Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2021;43(8):588-594
In around 85% of vaginal births, the parturients undergo perineal lacerations and/or episiotomy. The present study aimed to determine the incidence of lacerations and episiotomies among parturients in 2018 in a habitual-risk public maternity hospital in southern Brazil, and to determine the risk and protective factors for such events.
A retrospective cross-sectional study. Data were obtained from medical records and analyzed using the Stata software. Univariate and multivariate logistic regressions were performed. Values of p<0.05 were considered significant.
In 2018, there were 525 vaginal births, 27.8% of which were attended by obstetricians, 70.7% by obstetric nurses, and 1.5% evolved without assistance. Overall, 55.2% of the parturients had some degree of laceration. The professional who attended the birth was a significant variable: a greater number of first- and second-degree lacerations, as well as more severe cases, occurred in births attended by nurses (odds ratio [OR]: 2,95; 95% confidence interval [95%CI]: 1,74 to 5,03). Positions at birth that did not enable perineal protection techniques (expulsive period with the “hands-off” method), when analyzed in isolation, determined the risk; however, in the final regression model, this relationship was not confirmed. Although reported in the literature, there were no associations between the occurrence of laceration and age, skin color, or birth weight. In 24% of the births, episiotomy was performed, and doctors performed 63.5% of them.
Births attended by nurses resulted in an increased risk of perineal lacerations, of varying degrees. In turn, those assisted by physicians had a higher occurrence of episiotomy.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2021;43(7):535-544
To investigate the feasibility of pelvic floor muscle training (PFMT) through gametherapy for relieving urinary symptoms of climacteric women with stress ormixed urinary incontinence (UI).
Randomized clinical trial, divided into two groups: Gametherapy (G_Game) and Control (G_Control). Both groups received recommendations about unsupervised PFMT, and G_Game also received supervised PFMT through gametherapy. After 5 consecutive weeks, the feasibility was investigated considering participant adherence, urinary symptoms (evaluated by the International Consultation on Incontinence Questionnaire-Urinary Incontinence Short Form [ICIQ-UI-SF] questionnaire), and pelvic floor function (PERFECT Scheme: power, endurance, repetition and fast). The Fisher exact, Kruskal-Wallis, Wilcoxon sign paired, and Mann-Whitney U tests were used by intention-to-treat analysis, using STATA 15.1 (StataCorp, College Station, TX, USA) software.
The present study included 20 women per group and observed a higher adherence in G_Game. In the intragroup analysis, a decrease in the ICIQ-UI-SF score was observed in both groups (14.0 to 10.0; 13.5 to 0), associated with increased endurance (2.5 to 3.5; 2.5 to 4.0) in G_Control and G_Game, respectively. Moreover, there was a concomitant increase in pelvic floor muscles (PFMs) power (2.0 to 3.0), repetition (3.0 to 5.0), and fast (10.0 to 10.0) in G_Game. In the intergroup analysis, a reduction of UI was observed (p<0.001; r=0.8), as well an increase in PFM power (p=0.027, r=0.2) and endurance (p=0.033; r=0.3) in G_Game.
The feasibility of supervised PFMT through gametherapy was identified by observing participant adherence, relief of urinary symptoms, and improvement in PFM function.

Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2021;43(7):530-534
To evaluate the accuracy of transvaginal ultrasound in the diagnosis of intrauterine lesions, using hysteroscopy as the gold standard.
This was a prospective observational study with 307 patients. All patients underwent hysteroscopy after a previous transvaginal ultrasound to compare the results. The hysteroscopy was performed by experienced examiners, and transvaginal ultrasounds were performed in various public and private services, which is reflective of routine healthcare practices in obstetrics and gynecology. The sensitivity, specificity, and accuracy of the transvaginal ultrasound were calculated using hysteroscopy as the gold standard. The level of agreement between the two exams was calculated using the Kappa test.
Themean age was 56.55±12.3 years. For endometrial polyps, we observed a sensitivity of 39.8%, specificity of 72.7%, accuracy of 52.8%, and Kappa index of 0.11 (p=0.025). For fibroids, the sensitivity was 46.7%, specificity was 95.0%, accuracy was 87.9%, and Kappa index was 0.46 (p<0.001). For endometrial thickening, the sensitivity was 68.7%, specificity was 41.7%, accuracy was 47.6%, and Kappa index was 0.06 (p=0.126). For endometrial atrophy, we found a sensitivity of 6.7%, specificity of 99.3%, accuracy of 90.2%, and Kappa index of 0.10 (p=0.006). For the other findings, the sensitivity was 15.6%, specificity was 99.6%, accuracy was 87.3%, and Kappa index was 0.23 (P<0.001).
Our study demonstrated a low level of accuracy of transvaginal ultrasound for the diagnosis of endometrial lesions, when performed by a non-experienced professional. Thus, it is important to consider the use of hysteroscopy to avoid unnecessary and inappropriate treatments.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2021;43(7):522-529
To assess the sexual function and associated factors in postmenopausal women.
This a descriptive, cross-sectional study with 380 women aged 40 to 65 years, users of public health services in 2019. Questionnaires were applied on demographic characteristics, on climacteric symptoms (menopause rating scale) and on sexual function (sexual quotient, female version). Bivariate andmultiple analyses by logistic regression were performed, with adjusted odds ratios (ORad) and 95% confidence intervals (95%CIs).
