Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2015;37(9):411-416
DOI 10.1590/SO100-720320150005397
The aim of this study was to evaluate serum levels of inducible nitric oxide synthase (INOS), myeloperoxidase (MPO), total antioxidant status (TAS), and total oxidative status (TOS) in women with primary ovarian insufficiency (POI) and to compare them with healthy fertile women. We also examined the possible risk factors associated with POI.
This cross-sectional case control study was conducted in Zekai Tahir Burak Women's Health Education and Research Hospital. The study population consisted of 44 women with POI (study group) and 36 healthy fertile women (control group). In all patients, serum levels of INOS, MPO, TAS, and TOS were determined. INOS and MPO levels were measured by enzyme-linked immunosorbent assay whereas colorimetric method was used for evaluating TAS and TOS levels. Age, body mass index (BMI), obstetric history, smoking status, family history, comorbidities, sonographic findings, complete blood count values, C-reactive protein and baseline hormone levels were also analyzed. Student's t-test or Mann-Whitney U test was used to compare continuous variables between the groups; categorical data were evaluated by using Pearson χ2 or Fisher exact test, when appropriate. Binary logistic regression method was used to identify risk factors for POI.
We found significantly elevated levels of INOS (234.1±749.5 versus133.8±143.0; p=0.005), MPO (3,438.7±1,228.6 versus 2,481.9±1,230.1; p=0.001), and TOS (4.3±1.4 versus 3.6±1.4; p=0.02) in the sera of the study group when compared to the BMI-age matched control group. However, difference in serum levels of TAS were not significant between the 2 groups (1.7±0.2 versus 1.6±0.2; p=0.15). Logistic regression method demonstrated that BMI <25 kg/m2, nulliparity, family history of POI, smoking, and elevated serum levels of INOS, MPO, and TOS were independent risk factors for POI.
