You searched for:"César Cabello"
We found (9) results for your search.Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2022;44(9):871-877
This study aimed to evaluate the diagnostic profile of breast cancer cases during the coronavirus disease 2019 (COVID-19) pandemic compared with the previous year.
It is a retrospective study of cases diagnosed by a reference service in the public health system of Campinas, SP, Brazil. Two periods were analyzed: March to October 2019 (preCOVID period) and March to October 2020 (COVID-period). All women diagnosed during the periods were included. The Chi-Squared or Fisher exact and Mann-Whitney tests were used.
In the preCOVID and COVID periods, breast cancers were diagnosed, respectively, in 115 vs 59 women, and the mean ages at diagnosis were 55 and 57 years (p = 0.339). In the COVID period, the family history of breast cancer was more observed (9.6% vs 29.8%, p < 0.001), cases were more frequently symptomatic (50.4% vs 79.7%, p < 0.001) and had more frequently palpable masses (56.5% vs 79.7%, p = 0.003). In symptomatic women, the mean number of days from symptom to mammography were 233.6 (458.3) in 2019 and 152.1 (151.5) in 2020 (p = 0.871). Among invasive tumors, the proportion of breast cancers in stages I and II was slightly higher in the COVID period, although not significantly (76.7% vs 82.4%, p = 0.428). Also in the COVID period, the frequency of luminal A-like tumors was lower (29.2% vs 11.8%, p = 0.018), of triple-negative tumors was twice as high (10.1% vs 21.6%, p = 0.062), and of estrogen receptor-positive tumors was lower (82.2% vs 66.0%, p = 0.030).
During the COVID-19 pandemic, breast cancer diagnoses were reduced. Cases detected were suggestive of a worse prognosis: symptomatic women with palpable masses and more aggressive subtypes. Indolent tumors were those more sensitive to the interruption in screening.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2021;43(4):297-303
To evaluate the number of patients with early-stage breast cancer who could benefit from the omission of axillary surgery following the application of the Alliance for Clinical Trials in Oncology (ACOSOG) Z0011 trial criteria.
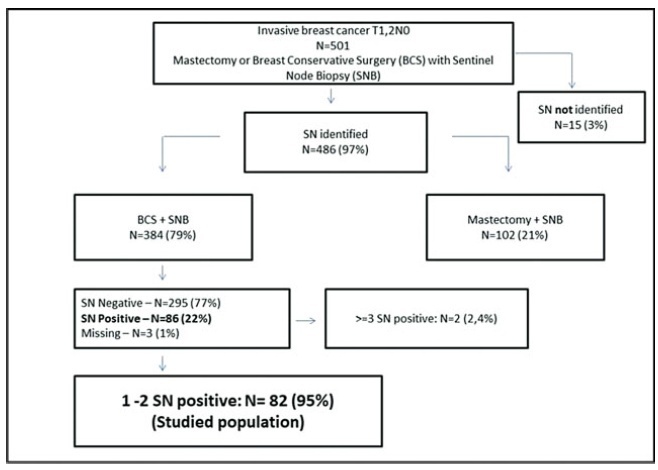
A retrospective cohort study conducted in the Hospital da Mulher da Universidade Estadual de Campinas. The study population included 384 women diagnosed with early-stage invasive breast cancer, clinically negative axilla, treated with breast-conserving surgery and sentinel lymph node biopsy, radiation therapy, chemotherapy and/or endocrine therapy, from January 2005 to December 2010. The ACOSOG Z0011 trial criteria were applied to this population and a statistical analysis was performed to make a comparison between populations.
A total of 384 patients underwent breast-conserving surgery and sentinel lymph node biopsy. Of the total number of patients, 86 women underwent axillary lymph node dissection for metastatic sentinel lymph nodes (SNLs). One patient underwent axillary node dissection due to a suspicious SLN intraoperatively, thus, she was excluded fromthe study. Among these patients, 82/86 (95.3%) had one to two involved sentinel lymph nodes andmet the criteria for the ACOSOG Z0011 trial with the omission of axillary lymph node dissection. Among the 82 eligible women, there were only 13 cases (15.9%) of lymphovascular invasion and 62 cases (75.6%) of tumors measuring up to 2 cm in diameter (T1).