More than half (243/64%) of the participating women were at risk of sexual dysfunction, with lower scores in the domains of sexual desire and interest, comfort, orgasm, and satisfaction. Women with a partner (ORad 2.07; 95%CI 1.03-4.17) and those who reported sleep problems (ORad 2.72; 95%CI 1.77-4.19), depressed mood (ORad 2.03; 95%CI 1.32-3.10), sexual complaints (ORad 8.16; 95%CI 5.06-13.15), and vaginal dryness (ORad 3.44; 95%CI 2.22-5.32) showed greater chance of sexual dysfunction.
There was a high prevalence of sexual dysfunction, with the influence of conjugality and climacteric symptoms on sexual function.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2021;43(7):513-521
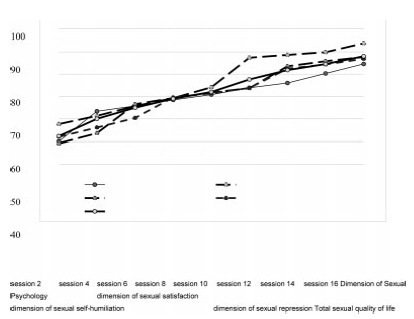
Early marriage has many deleterious effects on the health of girls, such as sexual dissatisfaction, an inevitable result of the lack of sufficient knowledge about sexual issues at the time of the marriage. The goal of the present study was to determine the effectiveness of counseling based on functional analytic psychotherapy with enhanced cognitive therapy (FECT) on the sexual quality of life of married adolescent women.
This clinical trial was conducted between July and October 2019 on 150 married adolescent women who met the inclusion criteria. In the intervention group, FECTwas conducted in sixteen 90-minute sessions twice a week. The Sexual Quality of Life-Female (SQOL-F) questionnaire was used. When the study ended, the control group was given the choice of receiving the same intervention as the intervention group.
The paired t-test showed a significant difference between the mean score of sexual quality of life before (52.33±23.09) and after (88.08±10.51) counseling in the intervention group (p<0.0001). According to the analysis of covariance, there was a significant difference between the score on sexual quality after counseling between the intervention (88.08±10.51) and control (60.32±23.73) groups (p<0.0001). There was also a significant difference between the mean score on the four dimensions of sexual quality of life in the intervention group (p<0.0001).
The results showed that counseling based on FECT improved the sexual quality of life in all dimensions in married adolescent women.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2021;43(7):507-512
To evaluate the factors associated with abortion complications following the implementation of the good-practice surveillance network Mujeres en Situación de Aborto (Women Undergoing Abortion, MUSA, in Spanish).
A cross-sectional study withwomen who underwent abortion due to any cause and in any age group at UNICAMP Women’s Hospital (part of MUSA network), Campinas, Brazil, between July 2017 and Agust 2019. The dependent variable was the presence of any abortion-related complications during hospitalization. The independent variables were clinical and sociodemographic data. The Chi-square test, the Mann-Whitney test, and multiple logistic regression were used for the statistical analysis.
Overall, 305 women were enrolled (mean±standard deviation [SD] for age: 29.79±7.54 years). The mean gestational age was 11.17 (±3.63) weeks. Accidental pregnancy occurred in 196 (64.5%) cases, 91 (29.8%) due to contraception failure. At least 1 complication was observed in 23 (7.54%) women, and 8 (34.8%) of them had more than 1. The most frequent complications were excessive bleeding and infection. The factors independently associated with a higher prevalence of complications were higher gestational ages (odds ratio [OR]: 1.22; 95% confidence interval [95%CI]: 1.09 to 1.37) and contraceptive failure (OR: 3.4; 95%CI: 1.32 to 8.71).
Higher gestational age and contraceptive failure were associated with a higher prevalence of complications. This information obtained through the surveillance network can be used to improve care, particularly in women more susceptible to unfavorable outcomes.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2021;43(8):608-615
To establish a relationship between serum progesterone values on the day of frozen blastocyst transfer in hormone-replaced cycles with the probability of pregnancy, miscarriage or delivery.
This was an ambispective observational study including all frozen-thawed embryo transfer cycles performed at our department following in vitro fecundation from May 2018 to June 2019. The outcomes evaluated were β human chorionic gonadotropin (β-hCG)-positive pregnancy and delivery. Groups were compared according to the level of serum progesterone on the day of embryo transfer: the 1st quartile of progesterone was compared against the other quartiles and then the 2nd and 3rd quartiles against the 4th quartile.
A total of 140 transfers were included in the analysis: 87 with β-HCG>10 IU/L (62%), of which 50 (36%) delivered and 37 had a miscarriage (42%).Women with lower progesterone levels (< 10.7ng/mL) had a trend toward higher β-HCG-positive (72 versus 59%; p>0.05), lower delivery (26 versus 39%; p>0.05) and higher miscarriage rates (64 versus 33%; p<0.01). Comparing the middle quartiles (P25-50) with those above percentiles 75, the rate of pregnancy was similar (60 versus 57%; p>0.05), although there was a trend toward a higher number of deliveries (43 versus 31%; p>0.05) and a lower number of miscarriages (28 versus 45%; p>0.05). These differences were not statistically significant.
There were no differences in pregnancy and delivery rates related with the progesterone level when measured in the transfer day. The miscarriage rate was higher in the 1st quartile group.