Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2021;43(9):669-675
Preeclampsia (PE) is a pregnancy-specific syndrome characterized by abnormal levels of cytokines and angiogenic factors, playing a role in the disease development. The present study evaluated whether immunological markers are associated with the gestational age and with the disease severity in preeclamptic women.
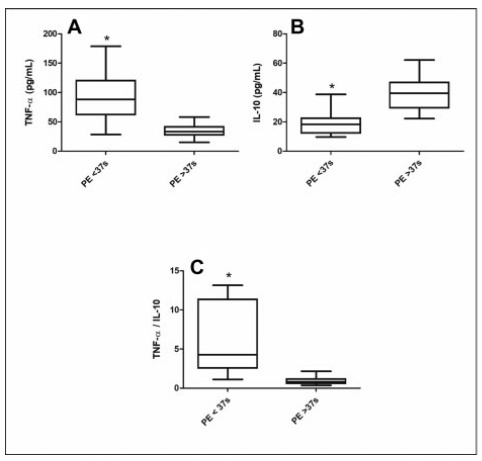
Ninety-five women who developed PE were stratified for gestational age as preterm PE (< 37 weeks) and term PE (≥ 37 weeks of gestation) and compared for disease severity as well as plasma concentration of angiogenic factors and cytokines. The concentrations of placental growth factor (PlGF), vascular endothelial growth factor (VEGF), Fms-like soluble tyrosine kinase (sFlt-1) and soluble endoglin (sEng), as well as the cytokines, tumor necrosis factor-α (TNF-α) and interleukin 10 (IL-10), were determined by enzyme-linked immunosorbent assay (ELISA).
The comparison between preeclamptic groups showed a higher percentage of severe cases in preterm PE (82.1%) than in term PE (35.9%). Similarly, the concentrations of TNF-α, sFlt-1, and sEng, as well as TNF-α/IL-10 and sFlt-1/PlGF ratios were significantly higher in the preterm PE group. In contrast, concentrations of PlGF, VEGF, and IL-10 were significantly lower in women with preterm PE. Negative correlations between TNF-α and IL-10 (r = 0.5232) and between PlGF and sFlt1 (r = 0.4158) were detected in the preterm PE.
In pregnant women with preterm PE, there is an imbalance between immunological markers, with the predominance of anti-angiogenic factors and TNF-α, associated with adverse maternal clinical outcomes.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2021;43(9):648-654
To identify how health providers recognize postpartum hemorrhage early and the difficulties involved in it.
An exploratory, descriptive study using a qualitative approach through a semi-structured interview technique. In total, 27 health professionals (nursing tech nicians, nurses, medical residents in Gynecology and Obstetrics, hired medical doctors, and medicine professors) working in a tertiary-level hospital of reference in women’s health care in the State of São Paulo, Brazil, participated in the study through an invitation. After they accepted the invitation, they signed the free and informed consent form. All interviews were recorded and transcribed, and a thematic analysis was conducted. We found three analysis categories: a) perception of the severity: “there is something wrong with the women”; b) difficulties in the early diagnosis of postpartum hemorrhage; and c) the process to improve obstetrical care.
Caregivers believe teamwork and communication should be improved. Besides the visual estimation of blood loss, the nursing team is attentive to behavioral symptoms like irritability, while the medical staff follow protocols and look for objective signs, such as altered vital signs.
Besides the objective evaluations, the subjective perceptions of the providers are involved in the clinical judgement regarding the diagnosis of postpartum hemorrhage, and this should be included in a broader diagnosis strategy.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2021;43(9):655-661
To describe the clinical experience with the B-Lynch technique in the management of postpartum hemorrhage as well as the factors related to the indication of the technique and to present the success rates of the application of the B-Lynch technique.
Observational, retrospective, cross-sectional, and analytical study. Patient data was obtained through the study of medical records. The study population comprised of patients who underwent hemostatic suture using the B-Lynch technique, including 104 patients within the period from January 1, 2005, to December 31, 2019.
