Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2014;36(12):531-534
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2014;36(12):535-540
DOI 10.1590/So100-720320140005086
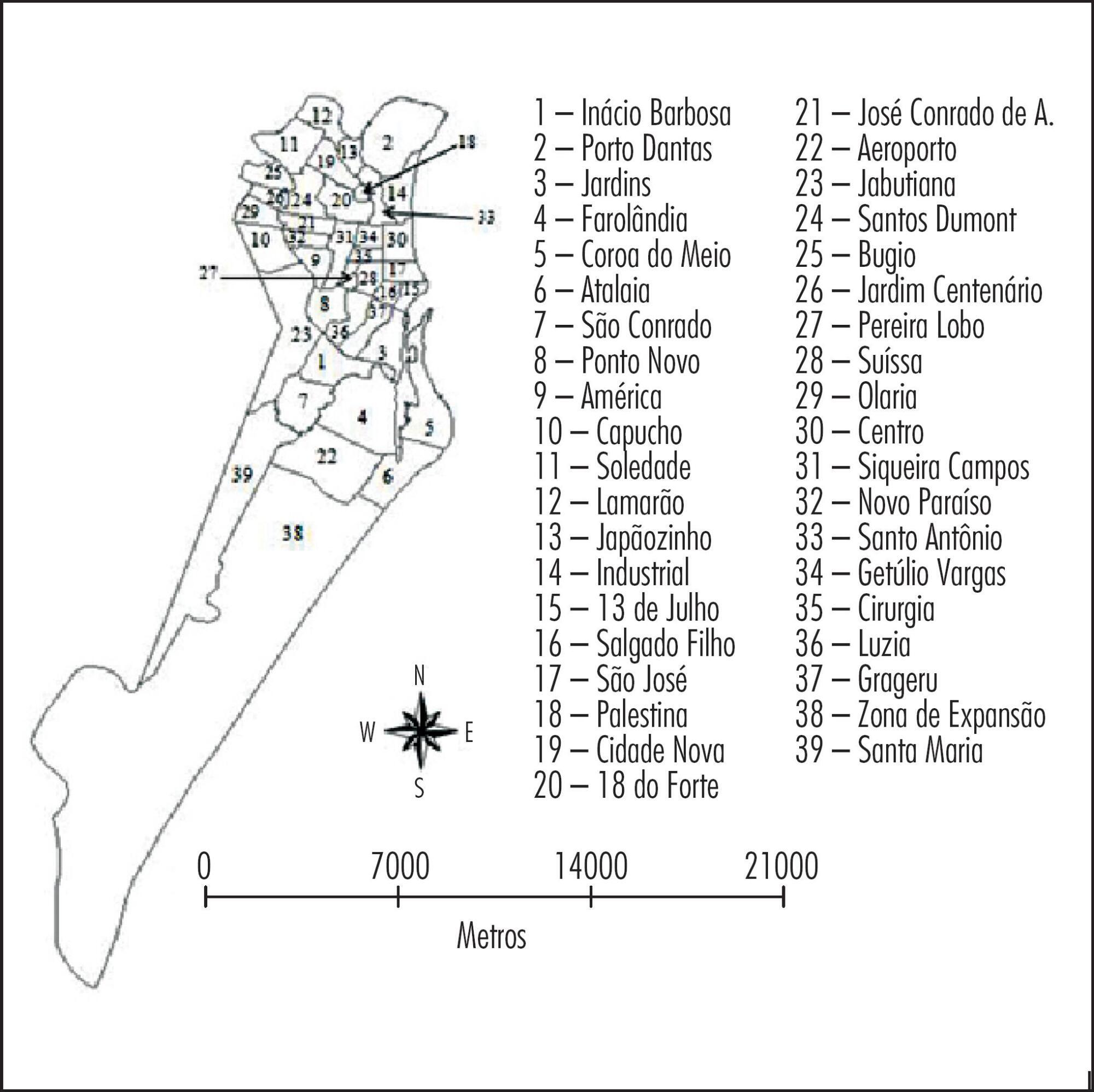
To analyze the spatial distribution of the prevalence of anti-toxoplasma gondii antibodies in pregnant women from a Brazilian Northeast city, and to correlate such prevalence with average maternal age and place of residence.
A descriptive, analytical and ecological study was conducted from January 1st to December 31st 2012. Data were obtained retrospectively from the Medical Specialties Center database and processed with the Epi info statistical package (Epi 7, Centers for Disease Control and Prevention, Atlanta, USA) and with Microsoft Excel 2010. The X2 test was applied to assess the association between the prevalence of antibodies to toxoplasma gondii and the average age. Spatial analysis of infection prevalence was performed using the TerraView software, version 4.2.2, with Kerneldensity estimation, which estimates the quantity of events through maps in order to identify areas with the highest concentration of cases in the city.