We found an increase in INOS, MPO, and TOS in women with POI. These serum markers may be promising in early diagnosis of POI. Further large-scale studies are required to determine whether oxidative stress markers have a role in diagnosing POI.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2015;37(6):283-290
DOI 10.1590/SO100-720320150005292
To determine the basic expression of ABC transporters in an epithelial ovarian cancer cell line, and to investigate whether low concentrations of acetaminophen and ibuprofen inhibited the growth of this cell line in vitro.
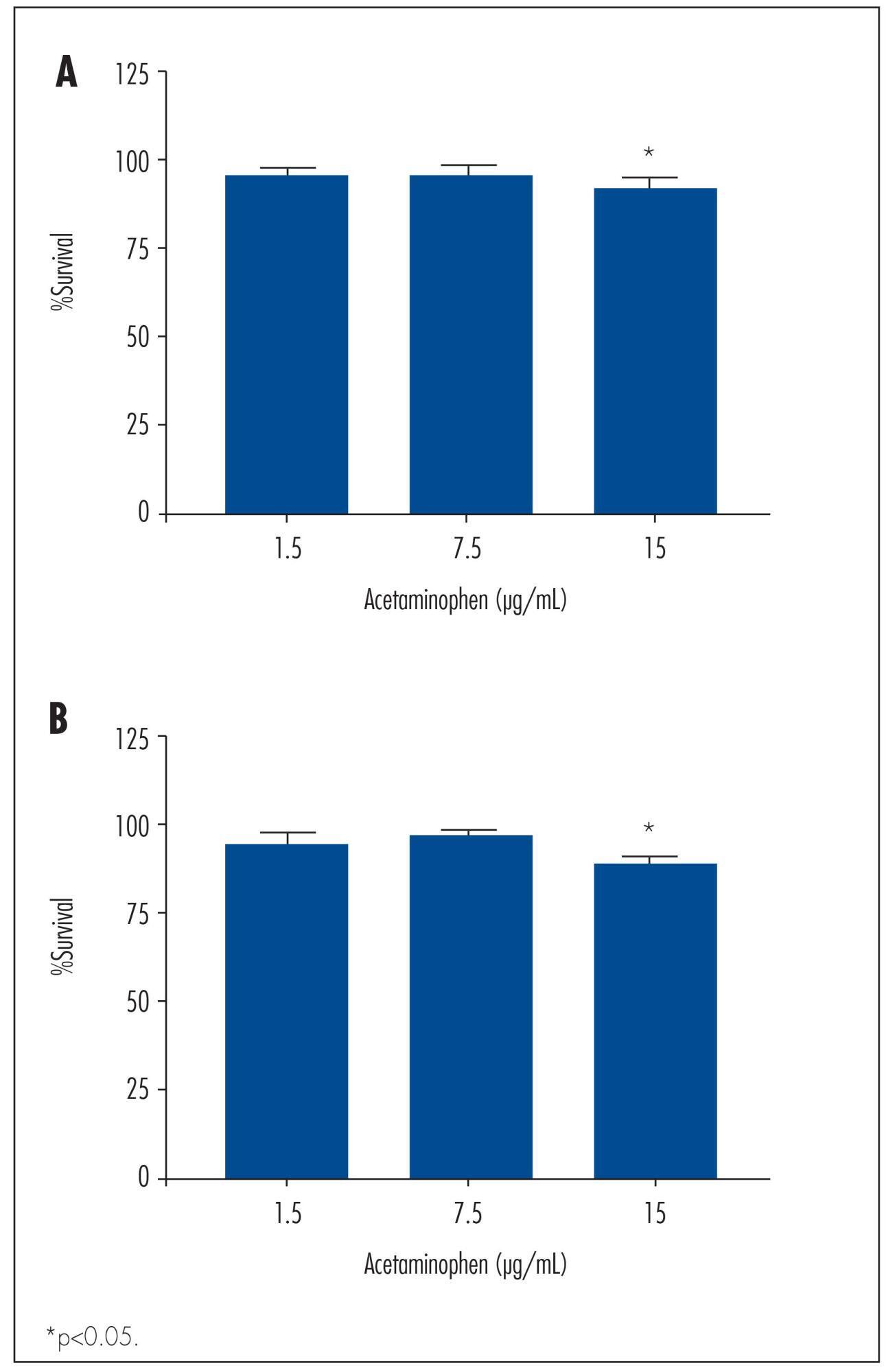
TOV-21 G cells were exposed to different concentrations of acetaminophen (1.5 to 15 μg/mL) and ibuprofen (2.0 to 20 μg/mL) for 24 to 48 hours. The cellular growth was assessed using a cell viability assay. Cellular morphology was determined by fluorescence microscopy. The gene expression profile of ABC transporters was determined by assessing a panel including 42 genes of the ABC transporter superfamily.
We observed a significant decrease in TOV-21 G cell growth after exposure to 15 μg/mL of acetaminophen for 24 (p=0.02) and 48 hours (p=0.01), or to 20 μg/mL of ibuprofen for 48 hours (p=0.04). Assessing the morphology of TOV-21 G cells did not reveal evidence of extensive apoptosis. TOV-21 G cells had a reduced expression of the genes ABCA1, ABCC3, ABCC4, ABCD3, ABCD4 and ABCE1 within the ABC transporter superfamily.
This study provides in vitro evidence of inhibitory effects of growth in therapeutic concentrations of acetaminophen and ibuprofen on TOV-21 G cells. Additionally, TOV-21 G cells presented a reduced expression of the ABCA1, ABCC3, ABCC4, ABCD3, ABCD4 and ABCE1 transporters.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2015;37(6):258-265
DOI 10.1590/SO100-720320150005366
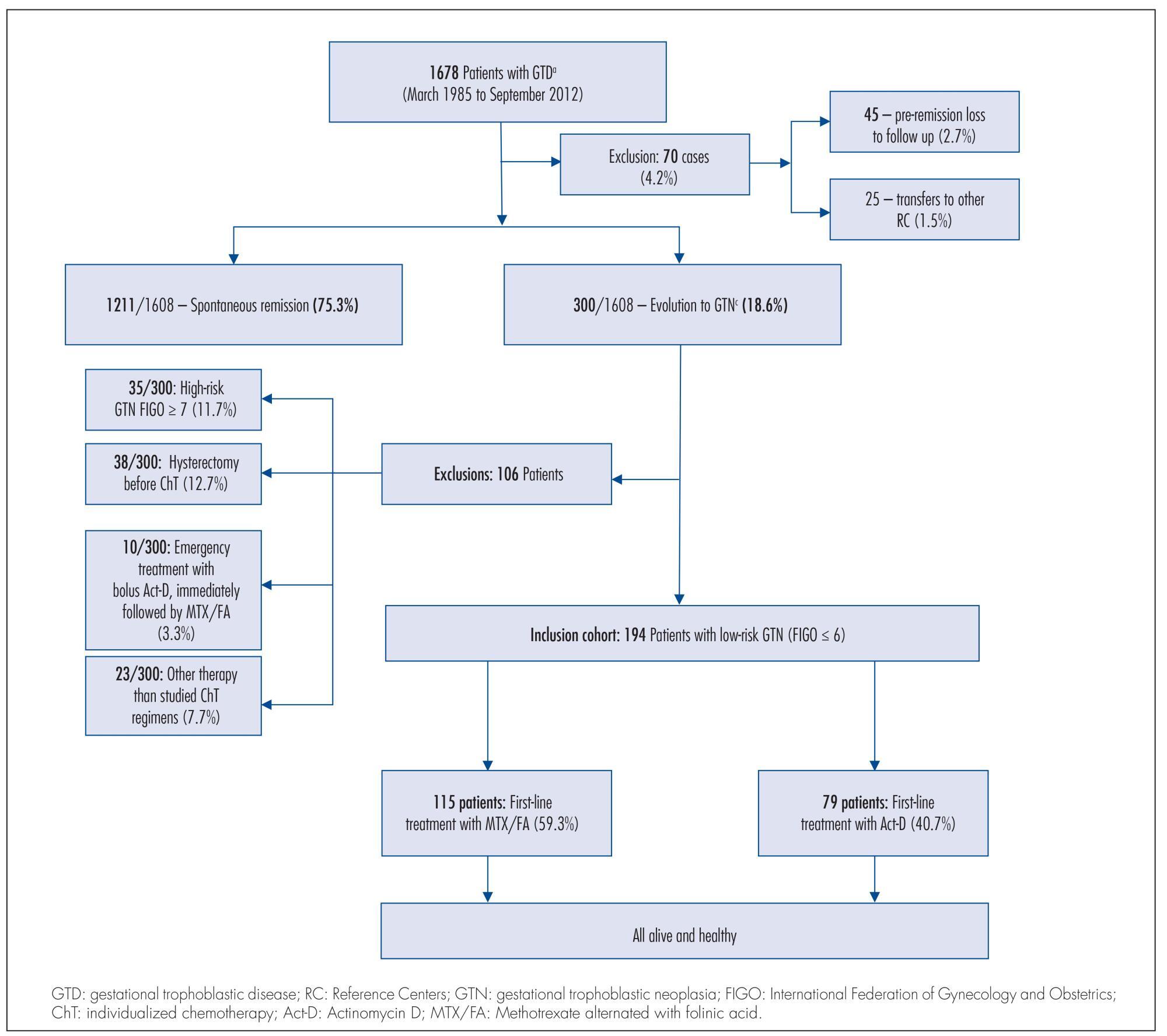
To compare two single-agent chemotherapy (ChT) regimens evaluating, in first-line treatment, response and side effects and, in final single-agent treatment, the outcomes, among Brazilian patients with low-risk gestational trophoblastic neoplasia (GTN), according to International Federation of Gynecology and Obstetrics (FIGO) 2002.