Of the total of 104 patients, 82.7% did not present any complications. Blood transfusion and intensive care unit admission were the most prevalent complications, with 13.5% and 15.4%, respectively. Only 1% of the patients had puerperal and surgical site infections. The factors most related to the application of the technique were the presence of previous cesarean section (30.8%), use of oxytocin (16.3%), and pre-eclampsia (11.6%). Puerperal hysterectomy was performed in 4.8% of the patients due to failure of the method.
The clinical experience with the B-Lynch technique was satisfactory since it presented few complications, with excellent results in hemorrhagic control. Previous cesarean section, the use of oxytocin, and preeclampsia stood out as factors related to the indication of the application of the technique, and the success rate in controlling postpartum hemorrhage was 95.2%.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2021;43(8):622-626
To analyze the effect of the One-minute Preceptor model for preceptors who work at the emergency department of a maternity teaching hospital.
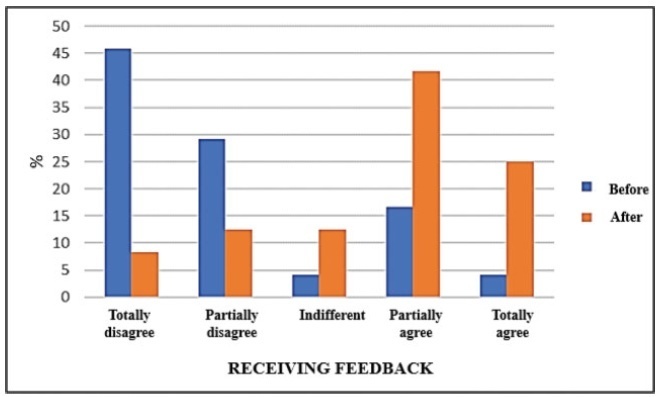
A quantitative intervention study conducted with Obstetrics and Gynecology residency preceptors at amaternity teaching hospital in northeastern Brazil. Three stages were performed: 1) a preintervention survey with the residents; 2) planning and execution of a pedagogical training course for the preceptors, which involved a lecture and a dramatization about the One-Minute Preceptor model; and 3) thirty days after the intervention, the residents answered another survey about the model and its repercussions and advantages.
The preintervention assessment with the residents showed that 91.7% agreed that there were discrepancies regarding the teaching model among the preceptors. After the training, all preceptors agreed that the model engages the student in the decision-making process, and that they would apply it to their routine. The postintervention results showed that 95.8% agreed that themodel ismore inviting than traditional teaching approaches. There was a perception of improvement in learning among 70.9% of the residents. In addition, the present study found a significant change in feedback before and after implementing the model, from 20.8% to 66.7%.
The training course of preceptors in the One-Minute Preceptor model proved to be efficient in providing formative feedback to residents in the emergency department of a maternity school. Further studies are needed to assess the consolidation of the methodology in the long term.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2021;43(8):616-621
This study evaluated the risk of the hereditary breast and ovarian cancer (HBOC) syndrome in patients with breast cancer by using the Family History Screening 7 (FHS-7) tool, a validated low-cost questionnaire with high sensitivity able to screen the HBOC risk in the population.
Women diagnosed with breast cancer (n=101) assisted by the Unified Health System at the 8th Regional Health Municipal Office of the state of Paraná answered the FHS-7, and the results were analyzed using IBM SPSS Statistics for Windows, Version 25.0. software (IBM Corp., Armonk, NY, USA).
The risk of HBOC was 19.80% (n=20). Patients at risk exhibited aggressive tumor characteristics, such as high-grade tumors (30%), presence of angiolymphatic emboli (35%), and premenopausal at diagnosis (50%). Significant associations between the prevalence of high-grade tumors were observed inwomen younger than 50 years at diagnosis with HBOC (p=0.003).
Our findings suggest a possible family inheritance associated with worse clinical features in women with breast cancer in this population, indicating that HBOC investigation can be initially performed with low-cost instruments such as FHS-7.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2021;43(8):600-607
To determine the concordance between the clinical diagnosis of women with abnormal vaginal discharge (AVD) and laboratory results using molecular detection and observation of the vaginal microbiota.