The ACOSOG Z0011 trial criteria can be applied to a select group of SLNpositive patients, reducing the costs and morbidities of breast cancer surgery.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 1998;20(6):303-308
DOI 10.1590/S0100-72031998000600002
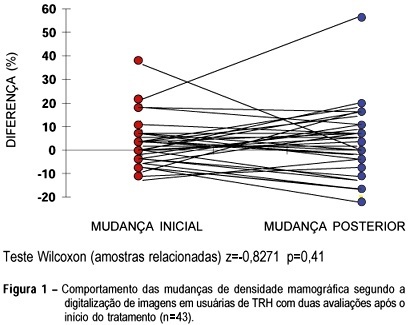
Objective: to compare mammographic density changes, case by case, according to image digitization in three consecutive evaluations of users or nonusers of hormonal replacement therapy (HRT). Methods: 59 postmenopausal women were evaluated, 43 being users of cyclic or continuous estro-progestin hormonal replacement therapy, and 16 nonusers. The criteria of inclusion were: amenorrhea for at least 12 months, a normal mammographic examination at the beginning of the HRT (users) or the clinical follow-up without HRT (nonusers), at two incidences (mediolateral and craniocaudal). The following variables were used for the evaluation of mammary density: initial change - the difference between the first mammography after HRT performed in 12 ± 3 months and the mammography performed before HRT-and final change - the difference between the second mammography after HRT performed in 24 ± 3 months and the mammography performed before HRT. Wilcoxon and c² tests were used in order to evaluate the differences in mammographic density changes. Results: more than half (56.3%) of the women, HRT users with initial increase in mammographic density remained with the increase after the final evaluation. This finding was not significant (p=0.617). In the same group, the initial nonincrease was significantly associated with the final nonincrease (p=0.017). Among the nonusers, all breasts that were not totally fat at the initial evaluation presented a mammographic density decrease at the final evaluation. Conclusions: the majority of HRT users presenting mammographic density increase at the first evaluation, after approximately one year of use, remained with the increase at a second evaluation. After some time, the nonusers tended to present a significant mammographic density decrease (p=0.003).
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 1999;21(8):431-437
DOI 10.1590/S0100-72031999000800002
Purpose: to evaluate risk factors and papillomavirus (HPV) associated lesions in male partners of women with genital intraepithelial neoplasia. Patients and Methods: three hundred and thirty-seven men were evaluated by urethral cytology, peniscopy, and biopsy, if necessary. We analyzed the results and the relations to age, educational level, smoking, contact time with the present partner, age at first intercourse, number of partners, previous sexually transmitted diseases (STD), circumcision, peniscopic findings, and female lesion grade. Results: peniscopy was positive in 144 (42,7%) and HPV infection was diagnosed in 105 (31,2%). Smoking, contact time with the present partner up to 6 months, and more than one previous sexual partner were associated with HPV lesions (p<0,05). The urethral cytology was suspect in 4,2% and smoking, positive peniscopy or biopsy and partners of women with high-grade lesion (p<0,05) were associated with the diagnosis. 72.1% of 229 biopsies were positive, independently of the peniscopic findings and women's lesion grade. Conclusions: HPV infection was diagnosed in 31.2% and was associated with smoking, contact time with the present partner up to 6 months and more than one previous sexual partner, but not with the female lesion grade, educationa level, previous STD, circumcision and peniscopic findings.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2004;26(2):125-130
DOI 10.1590/S0100-72032004000200007
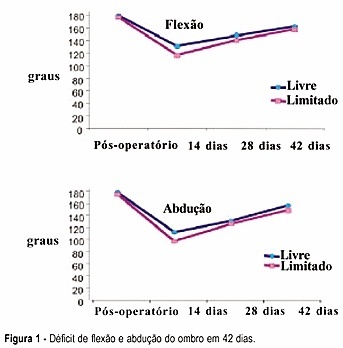
PURPOSE: to evaluate the efficacy of a physical exercise protocol in the recovery of shoulder movement in women who underwent complete axillary lymph node dissection due to breast carcinoma, comparing free and restricted amplitude movements. METHODS: 59 women who underwent complete axillary lymph node dissection associated with modified mastectomy (46) or quadrantectomy (13) were included in this clinical, prospective and randomized study. On the first day after surgery 30 women were randomized to do the shoulder movement with free amplitude and 29 women had this amplitude restricted to 90º in the first 15 days. Nineteen exercises were done, three sessions per