Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2024;46:e-rbgo84
Included evaluation of the possibility of using the systemic inflammatory indices for preoperative screening for the presence and severity of endometriosis (EM) in comparison to the findings of the exploratory laparoscopy
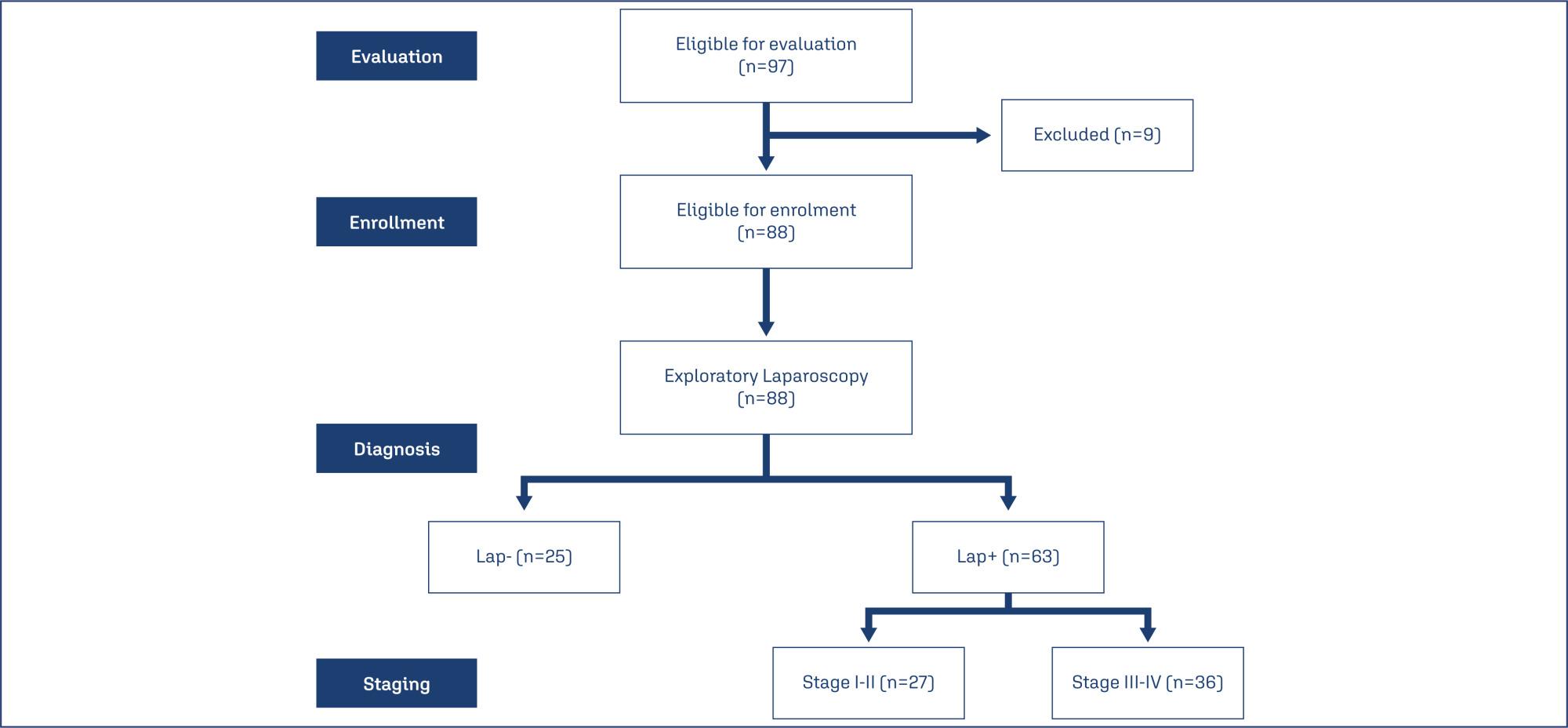
88 women with clinical manifestations suggestive of EM were evaluated clinically and by US and gave blood samples for estimation of serum cancer antigen-125 (CA125), platelet and total and differential leucocytic counts for calculation of inflammatory indices; the Systemic Immune-Inflammation index, the Systemic Inflammation Response Index (SIRI), the Neutrophil-Lymphocyte ratio (NLR), the Neutrophil-Monocyte ratio, the Neutrophil-Platelet ratio and the Platelet-Lymphocyte ratio. Then, patients were prepared to undergo laparoscopy for diagnosis and staging.
