Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2005;27(7):407-414
DOI 10.1590/S0100-72032005000700007
PURPOSE: to evaluate the prevalence of vulval squamous intraepithelial lesions and associated factors in HIV-infected patients attended at the public health services of Rio de Janeiro city. METHOD: a total of 374 HIV-infected patients were attended at public services in Rio de Janeiro city and submitted to gynecological examination, Pap smear and colposcopic examination of the cervix and vulva. The association of vulval intraepithelial lesion was analyzed according to the results of clinical (age and cervical lesions), laboratorial (CD4 count) and behavioral (number of partners and smoking habit) variables. The study (independent) variables were the epidemiological data, the immunologic status and the results of gynecological propaedeutic. Thus, age, the smoking habit, number of sexual partners, count of T CD4 lymphocites, and cervical intraepithelial lesion were selected. In the beginning, a bivariate analysis was performed, aiming at assessing the association between the presence of vulval intraepithelial lesion (ultimate variable) and the independent variables (age, smoking habits, number of sexual partners, cytology, colposcopy and CD4 count). Thereafter, the results with statistical significance (p<0.05) were submitted to a multiple logistic regression, and the probability ratio with the respective 95% confidence interval was established. RESULTS: the prevalence of vulval intraepithelial lesions was 40%. In the multivariate analysis CD4 count below 500 cells/mm³ OR=2.69 [IC 95%: 1.61-4.52], abnormal colposcopy OR=1.64 [IC 95%: 1.01-2.67] and age under 26 OR=1.98 [IC 95%: 1.18-3.30] were significant. In the vulval and cervical simultaneous lesion subgroup, age under 26 OR=3.30 [IC 95%: 1.65-6.59] and CD4 count below 500 cells/mm³ OR=4.15 [IC 95%: 1.92-8.96], were significant on analysis. CONCLUSIONS: the prevalence of vulval squamous intraepithelial lesions in HIV-infected patients is high. Immunodeficiency, presence of cervical intraepithelial lesions and age under 26 were associated with the presence of vulval intraepithelial lesions.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2005;27(7):415-420
DOI 10.1590/S0100-72032005000700008
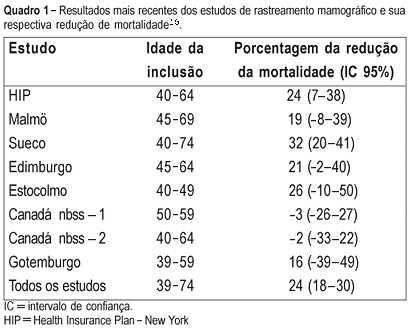
PURPOSE: to evaluate the cost of preventive mammographic screening in climacteric women, as compared to the cost of breast cancer treatment in more advanced stages. METHODS: one thousand and fourteen patients attended at the Climacteric outpatient service of the Gynecology Department, Federal University of São Paulo Paulista School of Medicine, were included in the study and submitted to mammographic test. All mammographic test's were analyzed by the same two physicians and classified according to the BI-RADS (Breast Imaging Reporting and Data System American College of Radiology) categories. The detected lesions were submitted to cytological and histological examination. RESULTS: the final diagnostic impression of the 1014 examinations, according to the classification of BI-RADS categories was: 1=261, 2=671, 3=59, 4=22 and 5=1. The invasive procedures were performed through a needle guided by ultrasound or stereotactic examinations: 33 fine-needle aspiration biopsies, 6 core biopsies guided by ultrasound and 20 core biopsies guided by stereotactic examination. Five cancer diagnoses were established. The total cost of this screening based on Brazilian procedure values was R$ 76,593.79 (25,534 dollars). Therefore, the cost of the diagnosis of the five cases of cancer in this screening was R$ 15,318.75 (5,106 dollars) each. However, the average cost per patient screened was R$ 75.53 (25 dollars). CONCLUSIONS: considering that the total treatment cost of only one case of breast cancer in advanced stage including hospital costs, surgery, chemotherapy, radiotherapy and hormonal treatment is similar to the cost of 1,000 mammographic screenings in climacteric women, it may be concluded that the cost of the early cancer diagnosis program is worth it and should be included in the public health program, as a way of lowering the public health expense.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2005;27(7):435-436
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2005;27(7):434-434
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2005;27(7):434-434
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2005;27(7):435-435