The seroprevalence of IgG was 68.5% (95%CI 67.2-69.8) and the prevalence of IgM was 0.36% (95%CI 0.23-0.6). A higher IgG prevalence was associated with increased age in the oldest neighborhoods of the state capital, whereas a higher IgG prevalence among younger women was detected in suburban neighborhoods. The spatial concentration of IgM antibodies was higher in suburban neighborhoods, with no significant correlation between seroprevalence and age.
Geoprocessing allowed the identification of areas with the highest prevalence, as well as the most susceptible average age and it was also useful as an instrument for the evaluation and implementation of appropriate preventive measures for this municipality and for other regions of Brazil.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2014;36(12):541-547
DOI 10.1590/So100-720320140005051
To identify the profile of use of medication during the first trimester of pregnancy with emphasis on safety assessment and on the adoption of folic acid and ferrous sulfate by pregnant women attended at a Basic Health Unit in Brazil.
This was a cross-sectional study nested in a cohort of pregnant women. Medications were classified according to the Anatomical Therapeutic Chemical (ATC), and their safety was evaluated according to the Food and Drug Administration (FDA) and the Brazilian Health Surveillance Agency (ANVISA). The adoption of ferrous sulfate and folic acid was investigated according to the protocol set forth by the Brazilian Ministry of Health.
The survey included 212 pregnant women, 46.7% of whom were taking medications at the time of pregnancy diagnosis, and 97.6% used medication during the first trimester after diagnosis. The highest percentage of self-medication occurred before the beginning of prenatal care (64.9%). According to the FDA criteria, there was a high level of exposure to D and X risk drugs before the beginning of prenatal care (23.0%), which was also observed for drugs not recommended by ANVISA (36.5%). Of the surveyed sample, 32.5% did not follow the protocol of the Brazilian Ministry of Health. In all, 67.9% of pregnant women had inadequate drug exposure. There was a difference between the proportions of drugs used according to the ATC, and the main anatomical groups identified were the drugs that act on blood and blood-forming organs, and anti-infective medications for systemic use. When pregnancy was diagnosed, the use of a large number of medications that act on the genitourinary system and sex hormones (16.2%) was identified, such as oral contraceptives, a fact probably related to the percentage of unplanned pregnancies (67.0%), on the same occasion 4 pregnant women used folic acid and 3 used ferrous sulphate.
The present results show that a large number of medications are used during pregnancy. Even if there was little exposure to drugs at the time of diagnosis, there is an overuse of potentially risky medications and self-medication during the first trimester of pregnancy.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2014;36(12):548-554
DOI 10.1590/So100-720320140005038
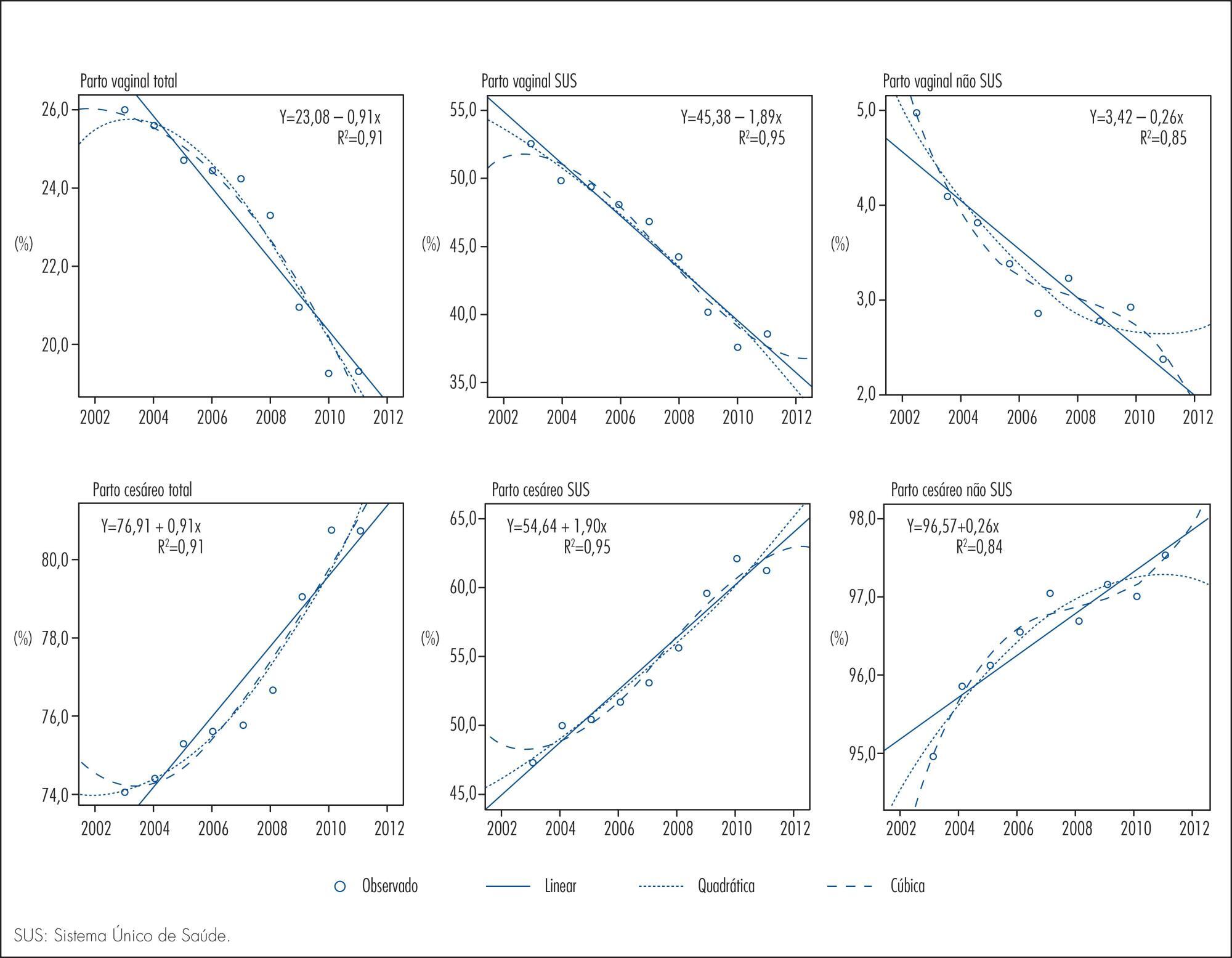
To analyze the time trend of the rates of cesarean and vaginal delivery according to the source of financing.
