Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2002;24(6):365-370
DOI 10.1590/S0100-72032002000600002
Purpose: to study the relationship between pelvic floor function and bladder neck mobility in women with and without stress urinary incontinence (SUI), in menacme and postmenopausal. Methods: sixty-one SUI patients were evaluated; 31 of them were in menacme and of these 17 had SUI and 14 did not have any complaint; 30 were postmenopausal and of these, 15 with SUI and 15 without SUI. Simple cystometry and empty supine stress test were performed in those who had urinary incontinence complaint. Bladder neck mobility was studied by ultrasound and by the Q-tip test. To study pelvic floor function, vaginal cones and digital palpation were used. Results: the bladder neck position in the incontinent women (Groups A and C), determined by ultrasound or the Q tip-test, was --11.8 cm in Group A and --12.5 cm in Group C, lower than the continent women, in whom the bladder neck was at +4.4 cm in Group B and +2.3 cm in Group D. There were no differences in bladder neck mobility among the continent menacme (9.1 cm) and postmenopausal (9.5 cm) groups. Also there were no differences among the incontinent groups (17.1 cm for Group A and 16.6 cm for Group C). The bladder neck mobility was greater in the incontinent women (A and C). Continent women had better results on evaluation of pelvic floor muscles than the incontinent ones, even using vaginal cones or digital palpation, and these results were not dependent on the hormonal status. Conclusion: a positive correlation was found between the Q-tip tests and ultrasound, and between test with vaginal cones and digital palpation. No significant correlation was found between pelvic floor function and bladder neck mobility.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2002;24(5):315-320
DOI 10.1590/S0100-72032002000500005
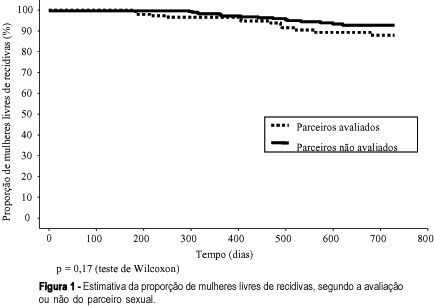
Purpose: to study the association between the evaluation or not of the male partner and relapses in women treated for HPV lesions. Methods: a reconstituted cohort study with 144 women with HPV lesions and whose partners had been evaluated, compared with 288 women whose partners had not been examined, controlled regarding date of attendance, age, lesion degree and treatment, attended between July 1993 and March 2000. We evaluated similarity between the groups, the association between the evaluation or not of the partners or the diagnosis of lesions with the occurrence and relapse lesion degree in the women and the disease-free interval (DFI). Results: the groups were similar regarding the control variables. Relapses occurred in 9.0 % of the women whose partners had been evaluated and in 5.9% of those whose partners had not been evaluated (p=0.23). When lesions were diagnosed in the men, 12.5% of their partners had relapses, against 7.3% of the women whose partners had no lesions (p=0.23), but there was no correlation with the relapse lesion degree and DFI. When the men reported a time of monogamous conjugal relationship <12 months, we observed 14.9% relapses in women, against 6.2% for the women whose partners reported a longer time (p=0.08). Conclusions: evaluation of the man did not decrease the relapse risk of HPV lesions in his partner. The presence of lesions in the male partners did not correlate with the occurrence and relapse degree in women and DFI. This study does not support the hypothesis that nonevaluated men would be an important cause of relapses in their partners.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2002;24(5):337-341
DOI 10.1590/S0100-72032002000500008
Purpose: to evaluate pregnancy outcome after laparoscopic tubal anastomosis. Method: from December 1998 to December 2001, 26 patients with bilateral tubal ligation who underwent laparoscopic tubal anastomosis were prospectively evaluated. Patients' age ranged from 28 to 37 years. The follow-up period ranged from 150 to 425 days and tubal patency (evaluated by hysterosalpingography) and pregnancy outcome were evaluated. Results: laparoscopic tubal reversal was performed in 23 patients. Bilateral reversal was attempted in all except two patients. The operation time ranged from 95 to 155 minutes and all patients were discharged on the following morning. Tubal patency was confirmed in 15 patients (15/23). Pregnancy rate was 56.5% (13/23), without ectopic pregnancies. Nine patients got pregnant in up to four months and four in up to nine months after discontinuing the use of condom. Conclusion: in selected cases, laparoscopic tubal reversal can be performed in patients who had been submitted to tubal sterilization and desire new pregnancies. Patient selection as well as meticulous surgical technique are key factors in achieving satisfactory pregnancy rates.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2002;24(5):329-334