Retrospective analysis of two concurrent cohorts with 194 low-risk GTN patients: from 1992 to 2012, as first-line treatment, 115 patients received 4 intramuscular doses of methotrexate alternated with 4 oral doses of folinic acid (MTX/FA) repetead every 14 days and, since 1996, 79 patients received an endovenous bolus-dose of actinomycin D (Act-D), biweekly. At GTN diagnosis, patient opinion was taken into consideration when defining the initial single-agent ChT regimen, and when there was resistance or toxicity to one regimen, the other drug was used preferentially. This study was approved by the Irmandade da Santa Casa de Misericórdia de Porto Alegre Ethical Committee.
Both groups were clinically similar (p>0.05). In first-line treatments, frequency of complete response was similar (75.7% with MTX/FA and 67.1% with bolus Act-D); the number of ChT courses -median 3 (range: 1-10) with MTX/FA and 2 (range: 1-6) with bolus Act-D - and the time to remission -median 9 weeks (range: 2-16) with MTX/FA and 10 weeks (range: 2-16) with bolus Act-D) - were not different between the groups. In both groups, first-line side effects frequency were high but intensity was low; stomatitis was higher with MTX/FA (p<0.01) and nausea and vomit with Act-D (p<0.01). Final single-agent ChT responses were high in both groups (94.8% with MTX/FA and 83.5% with bolus Act-D; p<0.01) and 13% higher in the group initially treated with MTX/FA. Rates of hysterectomy and of GTN recurrence were low and similar. No patient died due to GTN.
The two regimens had similar first-line ChT response. Final single-agent response rates were high and similar in both groups but the final single-agent remission rate was higher in the MTX/FA group.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2014;36(3):113-117
DOI 10.1590/S0100-72032014000300004
To investigate the prevalence of chromosomal abnormalities in couples with two or more recurrent first trimester miscarriages of unknown cause.