This was an ecological study of the time series analysis of cesarean and vaginal delivery rates according to the financing source, carried out in Maringá, Paraná State, Brazil, from 2002 to 2012. Information available at the System of Information on Live Births and at the System of Hospital Information of the Brazilian Unified Health System (SUS) was used for data collection. Moving averages were calculated for all mode of delivery rates in order to smooth random fluctuations in the series, dispersion diagrams were designed between the coefficients and years of the study, and polynomial regression models were estimated from the functional relation observed, with the level of significance set at p<0.05.
Throughout the 11 years of the study there were 48,210 births, 77.1% by cesarean delivery and only 22.9% by vaginal delivery. A total of 22,366 procedures were financed by SUS, 54.6% of them being cesareans. Trend analysis was significant for all the regression models, demonstrating an ascending trend for cesarean delivery and a descending trend for vaginal delivery for both types of financing. The non-SUS cesarean rates always exceeded 90.0% and were more frequent than the SUS cesarean rates, even with a 36.0% increase of the latter during the study period.
Based on trend analysis, cesarean deliveries will continue to increase in both health financing sources unless new actions and strategies of reduction are implemented, involving the sociocultural, demographic and obstetric characteristics of women, the training and activity of professionals in the area of obstetrics and an adequate structure of health services for providing vaginal delivery.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2014;36(12):555-561
DOI 10.1590/So100-720320140005155
To determine if illicit drug use increases the vertical transmission of HIV, to identify the risk factors involved in mother and child health and the prevalence of illicit drug use among these pregnant women.
Sixty-four (7.6%) of 845 pregnant women from the metropolitan region of Belo Horizonte, Minas Gerais, Brazil, attended in the service between October 1997 and February 2012 reported the use of illicit drugs. Cases were HIV-positive drug users (n=64) and controls were women who did not use drugs (n=192). Three controls were selected for each case. Several conditions of exposure were considered in the control group such as tobacco use, alcohol use, alcohol and tobacco use, maternal age, educational level, ethnicity, and marital status. Problems during the prenatal period, delivery and postpartum, vertical HIV transmission and neonatal outcomes were also investigated.
Univariate analysis showed as significant variables: maternal age, tobacco use, number of prenatal care visits, antiretroviral therapy, mode of infection, and viral load at delivery. Logistic regression revealed as significant variables: maternal age (less than 25 years); tobacco use, and number of prenatal care visits (less than 6). The vertical transmission of HIV was 4,8% (95%CI 1.7–13.3) among drug users and 2,1% (95%CI 0.8–5.2) in the control group, with no statistically significant difference between groups. Neonatal complications were more frequent among drug users, but also with no statistically significant difference between groups.