DOI 10.1590/S0100-72032002000500007
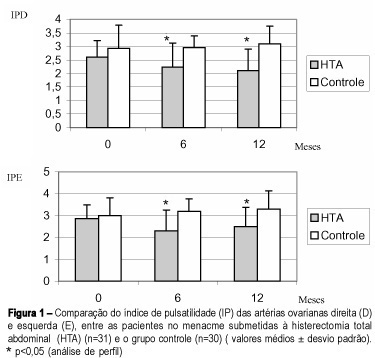
Purpose: to evaluate the effect of total abdominal hysterectomy on ovarian blood supply in women in reproductive age, using transvaginal color Doppler. Methods: a prospective study was carried out on 61 40-year-old or younger women. They were divided into two groups: G1, 31 patients submitted to hysterectomy, and G2, 30 normal women. Criteria of inclusion: normal ovarian function at baseline, normal body weight, without expasure to tobacco, no history of laparotomy or ovarian pathology. The pulsatility index (PI) of ovarian arteries determined by Doppler and the transvaginal ultrasonographic measurement of the ovarian volume were performed at three moments: baseline, 6 and 12 months. Results: at baseline the groups were homogeneous. In the hysterectomized group, with 6 and 12 months, increase of the volume of the ovaries and decrease of PI (p<0,05) were observed. At the end of the study, 25.5% (8/31) of the hysterectomized patients presented benign ovarian cysts. In the control group no alteration of the parameters was observed. Conclusion: The decrease of PI by Doppler of ovarian arteries suggests increased ovarian blood supply after total abdominal hysterectomy in women in reproductive age.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2002;24(5):323-327
DOI 10.1590/S0100-72032002000500006
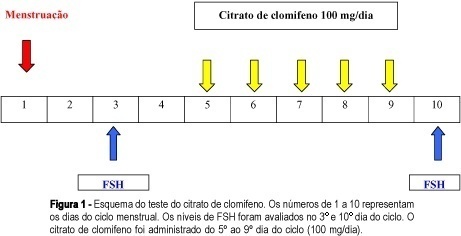
Purpose: to assess ovarian reserve by FSH determination on the 3rd day of the menstrual cycle compared to the clomiphene test and to correlate the results with the ovarian response to controlled hyperstimulation with gonadotrophins for in vitro fertilization. Methods: a total of 49 patients older than 30 years who had been presenting a clinical picture of infertility for at least 1 year were selected. All patients were evaluated for ovarian reserve by the clomiphene citrate test and 26 of them were later submitted to controlled ovarian hyperstimulation with gonadotrophins. Of these 26 patients, 18 showed a good response to ovarian hyperstimulation and 8 showed a poor response. Mean (+ SD) FSH values were calculated for the determinations on the 3rd and on the 10th day and for their sum in the group of patients who responded favorably to ovarian stimulation, and were later correlated with the ovarian response after gonadotrophin stimulation. Results: employing a FSH value > 16.1 IU/mL on the 10th day (mean plus 2 SD) for the prediction of a poor ovarian response in the clomiphene test, the sensitivity, specificity, and positive and negative predictive values of this parameter were 50, 100, 100 and 81.8%, respectively. Considering the clomiphene test to be positive when the sum of the FSH values determined on the 3rd and 10th day plus 2 SD was > 22.6 IU/mL, we obtained 62.5% sensitivity 100% specificity, 100% positive predictive value, and 85.7% negative predictive value. A single FSH determination of 10 IU/mL on the 3rd day of the cycle for the prediction of a poor ovarian response showed 87% sensitivity, 100% specificity, 100% positive predictive value and 94.7% negative predictive value. Conclusion: in the present study, a single FSH determination on the 3rd day of the cycle showed to be more sensitive than the clomiphene test for the evaluation of ovarian reserve.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2002;24(5):309-313
DOI 10.1590/S0100-72032002000500004