The study was conducted on 151 women and 94 partners who had an obstetrical history of two or more consecutive first trimester abortions (1-12 weeks of gestation). The controls were 100 healthy women without a history of pregnancy loss. Chromosomal analysis was performed on peripheral blood lymphocytes cultured for 72 hours, using Trypsin-Giemsa (GTG) banding. In all cases, at least 30 metaphases were analyzed and 2 karyotypes were prepared, using light microscopy. The statistical analysis was performed using the Student t-test for normally distributed data and the Mann-Whitney test for non-parametric data. The Kruskal-Wallis test or Analysis of Variance was used to compare the mean values between three or more groups. The software used was Statistical Package for the Social Sciences (SPSS), version 17.0.
The frequency of chromosomal abnormalities in women with recurrent miscarriages was 7.3%, including 4.7% with X-chromosome mosaicism, 2% with reciprocal translocations and 0.6% with Robertsonian translocations. A total of 2.1% of the partners of women with recurrent miscarriages had chromosomal abnormalities, including 1% with X-chromosome mosaicism and 1% with inversions. Among the controls, 1% had mosaicism.
An association between chromosomal abnormalities and recurrent miscarriage in the first trimester of pregnancy (OR=7.7; 95%CI 1.2--170.5) was observed in the present study. Etiologic identification of genetic factors represents important clinical information for genetic counseling and orientation of the couple about the risk for future pregnancies and decreases the number of investigations needed to elucidate the possible causes of miscarriages.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2014;36(2):72-78
DOI 10.1590/S0100-72032014000200005
To compare salivary and serum cortisol levels, salivary alpha-amylase (sAA), and unstimulated whole saliva (UWS) flow rate in pregnant and non-pregnant women.
A longitudinal study was conducted at a health promotion center of a university hospital. Nine pregnant and 12 non-pregnant women participated in the study. Serum and UWS were collected and analyzed every trimester and twice a month during the menstrual cycle. The salivary and serum cortisol levels were determined by chemiluminescence assay and the sAA was processed in an automated biochemistry analyzer.
Significant differences between the pregnant and non-pregnant groups were found in median [interquartile range] levels of serum cortisol (23.8 µL/dL [19.4-29.4] versus 12.3 [9.6-16.8], p<0.001) and sAA (56.7 U/L [30.9-82.2] versus 31.8 [18.1-53.2], p<0.001). Differences in salivary and serum cortisol (µL/dL) and sAA levels in the follicular versus luteal phase were observed (p<0.001). Median UWS flow rates were similar in pregnant (0.26 [0.15-0.30] mL/min) and non-pregnant subjects (0.23 [0.20-0.32] mL/min). Significant correlations were found between salivary and serum cortisol (p=0.02) and between salivary cortisol and sAA (p=0.01).
Serum cortisol and sAA levels are increased during pregnancy. During the luteal phase of the ovarian cycle, salivary cortisol levels increase, whereas serum cortisol and sAA levels decline.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2013;35(9):407-412
DOI 10.1590/S0100-72032013000900005
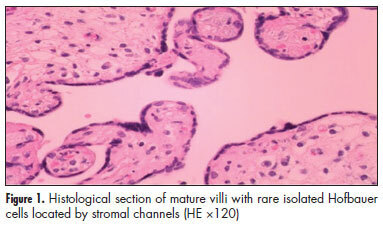
PURPOSE: In placentas from uncomplicated pregnancies, Hofbauer cells either disappear or become scanty after the fourth to fifth month of gestation. Immunohistochemistry though, reveals that a high percentage of stromal cells belong to Hofbauer cells. The aim of this study was to investigate the changes in morphology and density of Hofbauer cells in placentas from normal and pathological pregnancies. METHODS: Seventy placentas were examined: 16 specimens from normal term pregnancies, 10 from first trimester's miscarriages, 26 from cases diagnosed with chromosomal abnormality of the fetus, and placental tissue specimens complicated with intrauterine growth restriction (eight) or gestational diabetes mellitus (10). A histological study of hematoxylin-eosin (HE) sections was performed and immunohistochemical study was performed using the markers: CD 68, Lysozyme, A1 Antichymotrypsine, CK-7, vimentin, and Ki-67. RESULTS: In normal term pregnancies, HE study revealed Hofbauer cells in 37.5% of cases while immunohistochemistry revealed in 87.5% of cases. In first trimester's miscarriages and in cases with prenatal diagnosis of fetal chromosomal abnormalities, both basic and immunohistochemical study were positive for Hofbauer cells. In pregnancies complicated with intrauterine growth restriction or gestational diabetes mellitus, a positive immunoreaction was observed in 100 and 70% of cases, respectively. CONCLUSIONS: Hofbauer cells are present in placental villi during pregnancy, but with progressively reducing density. The most specific marker for their detection seems to be A1 Antichymotrypsine. It is remarkable that no mitotic activity of Hofbauer cells was noticed in our study, as the marker of cellular multiplication Ki-67 was negative in all examined specimens.