Cross-sectional study conducted in 2018 in Temuco, Chile. A total of 25 midwives from 12 health centers participated. A total of 125 women>18 years old, volunteers, were recruited. The sample of the posterior vaginal fornix was obtained by speculoscopy. Characteristics of the discharge and of the external and internal genitalia were observed. Gram staining was used to observe vaginal microbiota, blastoconidia and pseudohyphae, and polymerase chain reaction was used for the detection of Trichomonas vaginalis and Candida albicans. The Cohen kappa coefficient was used in the concordance analysis.
Out of a total of 125 women with AVD, 85.6% consulted spontaneously and 14.4% were diagnosed clinically during a routine check-up. Absolute concordance was significant (p=0.0012), with an agreement of 13.6%. The relative concordance was significant, but fair for bacterial vaginosis (Kappa=0.21; p=0.003) and candidiasis (Kappa=0.22; p=0.001), and slight for trichomoniasis (Kappa=0.14; p=0.009). The percentage of coincidence of the diagnoses (single or mixed) by laboratory and midwives was: bacterial vaginosis 63.2% (12/19), candidiasis 36.5% (27/74), and trichomoniasis 12.5% (4/32). There was 20% coinfection. A total of 36% of the clinical diagnoses of AVD had negative laboratory tests.
The vulvovaginitis conditions candidiasis and trichomoniasis appear to be overdiagnosed, and bacterial vaginosis appears to be underdiagnosed by the clinical diagnosis when compared with the laboratory diagnosis. The low concordance obtained shows the importance of complementing the clinical diagnosis with a laboratory study of AVD, particularly in women with failed treatments and/or coinfections with unspecific and varying signs and symptoms.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2021;43(8):595-599
To describe the hematological changes, the platelet indices in particular, in pregnant women with coronavirus disease 2019 (COVID-19) compared to healthy pregnant women.
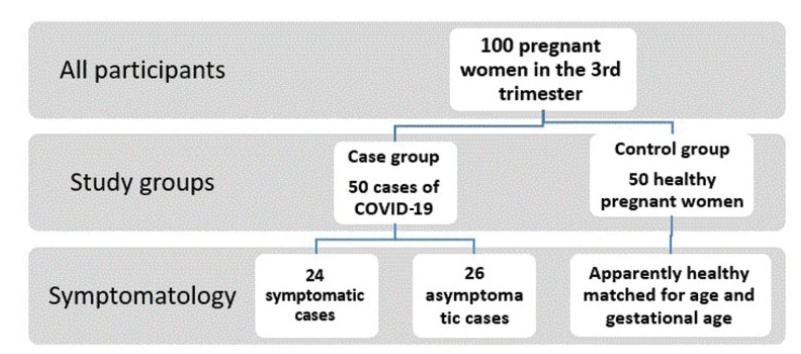
A retrospective case-control study conducted at the Al Yarmouk Teaching Hospital, in Baghdad, Iraq, involving 100 pregnant women, 50 with positive viral DNA for COVID-19 (case group), and 50 with negative results (control group); both groups were subjected to a thorough hematological evaluation.
Among the main hematological variables analyzed, the platelet indices, namely the mean platelet volume (MPV) and the platelet distribution width (PDW), showed statistically significant differences (MPV: 10.87±66.92 fL for the case group versus 9.84±1.2 fL for the control group; PDW: 14.82±3.18 fL for the case group versus 13.3±2.16 fL for the controls). The criterionvalue of the receiver operating characteristic (ROC) curve forPDWat a cutoffpoint of>11.8 fL showed a weak diagnostic marker, while the MPV at a cutoff value of>10.17 fL showed a good diagnostic marker.
The MPV and PDW are significantly affected by the this viral infection, even in asymptomatic confirmed cases, and we recommend that both parameters be included in the diagnostic panel of this infection.