Purpose: to evaluate the importance of endometrial thickness measurement as an orienting factor for the clinical treatment of unruptured tubal pregnancy. Method: longitudinal observational study, in which the greatest measure of the endometrial thickness was evaluated in millimeters, in the uterine longitudinal axis, through transvaginal ultrasonography. Our study group included 181 patients, all of them respecting the utilization criteria for the clinical treatment (expectant or medicated with methotrexate). Through Student's t test we evaluated the difference between the average thickness of the cases who presented successful results with the treatment and the average of those who failed. Results: the average endometrial thickness of the patients who presented successful results with the medical treatment (31 cases) was 6.4 mm, while the average in the cases of failure was 11.5 mm. These results were significantly different. The average thickness of the successful group with expectant management (128 cases) was 9.0 mm, while the average of those who failed was 9.6 mm. These values were not statistically different. Conclusions: the greatest measure of the endometrial thickness of the uterine longitudinal axis through transvaginal ultrasonography proved to be valuable as a new orienting factor for the medical treatment of patients with a diagnosis of unruptured tubal pregnancy. It may become a useful and auxiliary tool for the recommendation of the use of methotrexate. On the other hand, thickness did not show to be useful as an orienting factor for establishing expectant management.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2002;24(5):301-306
DOI 10.1590/S0100-72032002000500003
Purpose: to compare the outcome of pregnancies with and without threatened abortion presenting alive embryo/fetus between 6 and 13 weeks at sonographic evaluation. Method: this was a retrospective case-control study, carried out from February 1998 to December 1999. Criteria for inclusion were: topic and single pregnancy; embryo/fetus cardiac activity present in the ultrasound scan; gestational age between 6 weeks and 13 weeks and 6 days, absence of fetal anomalies, absence of attempt of abortion by drugs or manipulation, absence of maternal disease, known pregnancy result. A total of 1531 pregnancies were examined, of which 258 with threatened abortion (case group) and 1273 without threatened abortion (control group). The two groups were compared regarding outcome such as: abortion, stillbirth, prematurity and intrauterine growth restriction. Results: the percentage of abortion (11,7%) and prematurity (17,8%) were higher in the group with threatened abortion (p<0.001 and p=0.026, respectively). The frequency of stillbirth and intrauterine growth restriction did not differ significantly between the groups.Conclusion: threatened abortion with alive embryo/fetus in 6- to 13- week gestation presented a higher abortion risk and subsequent prematurity.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2002;24(5):293-299
DOI 10.1590/S0100-72032002000500002
Purpose: to study the prenatal care among Public Health Service ("Sistema Único de Saúde") users from Caxias do Sul - RS. Methods: a transversal study of 702 pregnancies attended at the Hospital Geral -Universidade de Caxias do Sul from March 2000 to March 2001 based on the criteria set by the "Programa Nacional de Humanização do Pré-natal e Nascimento (PNHPN)" of the Brazilian Ministry of Health. Results: the observed prenatal coverage was 95.4%, whereas the average of visits was 6.2. The main reported reason for not following prenatal care was the lack of information about its importance (65.6%). In 51.5% of the cases, prenatal care started in the third month of pregnancy, whereas 44.3% of the pregnant women carried out all the proposed complementary tests. Prenatal care was considered inappropriate in 64.8% and appropriate in 35.2% of the cases. The quality of prenatal attention was significantly associated with the mother's education, as well as with the number of previous deliveries. The higher the educational level, the better the quality of observed prenatal care (p=0.0148). In addition, the higher number of previous deliveries showed to be associated with a later beginning of prenatal care and a lower number of visits (p=0.0008). Conclusions: the prenatal care available at Caxias do Sul in spite of its good coverage, should be reviewed in terms of quality. Special attention should be given to education in health along the prenatal assistance.