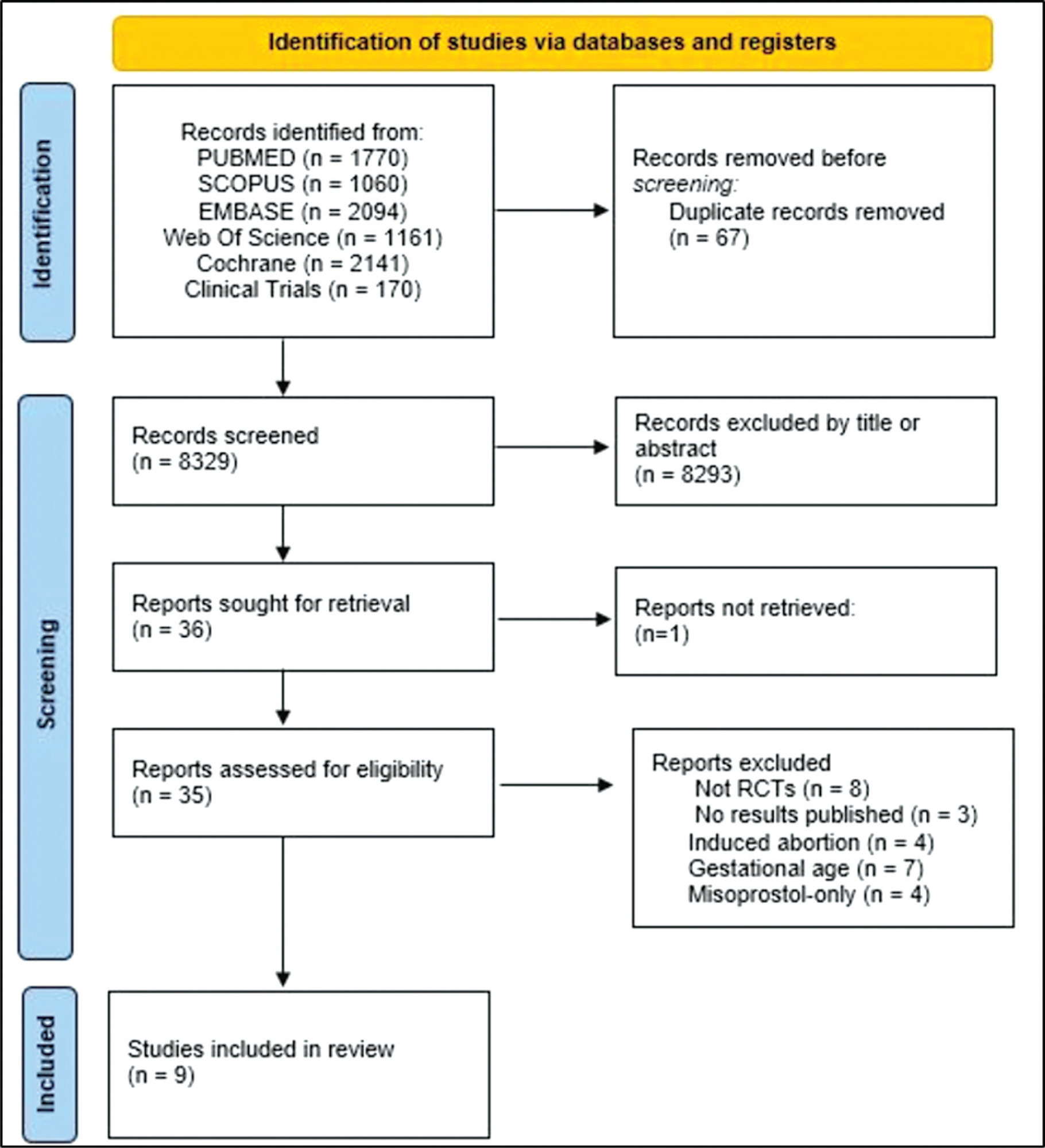
To assess the efficacy, safety, and acceptability of misoprostol in the treatment of incomplete miscarriage.
The PubMed, Scopus, Embase, Web of Science, Cochrane Library, and Clinical Trials databases (clinicaltrials.gov) were searched for the relevant articles, and search strategies were developed using a combination of thematic Medical Subject Headings terms and text words. The last search was conducted on July 4, 2022. No language restrictions were applied.
