Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2018;40(1):20-25
To validate the premenstrual symptoms screening tool (PSST) in relation to the daily record of severity of problems (DRSP) for premenstrual syndrome (PMS) and premenstrual dysphoric disorder (PMDD) diagnoses.
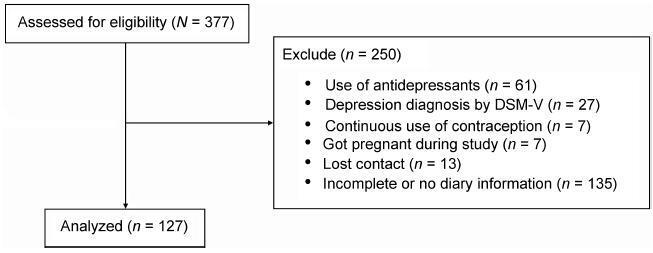
A cross-sectional study with 127 women (20 45 years) with PMS complaints. The women were evaluated in terms of weight, height and body mass index (BMI). After using the primary care evaluation of mental disorders (PRIME-MD) questionnaire to exclude the diagnosis of depression, the PSST was completed and the women were instructed to fill out the DRSP for two consecutive menstrual cycles. The agreement between the two questionnaires was assessed by the Kappa (k) and the prevalence-adjusted, bias-adjusted kappa (PABAK) values.
Two-hundred and eighty-two women met the eligibility criteria and answered the PSST. The DRSP was completed for two cycles by 127 women. The percentages of women with PMS and PMDD diagnoses by the DRSP were 74.8% and 3.9% respectively; by PSST, the percentages were41.7% and 34.6% respectively. The number of patients considered "normal" (with symptoms below the threshold for the diagnosis of PMS) was similar in both questionnaires. There was no agreement (Kappa = 0.12) in the results of PMS/ PMDD diagnosis (the PABAK coefficient confirmed this result = 0.39). The PSST had a high sensitivity (79%) and a low specificity (33.3%) for PMS/PMDD diagnosis.
The PSST should be considered a diagnostic screening tool. Positive PMS/PMDD cases by PSST should be further evaluated by DRSP to confirm the diagnosis.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2018;40(1):26-31
A vulvar squamous intraepithelial lesion is deemed to be a preceding lesion to vulvar cancer, especially in women aged under 40 years, holders of an acquired or idiopathic immunosuppression. Several treatments have been used to treat these lesions. One of the aesthetically acceptable therapeutic methods is the CO2 laser vaporization.
In a transversal study, 46 records of immunosuppressed women bearing a vulvar low grade and/or high grade squamous intraepithelial lesion were selected out of the retrospective analysis, computing age, date of record, date of vulvar lesion treatment with CO2 laser, the time elapsed between the first and the last visit (in months), the number of visits, the presence or absence of condylomatous lesions in other female lower genital tract sites and whether or not recurrences and persistence of intraepithelial lesions have been noticed during the follow-up.
Patients bearing vulvar high-grade squamous intraepithelial lesion and immunosuppressed (serumpositive forhumanimmunodeficiency virus [HIV] or with solid organs transplantation) have shown a higher level of persistence of lesions and a higher chance of having other areas of the female lower genital tract involved.
While the CO2 laser vaporization is the most conservative method for the treatment of vulvar high-grade intraepithelial lesions, it is far frombeing the ideal method, dueto the intrinsic infection features considered. The possibility of persistence, recurrences and spontaneous limited regression indicates that a closer surveillance in the long-term treated cases should be considered, in special for immunosuppressed patients.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2018;40(1):11-19
To evaluate the relation between changes the body mass index (BMI) percentile, reflected in the Atalah curve, and perinatal outcomes.
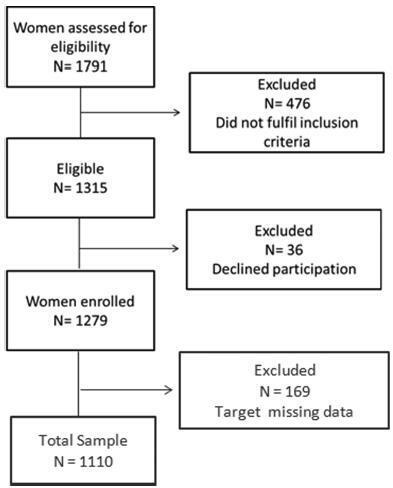
A cross-sectional study with 1,279 women was performed. Data regarding gestational weight, sociodemographic characteristics and perinatal outcomes were collected through medical charts, prenatal card and interviews in the postpartum period. Women could be classified according to the Atalah curve in the following categories: low weight, adequateweight, overweight, and obese. The BMIwas calculated at the first and at the last prenatal care visits, and these values were compared.