Laparoscopy detected EM lesions in 63 patients; 27 of stage I-II and 36 of stage III-IV. Positive laparoscopy showed significant relation with US grading, high serum CA125 levels, platelet and inflammatory cell counts and indices. Statistical analyses defined high SIRI and NLR as the significant predictors for positive laparoscopy and high serum CA125 and NLR as the most significant predictors for severe EM (stage III-IV) on laparoscopy
The intimate relation between EM and inflammation was reflected systematically as high levels of blood cellular components, but indices related to neutrophil especially NLR and SIRI showed highly significant relation to the presence and severity of EM and might be used as routine, cheap and non-invasive screening test before exploratory laparoscopy to guide the decision-making.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2024;46:e-rbgo86
HPV infection is considered the most common sexually transmitted virus today. The persistence of HPV is the main cause for the development of precursor lesions and cervical cancer. There are environmental and non-environmental factors that contribute to the persistence of the virus. Studies indicate a possible relationship between the vaginal microbiota (environmental factor) and the risk of high-grade cervical squamous intraepithelial lesions and cervical cancer. This study evaluates the association between the type of vaginal microbiota and the occurrence of high-grade squamous intraepithelial lesions of the cervix.
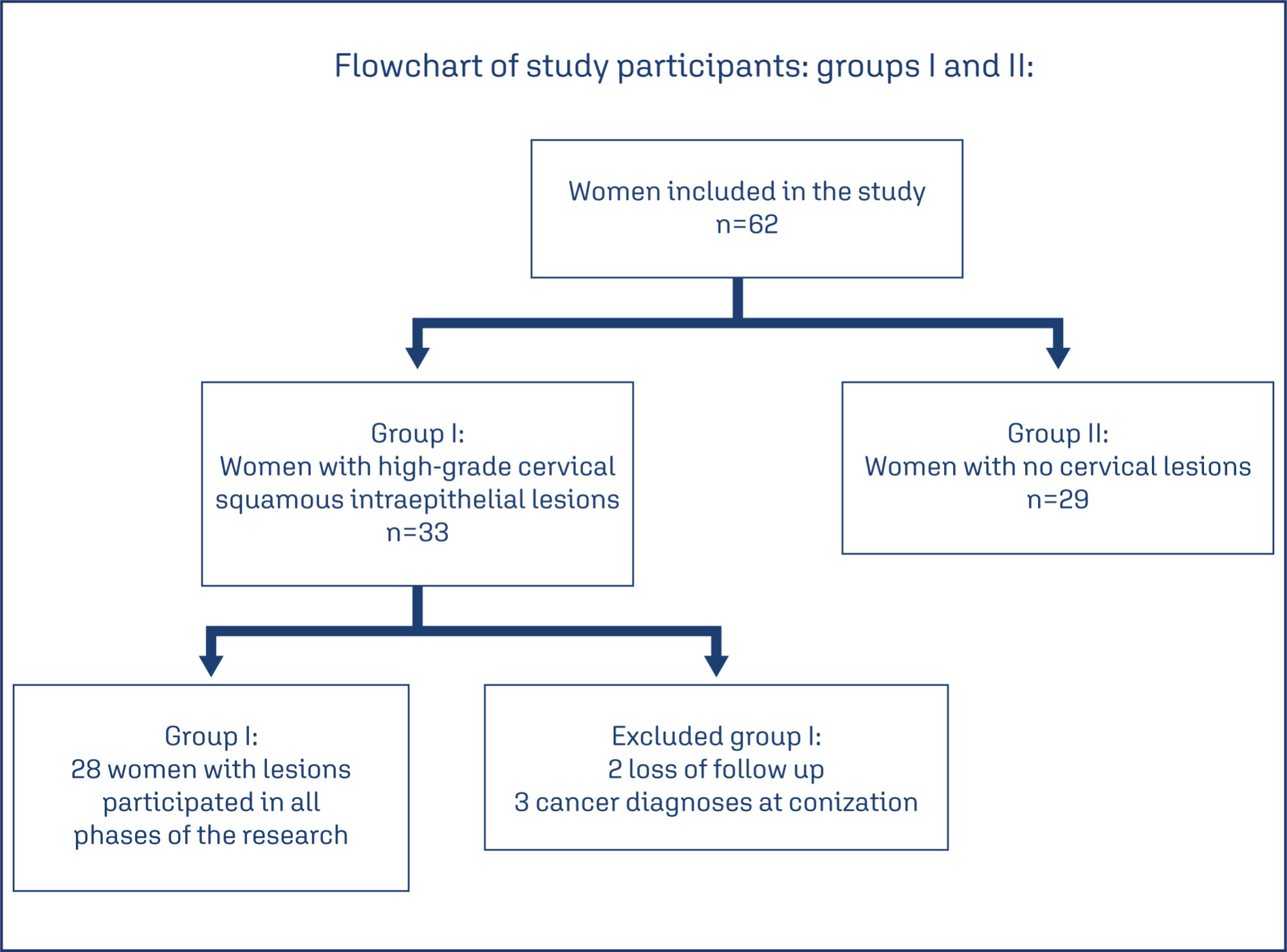
Observational, longitudinal, prospective, and analytical studies carried out between 2019 and 2021, which evaluated the vaginal microbiota of patients diagnosed with high-grade cervical squamous intraepithelial lesion before and after treatment in two collections with an interval of 6 months, using scrapings and vaginal swabs.