Randomized clinical trials with patients of gestational age up to 6/7 weeks with a diagnosis of incomplete abortion and who were managed with at least 1 of the 3 types of treatment studied were included. A total of 8,087 studies were screened.
Data were synthesized using the statistical package Review Manager V.5.1 (The Cochrane Collaboration, Oxford, United Kingdom). For dichotomous outcomes, the odds ratio (OR) and 95% confidence interval (CI) were derived for each study. Heterogeneity between the trial results was evaluated using the standard test, I2 statistic.
When comparing misoprostol with medical vacuum aspiration (MVA), the rate of complete abortion was higher in the MVA group (OR = 0.16; 95%CI = 0.07–0.36). Hemorrhage or heavy bleeding was more common in the misoprostol group (OR = 3.00; 95%CI = 1.96–4.59), but pain after treatment was more common in patients treated with MVA (OR = 0.65; 95%CI = 0.52–0.80). No statistically significant differences were observed in the general acceptability of the treatments.
Misoprostol has been determined as a safe option with good acceptance by patients.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2022;44(10):986-994
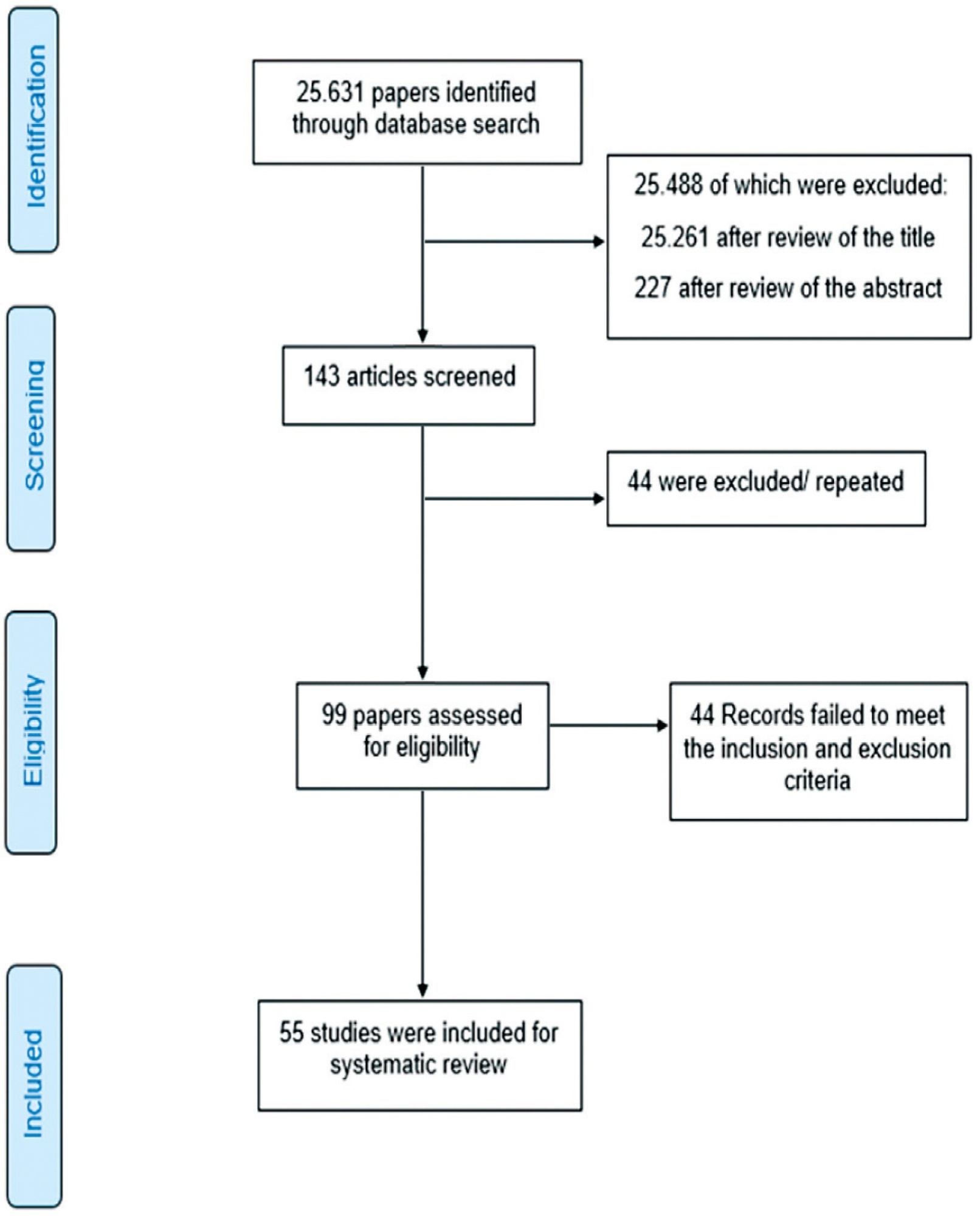
To evaluate the efficacy of the hormonal and nonhormonal approaches to symptoms of sexual dysfunction and vaginal atrophy in postmenopausal women.
