Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2016;38(9):450-455
To demonstrate the initial experience of robotic hysterectomy to treat benign uterine disease at a university hospital in Brazil.
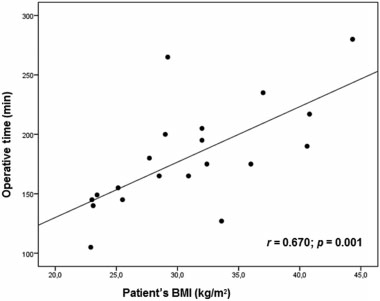
A cross-sectional study was conducted to review data from the first twenty patients undergoing robotic hysterectomy at our hospital. The surgeries were performed from November 2013 to August 2014, all of them by the same surgeon. The patients were reviewed for preoperative characteristics, including age, body mass index (BMI), indications for the hysterectomy and previous surgeries. Data of operative times, complications, postoperative pain and length of hospital stay were also collected.
The total operating room time was 252.9 minutes, while the operative time was 180.7 minutes and the console time was 136.6 minutes. Docking time was 4.2 minutes, and the average undocking time was 1.9 minutes. There was a strong correlation between the operative time and the patient's BMI (r = 0.670 ; p = 0.001). The console time had significant correlation with the uterine weight and the patient's BMI (r = 0.468; p = 0.037). A learning curve was observed during docking and undocking times.
Despite its high cost, the robotic surgery is gaining more space in gynecological surgery. By the results obtained in our hospital, this surgical proposal proved to be feasible and safe. Our initial experience demonstrated a learning curve in some ways.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2016;38(9):443-449
to translate and adapt the Patient Satisfaction Questionnaire (PSQ) to Portuguese and to assess its psychometric properties based on internal consistency, test-retest, factor analysis and divergent and convergent construct validities.
The study involved 218 participants and was approved by the local Research Ethics Committee. All participants gave written informed consent and their anonymity was ensured. The instrument was translated and culturally adapted for use in the Portuguese language. The internal consistency and factorial analysis were assessed by patients and physicians. Convergent and divergent validities were also assessed specifically for the patient group, as well as test-retest reliability. The Portuguese versions of the Patient Health Questionnaire (PHQ-9) and State-Trait Anxiety Inventory (STAI) were used for the analysis of the convergent validity. In addition, we applied a questionnaire of clinical and demographic data for the analysis of the divergent validity.
The adapted version of the PSQ showed good Cronbach’s α and test-retest values, and the results of the convergent construct validity between the PSQ and the PHQ-9 (r = 0.34; p = 0.02) and the STAI (r = 0.47; p = 0.001) were negative, significant and moderate correlations. Divergent validity showed significant correlations only with race and education. The Brazilian Portuguese versionof the PSQ proved to be a valid and reliable instrument, with psychometric properties suitable for the assessment of satisfaction among patients with chronic pelvic pain and their physicians in Brazil. The questionnairemay allow the homogenization of reports on this topic in the international literature.

Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2016;38(9):436-442
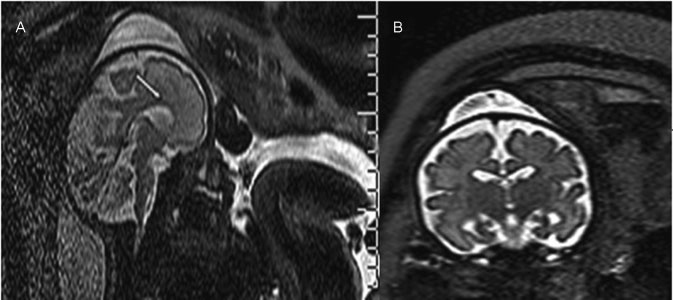
Ventriculomegaly (VM) is one the most frequent anomalies detected on prenatal ultrasound. Magnetic resonance imaging (MRI) may enhance diagnostic accuracy and prediction of developmental outcome in newborns.
The aim of this study was to assess the correlation between ultrasound and MRI in fetuses with isolated mild and moderate VM. The secondary aim was to report the neurodevelopmental outcome at 4 years of age.
Fetuses with a prenatal ultrasound (brain scan) diagnosis of VM were identified over a 4-year period. Ventriculomegaly was defined as an atrial width of 10- 15 mm that was further divided as mild (10.1-12.0 mm) and moderate (12.1-15.0 mm). Fetuses with VM underwent antenatal as well as postnatal follow-ups by brain scan and MRI. Neurodevelopmental outcome was performed using the Griffiths Mental Development Scales and conducted, where indicated, until 4 years into the postnatal period.
Sixty-two fetuses were identified. Ventriculomegaly was bilateral in 58% of cases. A stable dilatation was seen in 45% of cases, progression was seen in 13%, and regression of VM was seen in 4.5% respectively. Fetal MRI was performed in 54 fetuses and was concordant with brain scan findings in 85% of cases. Abnormal neurodevelopmental outcomes were seen in 9.6% of cases.