In Group I (with lesions) 28 women participated and 29 in Group II (without lesions). According to Nugent, in the initial collection of Group I, 16 women (57%) had lactobacillary microbiota, eight (28%) intermediate, and four (14%) coccus. In Group II, twenty-one (75%) were lactobacillary, one (3%) was intermediate, and seven (24%) werecoccus. With p=0.03.
According to Nugent's criteria, there was an association between the type of vaginal microbiota and the occurrence of high-grade cervical squamous intraepithelial lesions of the cervix. The same was not observed in the Donders classification. Studies with a larger sample are needed to confirm our results.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2024;46:e-rbgo91
The average age of patients with vulvar squamous cell carcinoma (SCC) has been reported to have declined. Human papilloma virus (HPV)-related lesions have been shown to be associated with the expression of the immunohistochemical (IHC) marker p16. Non-HPV-related tumors have been characterized by p53 abnormal expression and PDL1 expression. We aimed to evaluate the correlation between these markers and vulvar SCC and to relate it to the clinical and pathological characteristics.
Histopathologic assessments and IHC analyses of p16, p53, and PDL1 were performed in 41 samples of vulvar SCC collected between 2016 and 2021. The data were correlated with clinical and pathological characteristics of the patients.
The mean age of the patients was 72.1 years. Positive p16 and PDL1 staining was detected in 24.4% and 17.1% of the samples, respectively. p53 expression was negative in 19.5% of the samples, whereas it was overexpressed in 24.4%. p16-positive tumors showed a smaller depth of invasion (DOI) (p = 0.014), while tumors with p53 abnormal expression showed greater DOI (p = 0.041). PDL1 expression was correlated with increased number of inflammatory cells (p = 0.055). In addition, lesions with lymphovascular space invasion were p16-negative.
In our sample, regarding to the SCC incidence the patients’ mean age did not change. The expression of p16 was inversely correlated with p53 results. Tumors with p53 abnormal expression and absence of p16 showed a greater DOI. Our data suggest an association between PDL1 expression and increased inflammatory infiltrates in vulvar SCC.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2024;46:e-rbgo93
To analyze the prognosis of patients with breast cancer who developed trastuzumab-induced cardiotoxicity and to analyze factors associated with and resulting from cardiotoxicity.