We conducted a search on the PubMed, Embase, Scopus, Web of Science, SciELO, the Cochrane Central Register of Controlled Trials (CENTRAL), and Cumulative Index to Nursing and Allied Health Literature (CINAHL) databases, as well as on clinical trial databases. We analyzed studies published between 1996 and May 30, 2020. No language restrictions were applied.
We selected randomized clinical trials that evaluated the treatment of sexual dysfunction in postmenopausal women.
Three authors (ACAS, APFC, and JL) reviewed each article based on its title and abstract. Relevant data were subsequently taken from the full-text article. Any discrepancies during the review were resolved by consensus between all the listed authors.
A total of 55 studies were included in the systematic review. The approaches tested to treat sexual dysfunction were as follows: lubricants and moisturizers (18 studies); phytoestrogens (14 studies); dehydroepiandrosterone (DHEA; 8 studies); ospemifene (5 studies); vaginal testosterone (4 studies); pelvic floor muscle exercises (2 studies); oxytocin (2 studies); vaginal CO2 laser (2 studies); lidocaine (1 study); and vitamin E vaginal suppository (1 study).
We identified literature that lacks coherence in terms of the proposed treatments and selected outcome measures. Despite the great diversity in treatment modalities and outcome measures, the present systematic review can shed light on potential targets for the treatment, which is deemed necessary for sexual dysfunction, assuming that most randomized trials were evaluated with a low risk of bias according to the Cochrane Collaboration risk of bias tool. The present review is registered with the International Prospective Register of Systematic Reviews (PROSPERO; CRD42018100488).
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2020;42(5):303-304
The COVID-19 outbreak is increasing around the world in the number of cases, deaths, and affected countries. Currently, the knowledge regarding the clinical impact of COVID-19 on maternal, fetal, and placental aspects of pregnancy is minimal. Although the elderly and men were the most affected population, in previous situations, such as the 2009 H1N1 influenza pandemic and the Ebola epidemic, pregnant women were more likely to develop complications than nonpregnant women. There are unanswered questions specific to pregnant women, such as whether pregnant women are more severely affected and whether intrauterine transmission occurs. Additional information is needed to inform key decisions, such as whether pregnant health care workers should receive special consideration, whether to separate infected mothers and their new borns, and whether it is safe for infected women to breastfeed.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2018;40(6):369-371
Hemangioma is a benign neoplasm that may affect the vulva, and it can cause functional or emotional disability. This article reports the case of a 52-year-old female patient with a history of a genital ulcer for the past 3 years and who had undergone various treatments with creams and ointments. The patient was biopsied and diagnosed with vulvar hemangioma and was subsequently submitted to surgical excision of the lesion. We emphasize the importance of following the steps of the differential diagnosis and proceeding with a surgical approach only if necessary.

Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2016;38(11):559-563
To identify pregnancy as a causative factor of sexual dysfunction among expectant women.