Fetuses in whom a progression of VM is seen are at a higher risk of developing an abnormal neurodevelopmental outcome. Although brain scan and MRI are substantially in agreement in defining the grade of ventricular dilatation, a low correlation was seen in the evaluation of VM associated with central nervous system (CNS) or non-CNS abnormalities.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2016;38(9):428-435
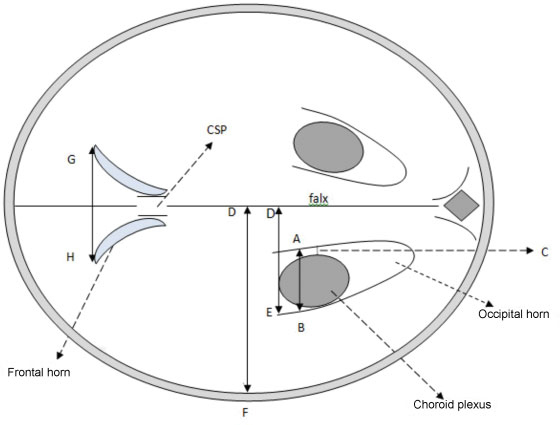
This study was done to evaluate the normal fetal cerebral lateral ventricle dimensions with transabdominal ultrasonography. The atrial width (AW), ventricle-tochoroid measurement (V-C), ventricle-to-hemisphere ratio (VHR), and combined anterior horn measurement (CAHM) were taken.
This was a cross-sectional study involving 400 normal singleton pregnant subjects whose gestational ages were between 14 and 40 weeks. Transabdominal sonography was performed to obtain the values of the fetal cerebral lateral ventricle (FCLV) parameters. Data were reported as mean standard deviation (SD) for continuous variables. The degrees of correlation between FCLV parameters and the estimated gestational age (EGA) were obtained using Pearson's correlation. Regression equations were used to generate the reference limits for the FCLV measurements.
The values of AW, V-C measurements and CAHM increased with advancing gestation. The mean values of the AW, V-C and CAHM from 14 to 40 weeks increased from 6.60 0.94 mm to 9.75 0.07 mm (R2 = 0.114), 0.80 0.00 mm to 1.90 0.14 mm (R2= 0.266), and 6.95 0.06 mm to 23.07 4.02 mm (R2= 0.692) respectively, while the mean VHR decreased from 61.20 1.60% to 42.84 2.91% (R2 = 0.706) over the same period.
The AW, V-C, and CAHM increase, while VHR decreases with advancing gestation.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2016;38(7):348-355
To identify the epidemiological risk factors for congenital anomalies (CAs) and the impact of these fetal malformations on the perinatal outcomes.
This prospective cohort study comprised 275 women whose fetuses had CAs. Maternal variables to establish potential risk factors for each group of CA and perinatal outcomes were evaluated. The primary outcome was CA. Secondary outcomes included: fetal growth restriction (FGR); fetal distress (FD); premature rupture of membranes (PROM); oligohydramnios or polyhydramnios; preterm delivery (PTD); stillbirth; cesarean section; low birth weight; Apgar score < 7 at the 1st and 5th minutes; need for assisted ventilation at birth; neonatal infection; need for surgical treatment; early neonatal death; and hospitalization time. Chi-square (x2) test and multilevel regression analysis were applied to compare the groups and determine the effects of maternal characteristics on the incidence of CAs.
The general prevalence of CAs was of 2.4%. Several maternal characteristics were associated to CAs, such as: age; skin color; level of education; parity; folic acid supplementation; tobacco use; and history of previous miscarriage. There were no significant differences among the CA groups in relation to FGR, FD, PROM, 1-minute Apgar score > 7, and need for assisted ventilation at birth. On the other hand, the prevalence of the other considered outcomes varied significantly among groups. Preterm delivery was significantly more frequent in gastrointestinal tract/abdominal wall defects. The stillbirth rate was increased in all CAs, mainly in isolated fetal hydrops (odds ratio [OR]: 27.13; 95% confidence interval [95%CI]: 2.90-253.47). Hospitalization time was higher for the urinary tract and congenital heart disease groups (p < 0.01). Neonatal death was significantly less frequent in the central nervous system anomalies group.
It was possible to identify several risk factors for CAs. Adverse perinatal outcomes were presented in all CA groups, and may differ according to the type of CA considered.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2016;38(7):340-347
Aerobic exercises may improve quality of life (QoL) in women with polycystic ovary syndrome (PCOS). However, there is no data on the effect of resistance exercise training (RET) programs on the QoL of women with PCOS. Thus, this study aimed to assess the effect of a 16-week RET program on QoL in PCOS women.