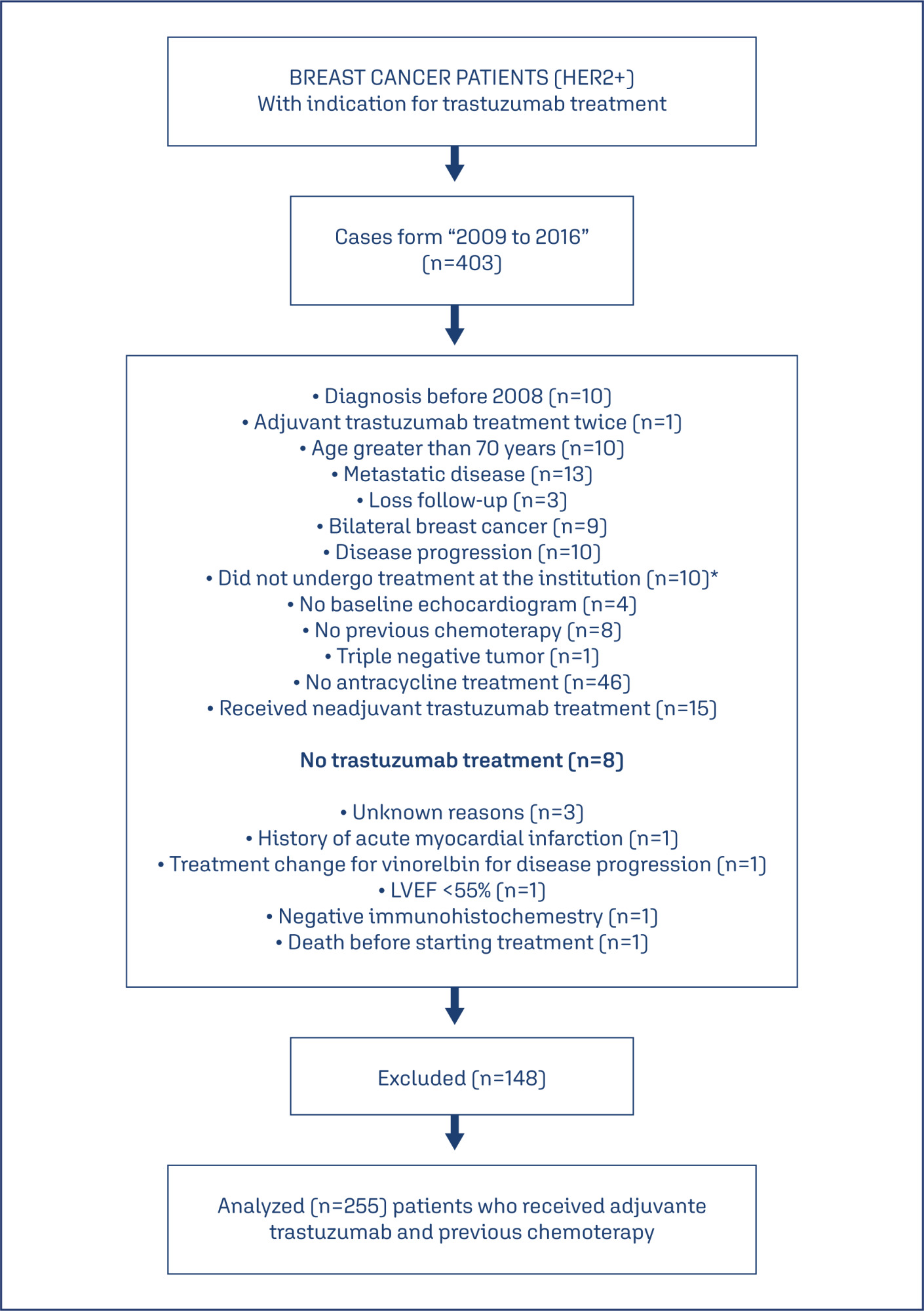
This was a retrospective cohort study that included 255 HER2-positive breast cancer patients who received adjuvant trastuzumab therapy. The inclusion criteria were a diagnosis of HER2-positive breast cancer and adjuvant trastuzumab therapy; disease stage I-III; <70 years; and a baseline echocardiogram showing a left ventricular ejection fraction (LVEF) ≥ 55%. The Kaplan-Meier method, the log-rank test, and the Cox proportional hazards model were used.
In all, 15.3% (39/255) of patients presented with cardiotoxicity. Treatment was suspended in 92.3% (36/39) of patients who presented with cardiotoxicity during trastuzumab treatment. The treatment was suspended in 46 of 255 patients and it was permanently interrupted in 84.8% (33/46) of these patients, with 84.8% (28/33) due to cardiotoxicity. Cardiotoxicity was not associated with disease-free survival (DFS) (hazard ratio (HR) = 1.48; 95% confidence interval (CI = 0.79-2.78) or overall survival (OS) (HR = 1.68; 95%CI= 0.83-3.41). Patients with clinical stage III and whom trastuzumab therapy was suspended (all causes) had worse DFS; (HR = 3.19; 95% CI=1.77-5.74) and (HR = 1.83; 95% CI=1.01-3.32) respectively. Those with clinical stage III and whom trastuzumab therapy was permanently interrupted had worse OS; (HR = 3.80; 95% CI =1.82-7.94), and (HR = 2,26; 95% CI =1.09-4.68 respectively.