week, for six weeks. Mean (± standard error) deficits of shoulder flexion and abduction were compared, as well as gross and adjusted incidence rates of seroma and dehiscence. RESULTS: 42 days after surgery, flexion and abduction means were similar in the two groups. Both presented a mean flexion deficit (17.2º and 21.6º, respectively), and abduction deficit (19.7º and 26.6º, respectively). The incidence rates of seroma and dehiscence were neither related to exercise nor to the type of surgery, time of drain permanence, number of dissected or compromised lymph nodes, age or obesity. CONCLUSION: early physiotherapy with free movement of the women's shoulder was associated neither with functional capacity nor with postsurgical complications.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2004;26(1):45-52
DOI 10.1590/S0100-72032004000100007
PURPOSE: to evaluate the relationship between epidemiologic, anthropometric, reproductive and hormonal factors and mammographic density in postmenopausal women. METHODS: this is a retrospective, cross-sectional study, including 144 women aged 45 years or more, with at least 12 months of amenorrhea and who were non users of hormone replacement therapy during the last six months. Medical charts were reviewed to evaluate age, weight, body mass index (BMI), parity, age at menarche, age at menopause and levels of estradiol, follicle stimulating (FSH) and luteinizing hormones. Mammograms were analyzed by two blinded investigators. The films were taken in the craniocaudal and mediolateral views and mammography was classified as dense and nondense, according to the Wolfe criteria. For statistical analysis, the frequency, median, minimum and maximum values, the Wilcoxon test and the odds ratio were used. Multiple logistic regression was performed, using the stepwise selection, with a 5% significance level. RESULTS: the frequency of dense breasts was 45%. Women with dense breasts were of lower weight (60.5 vs. 71.9 kg - p<0.01), had a lower BMI (25.9 vs 31.0 kg/m² - p<0.01), a shorter time since onset of menopause (6.0 vs 10 years - p<0.01) and higher levels of FSH (75.2 vs 60.3 mU/mL - p<0.01). The probability of having dense breasts decreased in women whose weight was 67 kg or more (OR = 4.0, CI 95% = 1.50-10.66), BMI was higher than 30 kg/m² (OR = 6.69, CI 95% = 1.67-36.81), time since onset of menopause was superior or equal to seven years (OR = 2.05, CI 95% = 1.05-3.99) and FSH levels were lower than 134.8 mU/mL. CONCLUSION: weight, BMI, parity, time since menopause and FSH levels were significantly associated with mammographic density patterns.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2002;24(5):315-320
DOI 10.1590/S0100-72032002000500005
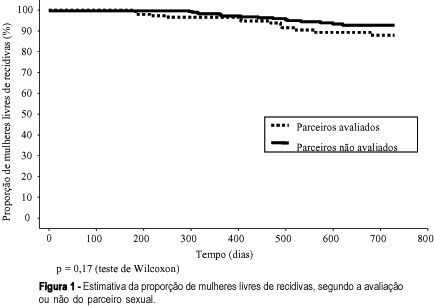
Purpose: to study the association between the evaluation or not of the male partner and relapses in women treated for HPV lesions. Methods: a reconstituted cohort study with 144 women with HPV lesions and whose partners had been evaluated, compared with 288 women whose partners had not been examined, controlled regarding date of attendance, age, lesion degree and treatment, attended between July 1993 and March 2000. We evaluated similarity between the groups, the association between the evaluation or not of the partners or the diagnosis of lesions with the occurrence and relapse lesion degree in the women and the disease-free interval (DFI). Results: the groups were similar regarding the control variables. Relapses occurred in 9.0 % of the women whose partners had been evaluated and in 5.9% of those whose partners had not been evaluated (p=0.23). When lesions were diagnosed in the men, 12.5% of their partners had relapses, against 7.3% of the women whose partners had no lesions (p=0.23), but there was no correlation with the relapse lesion degree and DFI. When the men reported a time of monogamous conjugal relationship <12 months, we observed 14.9% relapses in women, against 6.2% for the women whose partners reported a longer time (p=0.08). Conclusions: evaluation of the man did not decrease the relapse risk of HPV lesions in his partner. The presence of lesions in the male partners did not correlate with the occurrence and relapse degree in women and DFI. This study does not support the hypothesis that nonevaluated men would be an important cause of relapses in their partners.