An increase in the BMI category according to the Atalah classification occurred in 19.9% of pregnant women, and an increase of 3.4, 5.8 and 6.4 points of BMI were found for women respectively classified in the adequate weight, overweight and obese categories at the first prenatal visit. Women with high school education presented a lower chance of increasing their BMI (odds ratio [OR] 0:47 [0.24- 0.95]). Women who evolved with an increase in the the Atalah classification were associated with cesarean section (OR 1.97-2.28), fetalmacrosomia (OR 4.13-12.54) and large for gestational age newborn (OR 2.88-9.83).
Pregnant women who gained enough weight to move up in their BMI classification according to the Atalah curve had a higher chance of cesarean section and macrosomia. Women classified as obese, according to the Atalah curve, at the first prenatal visit had a high chance of cesarean section and delivering a large for gestational age newborn.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2018;40(1):04-10
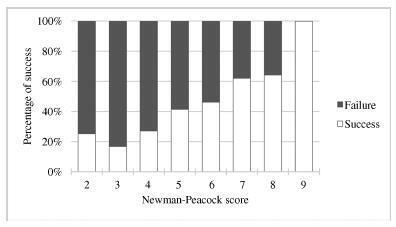
External cephalic version (ECV) is a maneuver that enables the rotation of the non-cephalic fetus to a cephalic presentation. The Newman-Peacock (NP) index, which was proposed by Newman et al. in a study published in 1993, was described as a prediction tool of the success of this procedure; it was validated in a North-American population, and three prognostic groups were identified.
To evaluate the value of the NP score for the prediction of a successful ECV in a Portuguese obstetrical population, and to evaluate maternal and fetal safety.
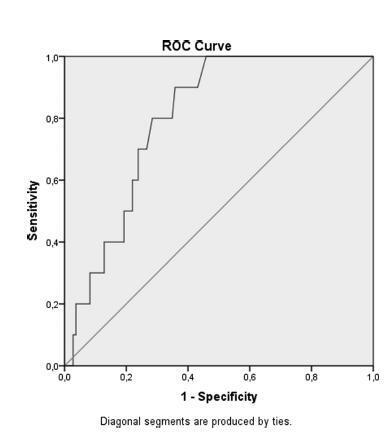
We present an observational study conducted from 1997-2016 with pregnant women at 36-38 weeks of pregnancy who were candidates for external cephalic version in our department. Demographic and obstetrical data were collected, including the parameters included in the NP index (parity, cervical dilatation, estimated fetal weight, placental location and fetal station). The calculation of the NP score was performed, and the percentages of success were compared among the three prognostic groups and with the original study by Newman et al. The performance of the score was determined using the Student t-test, the Chi-squared test, and a receiver operating characteristic (ROC) curve.
In total, 337 women were included. The overall success rate was of 43.6%. The univariate analysis revealed that multiparity, posterior placentation and a less engaged fetus were factors that favored a successful maneuver (p < 0.05). Moreover, a higher amniotic fluid index was also a relevant predictive factor (p < 0.05). The Newman-Peacock score had a poorer performance in our population compared with that of the sample of the original study, but we still found a positive relationship between higher scores and higher prediction of success (p < 0.001). No fetal or maternal morbidities were registered.
The Newman-Peacock score had a poorer performance among our population compared to its performance in the original study, but the results suggest that this score is still a useful tool to guide our clinical practice and counsel the candidate regarding ECV.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2017;39(5):229-234
Preoperatively identification of malignancy potential of a postmenopausal adnexal masses is important.
To evaluate the effectiveness of the Risk of Malignancy Index-2 in presumably benign adnexal masses in postmenopausal women.
Retrospective, observational study.
119 women with postmenopausal adnexal masses with a preliminary diagnosis of benign tumors according to the Risk of Malignancy Index-2 were included. Age, duration of menopause, ultrasonographic findings, and serum CA-125 levels were recorded preoperatively. The definitive diagnosis was based on postoperative histopathological examination.