This 16-week case-control study enrolled 43 women with PCOS (PCOS group, PCOSG) and 51 healthy pre-menopausal controls aged 18 to 37 years (control group, CG). All women underwent a supervised RET program for 16 weeks, and were evaluated in two different occasions: week-0 (baseline), and week-16 (after RET). Quality of life was assessed using the 36-Item Short Form Health Survey (SF-36).
Testosterone reduced significantly in both groups after RET (p < 0.01). The PCOSG had improvements in functional capacity at week-16 relative to week-0 (p = 0.02). The CG had significant improvements in vitality, social aspects, and mental health at week-16 relative to week-0 (p ≤ 0.01). There was a weak correlation between social aspects of the SF-36 domain and testosterone levels in PCOS women.
A 16-week RET program modestly improved QoL in women with PCOS.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2016;38(7):333-339
To assess the viability of bovine ovarian tissue after cryopreservation through either slow freezing or vitrification, and to compare it to that of control tissue by performing morphological analyses.
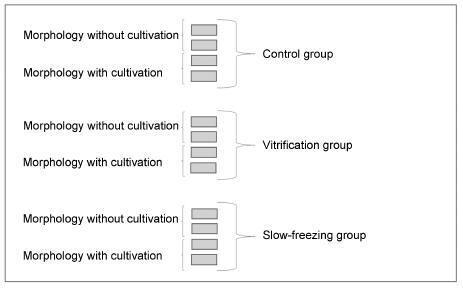
The study included 20 bovine ovarian cortex fragments that were divided into control, vitrification, and slow freezing groups. Each group consisted of four fragments of the same ovary, two fixed without cultivation, and two fixed with cultivation. Tissues were evaluated based on follicular morphology immediately after heating and after 7 days of culture, and compared with the control group.
A total of 240 fragments were analyzed, generating a sample of 1,344 follicles without cultivation and 552 with cultivation. When the non-cultivated samples were classified as non-atretic follicles, 572 were found in the control group, 289 in the vitrification group, and 373 in the slow freezing group, showing no significant differences. When classified as atretic, 46 follicles were found in the control group, 23 in the vitrification group, and 41 in the slow freezing group, also showing no statistical difference. In the post-culture sample, an evolution of the follicular stages could be observed. This finding was important to support that the follicles considered non-atretic in the non-cultivated group were actually viable in the morphological evaluation.
With no differences between the protocols, vitrification was shown to be an advanced and alternative method for patients who will undergo treatments that
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2016;38(7):325-332
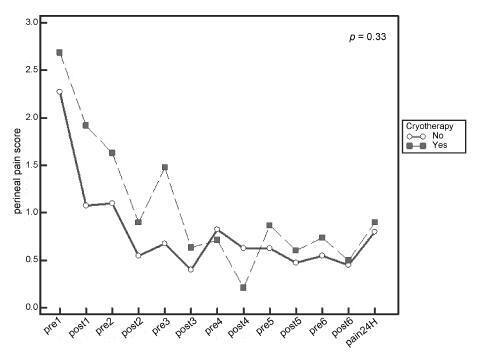
Systematic reviews that evaluate the perineal cryotherapy to reduce pain in the vaginal postpartum are inconclusive.
To evaluate clinical effectiveness of cryotherapy in the management of humanized postpartum perineal pain and vaginal edema.
A double-bind randomized controlled clinical trial (UTN number: U1111- 1131-8433) was conducted in a hospital in Northeastern, Brazil.Women were included following humanized childbirth. All had vaginal deliveries of a single, full-term pregnancy with cephalic presentation. Exclusion criteria included previous perineal lesion, episiotomy during the current delivery, instrumental delivery, uterine curettage and postpartum hemorrhage. In the experimental group, an ice pack was applied six times on the perineum for 20 minutes, reducing the temperature between 10 and 15° C, then 60 minutes without exposure to cold. In the non-cryotherapy, a water bag unable to reduce the temperature to this extent was used, compliance with the same application protocol of the first group. Perineal temperature wasmonitored at zero, 10 and 20 minutes for application in both groups. Evaluations were made immediately before and after the applications and 24 hours after delivery spontaneous, to determine the association between variables.
A total of 80 women were included in the study, 40 in each group. There was no significant difference in scores of perineal pain and edema between the groups with or without cryotherapy until 24 hours after childbirth. There was no difference between groups when accomplished repeated measures analysis over the 24 hours after delivery, considering the median perineal pain (p = 0.3) and edema (p = 0.9). Perineal cryotherapy did not influence the amount of analgesics used (p = 0.07) and no adverse effect was registered.
The use of cryotherapy following normal vaginal delivery within the concept of humanized minimally interventionist childbirth had no effect on perineal pain and edema, since it was already substantially lower, nor the need for pain medicaments.