Cardiotoxicity was not associated with DFS or OS. Clinical stage III, Suspension and permanent interruption of treatment regardless of the cause were associated with worse DFS and OS in breast cancer patients.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2024;46:e-rbgo78
To traslate and validate of the Brazilian version of the SDI-2.
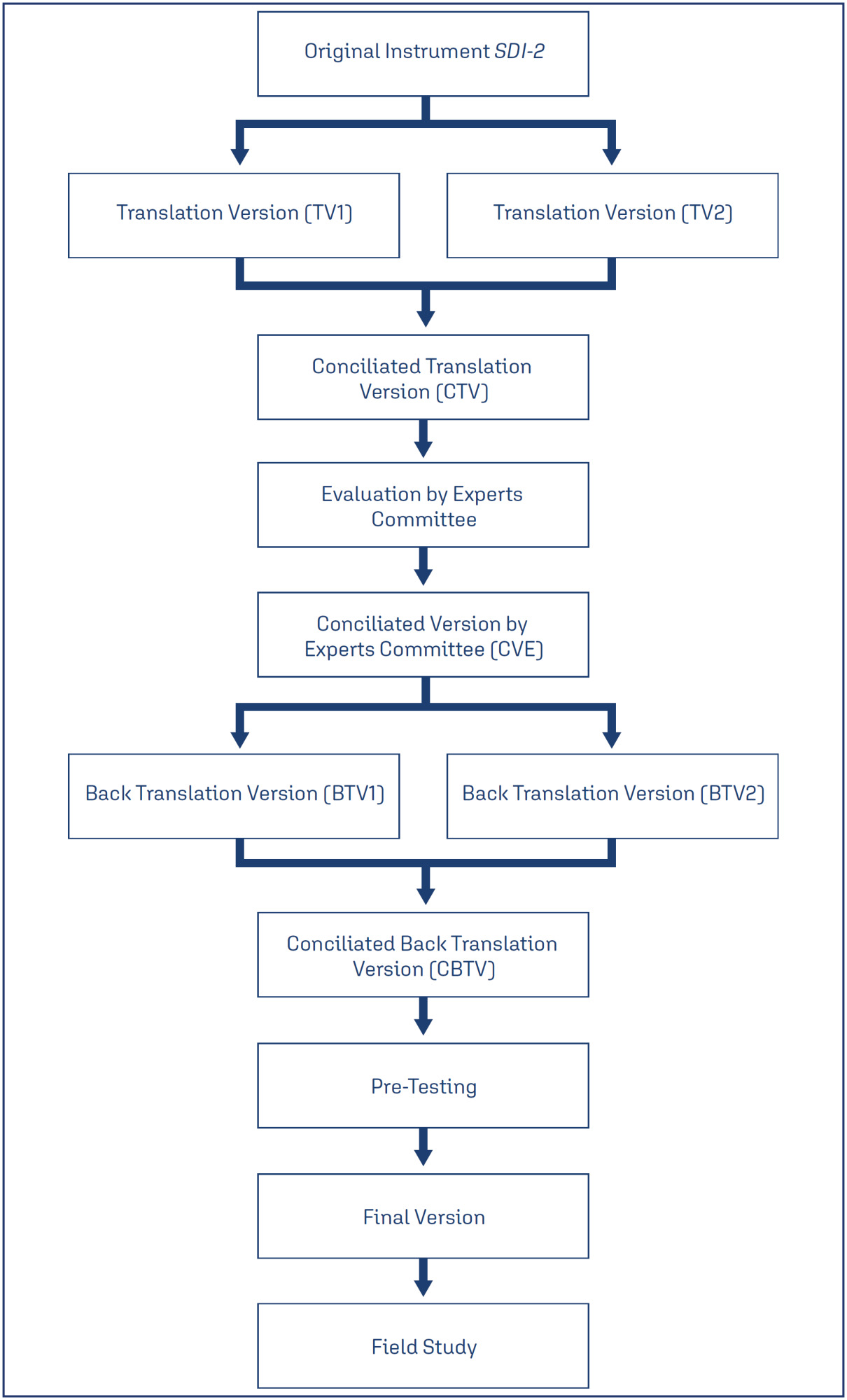
This was a cross-sectional study. The cultural adaptation considered the stages of initial translation, synthesis of translations, evaluation by a committee of experts from different regions of Brazil, back-translation, and pre-test. The content validity and psychometric proprieties was assessed.