Of 119 adnexal mass, 10 were malignant and 109 were benign. There was no statistically significant difference with regard to age and tumor size between the groups. The two significant ultrasonographic parameter between groups were the presence of solid area in the mass and bilaterality. Moreover, if the cut off point for serum CA-125 was adjusted to 14.75 IU/mL according to ROC curve, a sensitivity value of 80% and a specificity value of 72% could be achieved to discriminate benign and malign cysts.
In the differential diagnosis of benign and malignant adnexal masses in postmenopausal women, the presence of a solid component, bilaterallity based on ultrasonography and high CA-125 values may be used as discriminative criteria. There is no direct relation between the size of the adnexal mass and malignancy potential. Therefore, in the malignancy indexes of postmenopausal women, we recommend lower cut-off values of CA-125 to increase the sensitivity of preoperative evaluation tests without having a great impact on negative predictive values.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2017;39(5):224-228
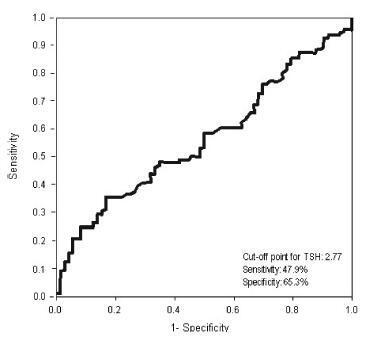
This study analyzed the effectiveness of the thyroid-stimulating hormone (TSH) as a predictor of insulin resistance (IR) and its association with the clinical and metabolic parameters of women with polycystic ovary syndrome (PCOS) without overt hypothyroidism.
A cross-sectional study was performed. Women with PCOS and without overt hypothyroidism (n = 168) were included.
Receiver operating characteristic (ROC) curve was used to determine the cut-off point for TSH that would maximize sensitivity and specificity for a diagnosis of IR using homeostatic model assessment of insulin resistance (HOMA-IR)≥ 2.71. Clinical and metabolic parameters were compared as a function of the TSH cut-off limit and the presence of IR.
Thyroid-stimulating hormone ≥ 2.77 mIU/L was associated with a diagnosis of IR, with sensitivity of 47.9% and specificity of 65.3%. There were no differences in clinical, hormonal or metabolic parameters between TSH < 2.77 and TSH of 2.77 - 10 mIU/L.
In women with PCOS without overt hypothyroidism, TSH ≥2.77 mIU/L is associated with IR; however, with poor sensibility, showing TSH to be a poor predictor of IR in this population. No clinical or metabolic alterations were found that would justify a change in clinical management. Thus, the IR should be investigated in all women with PCOS irrespective of TSH level.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2017;39(5):217-223
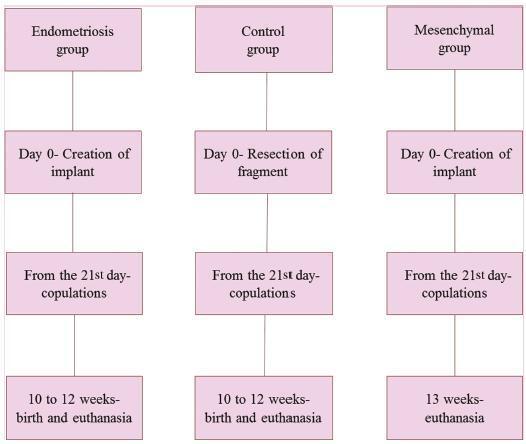
To evaluate the effect of mesenchymal stem cells (MSCs) on fertility in experimental retrocervical endometriosis.
A total of 27 New Zealand rabbits were divided into three groups: endometriosis, in which endometrial implants were created; mesenchymal, in which MSCs were applied in addition to the creation of endometrial implants; and control, the group without endometriosis. Fisher’s exact test was performed to compare the dichotomous qualitative variables among the groups. The quantitative variables were compared by the nonparametric Mann-Whitney and Kruskal-Wallis tests. The MannWhitney test was used for post-hoc multiple comparison with Boniferroni correction.
Regarding the beginning of the fertile period, the three groups had medians of 14±12.7, 40±5, and 33±8.9 days respectively (p = 0.005). With regard to fertility (number of pregnancies), the endometriosis and control groups showed a rate of 77.78%, whereas the mesenchymal group showed a rate of 11.20% (p = 0.015). No differences in Keenan’s histological classification were observed among the groups (p = 0.730). With regard to the macroscopic appearance of the lesions, the mesenchymal group showed the most pelvic adhesions.
The use of MSCs in endometriosis negatively contributed to fertility, suggesting the role of these cells in the development of this disease.