A prospective study with 225 expectant mothers seen in the prenatal clinic of a federal university. Sexual function was evaluated by means of the Female Sexual Function Index (FSFI), and all domains were analyzed (desire, arousal, lubrication, orgasm, satisfaction, and pain). Initially, a univariate analysis of the sample was done. The averages for each domain according to the risk of sexual dysfunction (FSFI ≤ 26.5) were compared using the Student’s t-test for independent samples. The strength of the correlation between sexual dysfunction and all sociodemographic, clinical and behavioral variables was measured by the Chi-Square (X2) test. Then, odds ratios (ORs) and their confidence intervals were assigned to perform a bivariate analysis. Any p values less than 0.05 were considered significant.
Approximately two-thirds of the women (66.7%) showed signs of risk of sexual dysfunction (FSFI ≤ 26.5). Within these cases, all sexual dysfunction domains (desire, arousal, lubrication, orgasm, satisfaction, and pain) were found to be statistically significant (p < 0.001). The domains most affected were desire (2.67), satisfaction (2.71) and arousal (2.78).
Pregnancy appears to be an important causative factor of sexual dysfunction among pregnant women.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2016;38(3):154-159
To correlate the expression of high-risk HPV E6 mRNA with pap smear, colposcopy, and biopsy results in women with high grade squamous intraepithelial lesion (HSIL).
A cross-sectional study was performed on women referred for primary care services after cytological diagnosis of HSIL. We evaluated the expression of E6/E7 mRNA of HPV types 16,18,31,33, and 45 and correlated the results with those of Pap smear, colposcopy, and biopsy. For amplification/detection of mRNA E6 / E7 we used NucliSENSEasyQ kit to detect HPV mRNA by polymerase chain reaction with primers/ probes for HPV types 16, 18, 31, 33, and 45.
Out of 128 valid tests, the results of 30 (23.4%) tests were negative and 98 (70%) tests were positive. Only one type of HPV was detected in 87.7% of the E6/E7 mRNA positive cases. HPV16 was detected in 61.2% of the cases, followed by HPV33 (26.5%), HPV31 (17.3%), HPV18 (10%), and HPV45 (4.08%). Pap smear tests revealed that the E6/E7 test was positive in 107 (83.8%) women with atypical squamous cells - high grade (ASC-H), HSIL, or higher. The E6/E7 test was positive in 69 (57.5%) specimens presenting negative cytology results. When analyzing the association with colposcopy results, the frequency of positive E6/E7 results increased with the severity of the injury, ranging from 57.1% in women without colposcopy-detected injury to 86.5% in those with higher levels of colposcopy findings. Of the 111 women who underwent biopsy and E6/E7 testing, the E6/E7 test was positive in 84.7% of the women who presented with lesions of cervical intraepithelial neoplasia (CIN) grade 2 or higher. Finally, 41.2% of women with a negative biopsy presented a positive E6/E7 test.
E6/E7mRNA expression was higher in women with HSIL and CIN grade 2 or higher.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2014;36(3):107-112
DOI 10.1590/S0100-72032014000300003
To evaluate the impact of sexual and reproductive health theme insertion in the undergraduate medical curriculum at a Brazilian public university.
We developed an instrument for cognitive assessment in sexual and reproductive health based on the subjects addressed in the optional curriculum component Reproductive Health, resulting in an objective multiple choice test containing 27 items. The selected topics were: human, sexual and reproductive rights (HSRR), sexuality, institutional violence, gender, sexual violence, conception, contraception, abortion/legal interruption of pregnancy, maternal mortality and sexually transmitted infections (STIs) - HIV/AIDS. The subjects were grouped into three dimensions of knowledge: HSRR, legal/institutional and biomedical. Two multivariate models were adjusted in the analysis of covariance.
The study included 183 students, 127 of the group who took the elective curriculum course reproductive health (RH Group) and 56 who did not (Non-RH Group). Ninety-six students (52.5%) were males and 87 (47.5%) were females. Mean age was 24.7±1.9 years for the RH Group and 24.4±2.6 for the Non-RH Group. The average performance of the SR Group was higher than that of Non-RH subjects regarding the following subjects: HSRR, sexuality, institutional violence, sexual violence, abortion/legal interruption, and STDs - HIV/AIDS. There was no gender difference in performance, except for the theme maternal mortality, in which males scored worse than females (6.9±0.2 and 7.8±0.2, respectively; p<0.05).
The participation of students in the elective curriculum component Reproductive Health was associated with better performance in some dimensions of cognitive assessment, suggesting a positive impact of this initiative on general medical education.