Ten specialists participated in the cultural adaptation of the SDI-2. The content validity showed a Content Validity Ratio (CVR) ≥ 0.75 (p = 0.05). A total of 674 subjects participated in the field study. The Exploratory Factorial Analysis (EFA) presented factor loads ≥ 0.445, and commonalities ≥ 0.40; and two dimensions represented 77% of the total variance explained. The Confirmatory Factorial Analysis CFA presented X2/df = 4.265; the Root Mean Square Error of Approximation RMSEA = 0.110; the Non-Normed Fit Index NNFI = 0.946; the Comparative Fit Index (CFI) = 0.963; the Goodness of Fit Index GFI = 0.986; and the Adjusted Goodness of Fit Index AGFI = 0.979 for a two-factor model. The coefficient values for the total SDI-2 score were 0.91 for Cronbach's alpha, 0.91 for McDonald's Omega, and 0.97 for the Greatest Lower Bound GLB coefficients. The invariance between sexes was 0.01 for the ΔCFI and ΔRMSEA, showing model stability for these two populations.
The Brazilian version of the SDI-2 is self-report, valid, reliable and invariant across sex.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2024;46:e-rbgo83
Evaluate the risk factors for the development of post-molar gestational trophoblastic neoplasia.
Retrospective cohort study with 320 women with gestational trophoblastic disease (GTD) followed in a tertiary hospital from January 2005 to January 2020. Data referring to the women's sociodemographic profile, clinical, laboratory and treatment aspects and types of GTD were analyzed.
The mean age of women with the benign form was 26.4±8.6 years and with the malignant forms 26.9±8.5 years (p=0.536). Most women with malignant forms came from regions further away from reference center (p=0.012), had vesicle elimination at the time of diagnosis (p=0.028) and needed more than one uterine evacuation (p<0.001) when compared to the benign forms. There was no difference between laboratory tests in both forms. Being between 30 and 39 years old increased the chance of developing invasive mole by 2.5 (p=0.004; 95%CI:1.3–4.9) and coming from regions far from reference center by 4.01 (p=0.020; CI95%: 1.2-12.9). The women with the highest risk of malignant forms were those with the longest time of become normal on human gonadotrophic hormone (hCG) testing (each week the risk increases 1.3 times; p<0.001, 95%CI: 1.2-1.3).
The prolonged hCG fall curve is the main indicator of an increased chance of GTN. Women from regions further away from reference center have a greater chance of developing malignant forms, probably due to the difficulty in accessing the reference center and, therefore, adequate follow-up that would allow early identification of more serious cases.

Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2024;46:e-rbgo87
To compare access and suitability of antenatal care between years 2020 and 2022 among postpartum individuals at a Hospital in Florianopolis, and evaluate factors associated with antenatal suitability.
Observational, cross-sectional, and quantitative study carried out in 2022. Collected data were compared with the database of a previous similar study carried out in the same setting in 2020. Data were extracted from medical records and prenatal booklets, in addition to a face-to-face questionnaire. Adequacy was measured using the Carvalho and Novaes index and health access was qualitatively evaluated. Socio-demographic and antenatal variables were analyzed. A statistical significance level of 0.05 was considered. Open-ended questions were categorized for analysis.
395 postpartum individuals were included. Antenatal care was adequate for 48.6% in 2020 and 69.1% in 2022. Among the barriers to access, 56% reported difficulty in scheduling appointments and/or exams and 23% complained of reduced healthcare staff due to strikes, COVID-19, among others. Adequate antenatal care was associated with being pregnant in 2022, being referred to high-risk units (PNAR), and not reporting difficulties in access. Also, it was associated with twice the chance of investigation for gestational diabetes (GDM) and syphilis.
The 2022 post-vaccination period showed higher antenatal adequacy. The main difficulty for postpartum individuals was scheduling appointments and/or exams. Having antenatal care in 2022, no reports of difficulty in access, and follow-up at a high-risk unit were associated with antenatal adequacy.