You searched for:"Joaquim Teodoro de Araujo Neto"
We found (2) results for your search.Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2010;32(3):144-149
DOI 10.1590/S0100-72032010000300008
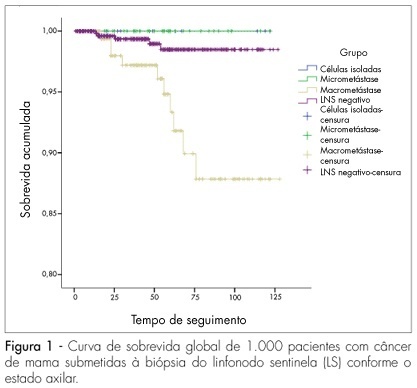
PURPOSE: to evaluate which clinical, pathological or immunohistochemical factors may be predictive of metastatic involvement of other lymph nodes in patients with breast carcinoma undergoing sentinel lymph node biopsy (SLNB). METHODS: a retrospective study carried out with 1,000 successive patients with SLNB from 1998 to 2008. Age, tumor size, histological grade, lymphovascular invasion, hormone receptor status and HER-2, size of metastasis and number of positive SLN were evaluated. The associations between the characteristics of the tumors and the types of metastases were evaluated through χ2 corrected likelihood ratio tests for insufficient samples. RESULTS: mean age was 57.6 years and mean tumor size was 1.85 cm. A total of 72.2% SLN were negative and 27.8% were positive, but in 61.9% of the cases, the SLN was the only positive one, with 78.4% having macrometastases, 17.3% micrometastases and 4.3% isolated tumor cells (CTI). Tumor size was predictive of metastases in non-sentinel lymph nodes. After 54 months of follow-up, there were no recurrences in patients with CTI, but one local recurrence and two systemic recurrences were observed in the micrometastasis group, as well as four local and 30 distant metastases in the macrometastasis group. CONCLUSIONS: among the clinical parameters studied, only tumor size was correlated with metastatic involvement in axillary lymph nodes. The size of the metastases and the number of positive SLN also directly increased the possibility of systemic recurrence. The different rates of recurrence indicate that the biological significance of these types of metastases is different and that patients with SLN metastases may also have different risks of metastatic involvement of other axillary lymph nodes.


Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2010;32(3):144-149
DOI 10.1590/S0100-72032010000300008
PURPOSE: to evaluate which clinical, pathological or immunohistochemical factors may be predictive of metastatic involvement of other lymph nodes in patients with breast carcinoma undergoing sentinel lymph node biopsy (SLNB). METHODS: a retrospective study carried out with 1,000 successive patients with SLNB from 1998 to 2008. Age, tumor size, histological grade, lymphovascular invasion, hormone receptor status and HER-2, size of metastasis and number of positive SLN were evaluated. The associations between the characteristics of the tumors and the types of metastases were evaluated through χ2 corrected likelihood ratio tests for insufficient samples. RESULTS: mean age was 57.6 years and mean tumor size was 1.85 cm. A total of 72.2% SLN were negative and 27.8% were positive, but in 61.9% of the cases, the SLN was the only positive one, with 78.4% having macrometastases, 17.3% micrometastases and 4.3% isolated tumor cells (CTI). Tumor size was predictive of metastases in non-sentinel lymph nodes. After 54 months of follow-up, there were no recurrences in patients with CTI, but one local recurrence and two systemic recurrences were observed in the micrometastasis group, as well as four local and 30 distant metastases in the macrometastasis group. CONCLUSIONS: among the clinical parameters studied, only tumor size was correlated with metastatic involvement in axillary lymph nodes. The size of the metastases and the number of positive SLN also directly increased the possibility of systemic recurrence. The different rates of recurrence indicate that the biological significance of these types of metastases is different and that patients with SLN metastases may also have different risks of metastatic involvement of other axillary lymph nodes.


Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2005;27(7):421-424
DOI 10.1590/S0100-72032005000700009
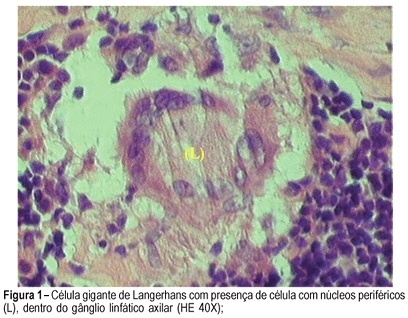
Report of a case of an 83-year-old woman presenting a nodule and skin retraction in the right breast for eight months. On physical examination, a solid nodule of 5 cm was observed, located in the upper-lateral quadrant of the right breast, associated with skin retraction and ipsilateral lymph nodes. Mammographic findings showed irregularly limited nodules of 4 cm in the upper-lateral quadrant of the right breast (bi-rads V). Clinical staging: T2N1M0 (IIB). Surgical treatment included a modified radical mastectomy with axillary dissection levels I, II, and III. Histopathologic evaluation demonstrated the presence of an infiltrating lobular carcinoma measuring 2.5 cm (T2), presence of granulomatous lymphadenitis caused by tuberculosis in level I, II, and III lymph nodes, associated with lobular carcinoma metastasis in a single level I lymph node. Pathologic staging: pT2pN1aM0. The treatment for the axillary tuberculous lymphadenitis was done with rifampin, isoniazid and pyrazinamide for one year. Hormone receptors were positive, and adjuvant therapy was initiated with tamoxifen. During the first year of follow-up the patient had no signal of local recurrence or distant metastases.


Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2005;27(7):421-424
DOI 10.1590/S0100-72032005000700009
Report of a case of an 83-year-old woman presenting a nodule and skin retraction in the right breast for eight months. On physical examination, a solid nodule of 5 cm was observed, located in the upper-lateral quadrant of the right breast, associated with skin retraction and ipsilateral lymph nodes. Mammographic findings showed irregularly limited nodules of 4 cm in the upper-lateral quadrant of the right breast (bi-rads V). Clinical staging: T2N1M0 (IIB). Surgical treatment included a modified radical mastectomy with axillary dissection levels I, II, and III. Histopathologic evaluation demonstrated the presence of an infiltrating lobular carcinoma measuring 2.5 cm (T2), presence of granulomatous lymphadenitis caused by tuberculosis in level I, II, and III lymph nodes, associated with lobular carcinoma metastasis in a single level I lymph node. Pathologic staging: pT2pN1aM0. The treatment for the axillary tuberculous lymphadenitis was done with rifampin, isoniazid and pyrazinamide for one year. Hormone receptors were positive, and adjuvant therapy was initiated with tamoxifen. During the first year of follow-up the patient had no signal of local recurrence or distant metastases.


Search
Search in:
breast breast cancer Breast neoplasms Cesarean section Endometriosis infertility Maternal mortality Menopause Obesity Polycystic ovary syndrome Postpartum period Pregnancy Pregnancy complications Prenatal care prenatal diagnosis Quality of life Risk factors Ultrasonography Uterine cervical neoplasms Women’s health