The use of illicit drug is frequent during pregnancy among HIV-infected women. The approach to illicit drug use should be routine during prenatal care visits. These women are more discriminated against and tend to deny their habits or do not seek prenatal care. There was no difference in vertical virus transmission between groups, probably indicating adherence to antiretroviral use for antiretroviral therapies during pregnancy.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2014;36(12):569-574
DOI 10.1590/SO100-720320140005068
The aim of this study was to evaluate the clinical features and prognostic implications of patients with recurrent cervical cancer.
By reviewing the medical records we evaluated all patients with cervical cancer at stages IA to IVA who started treatment at a specialized hospital in the Southeast region of Brazil from 2007 to 2009. Recurrence episodes were categorized according to location of disease and information was collected regarding the type of treatment and survival of these patients. The sample was characterized by descriptive statistics and association analyses were performed using Fisher's exact test.
Fifty cases of recurrence were identified among 469 selected records, with 31 patients being symptomatic at diagnosis of recurrence (62%); and 19 being asymptomatic (38%). Among women with symptoms, eight requested anticipation of the previously scheduled appointment because of the presence of clinical complaints. Patients with symptoms at the diagnosis of recurrence had lower rates of overall two-year survival (39.4 versus 67.6%) (p=0.081). None of the patients with recurrence at distance received curative intent treatment, but all received surgical treatment or radiotherapy aiming at full remission of the disease. Women who requested anticipation of the appointment because of the presence of symptoms had a significant reduction of overall two-year survival after recurrence (0 versus 60.4%; p<0.001) compared to those who attended the consultation on the scheduled date, and none of them received curative intent treatment. As expected, the patients who underwent palliative treatment with the main objective of improving quality of life and increasing survival but with no perspective of cure had a significant reduction in overall survival compared to those who were treated with curative intent (76.7 versus 35.4%; p<0.001).
The benefit of detecting asymptomatic recurrence of cervical cancer has the potential to improve the prognosis of patients with local and regional recurrence, but studies on larger series are necessary to confirm this possibility.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2014;36(12):575-580
DOI 10.1590/SO100-720320140005158
To compare the distributions of patients with clinical-pathological subtypes of luminal B-like breast cancer according to the 2011 and 2013 St. Gallen International Breast Cancer Conference Expert Panel.
We studied 142 women with breast cancer who were positive to estrogen receptor and had been treated in São Paulo state, southeast Brazil. The expression of the following receptors was assessed by immunohistochemistry: estrogen, progesterone (PR) and Ki-67. The expression of HER-2 was measured by fluorescent in situ hybridization analysis in tissue microarray.
There were 29 cases of luminal A breast cancers according to the 2011 St. Gallen International Breast Cancer Conference Expert Panel that were classified as luminal B-like in the 2013 version. Among the 65 luminal B-like breast cancer cases, 29 (45%) were previous luminal A tumors, 15 cases (20%) had a Ki-67 >14% and were at least 20% PR positive and 21 cases (35%) had Ki-67 >14% and more than 20% were PR positive.
The 2013 St. Gallen consensus updated the definition of intrinsic molecular subtypes and increased the number of patients classified as having luminal B-like breast cancer in our series, for whom the use of cytotoxic drugs will probably be proposed with additional treatment cost.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2014;36(12):562-568
DOI 10.1590/SO100-720320140005161
To verify the existence of associations between different maternal ages and the perinatal outcomes of preterm birth and intrauterine growth restriction in the city of São Luís, Maranhão, Northeastern Brazil.
A cross-sectional study using a sample of 5,063 hospital births was conducted in São Luís, from January to December 2010. The participants comprise the birth cohort for the study "Etiological factors of preterm birth and consequences of perinatal factors for infant health: birth cohorts from two Brazilian cities" (BRISA). Frequencies and 95% confidence intervals were used to describe the results. Multiple logistic regression models were applied to assess the adjusted odds ratio (OR) of maternal age associated with the following outcomes: preterm birth and intrauterine growth restriction.
The percentage of early teenage pregnancy (12–15 years old) was 2.2%, and of late (16–19 years old) was 16.4%, while pregnancy at an advanced maternal age (>35 years) was 5.9%. Multivariate analyses showed a statistically significant increase in preterm births among females aged 12–15 years old (OR=1.6; p=0.04) compared with those aged 20–35 years. There was also a higher rate in preterm births among females aged 16–19 years old (OR=1.3; p=0.01). Among those with advanced maternal age (>35 years old), the increase in the prevalence of preterm birth had only borderline statistical significance (OR=1.4; p=0.05). There was no statistically significant association between maternal age and increased prevalence of intrauterine growth restriction.