Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2022;44(11):1032-1039
To determine how many patients underwent screening for diabetes mellitus (DM) in the puerperium after a diagnosis of gestational DM (GDM) and which factors were related to its performance.
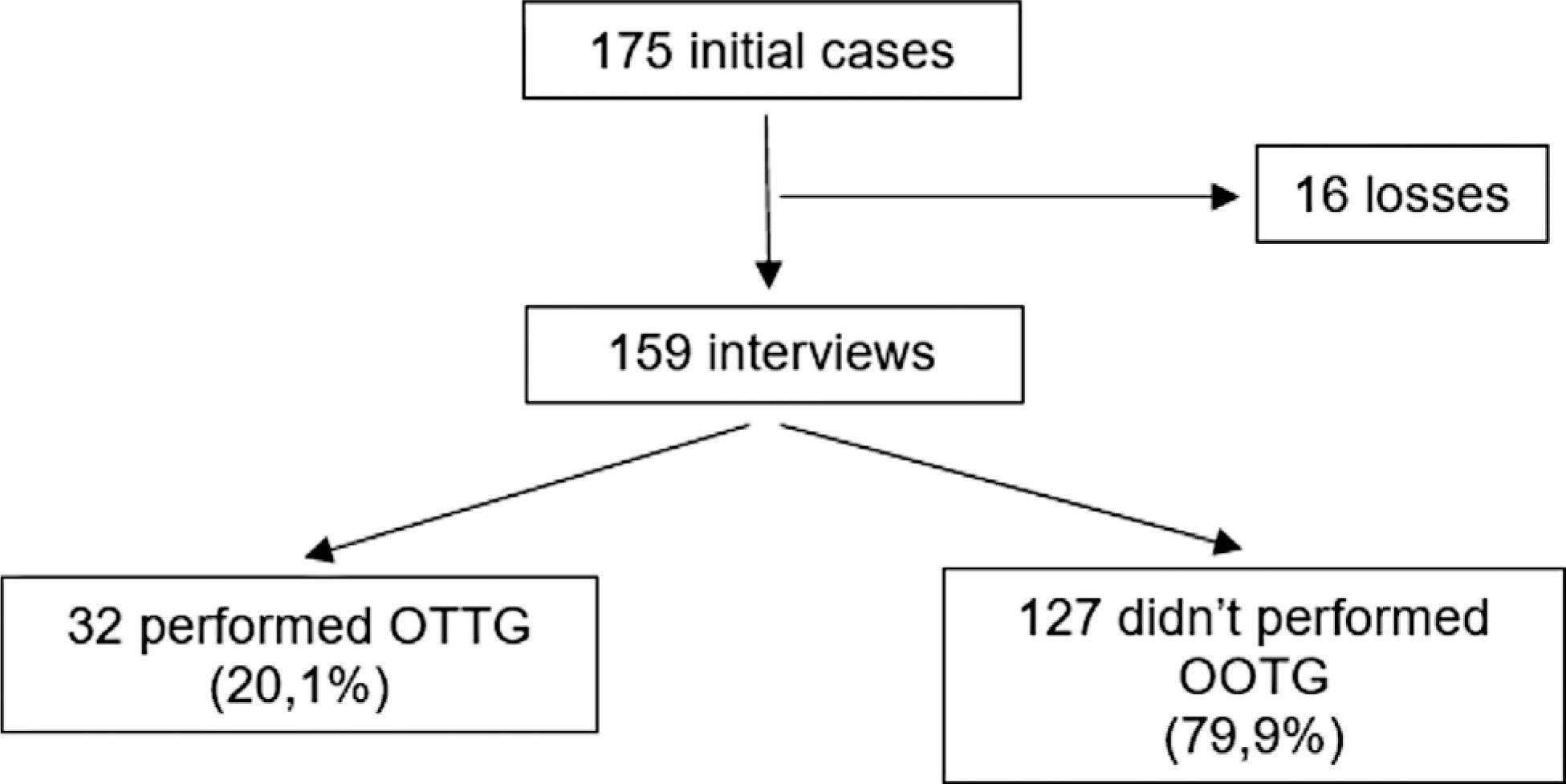
The present is a prospective cohort study with 175 women with a diagnosis of GDM. Sociodemographic and clinico-obstetric data were collected through a questionnaire and a screening test for DM was requested six weeks postpartum. After ten weeks, the researchers contacted the patients by telephone with questions about the performance of the screening. The categorical variables were expressed as absolute and relative frequencies. The measure of association was the relative risk with a 95% confidence interval (95%CI), and values of p ≤ 0.05 were considered statistically significant and tested through logistic regression.
The survey was completed by 159 patients, 32 (20.1%) of whom underwent puerperal screening. The mean age of the sample was of 30.7 years, and most patients were white (57.9%), married (56.6%), and had had 8 or more years of schooling (72.3%). About 22.6% of the patients used medications to treat GDM, 30.8% had other comorbidities, and 76.7% attended the postnatal appointment. Attendance at the postpartum appointment, the use of medication, and the presence of comorbidities showed an association with the performance of the oral glucose tolerance test in the puerperium.
The prevalence of screening for DM six weeks postpartum is low in women previously diagnosed with GDM. Patients who attended the postpartum consultation, used medications to treat GDM, and had comorbidities were the most adherent to the puerperal screening. We need strategies to increase the rate of performance of this exam.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2022;44(11):1052-1058
Nipple-sparing mastectomy (NSM) has been traditionally used in selected cases with tumor-to-nipple distance > 2 cm and negative frozen section of the base of the nipple. Recommending NSM in unselected populations remains controversial. The present study evaluated the oncological outcomes of patients submitted to NSM in an unselected population seen at a single center.
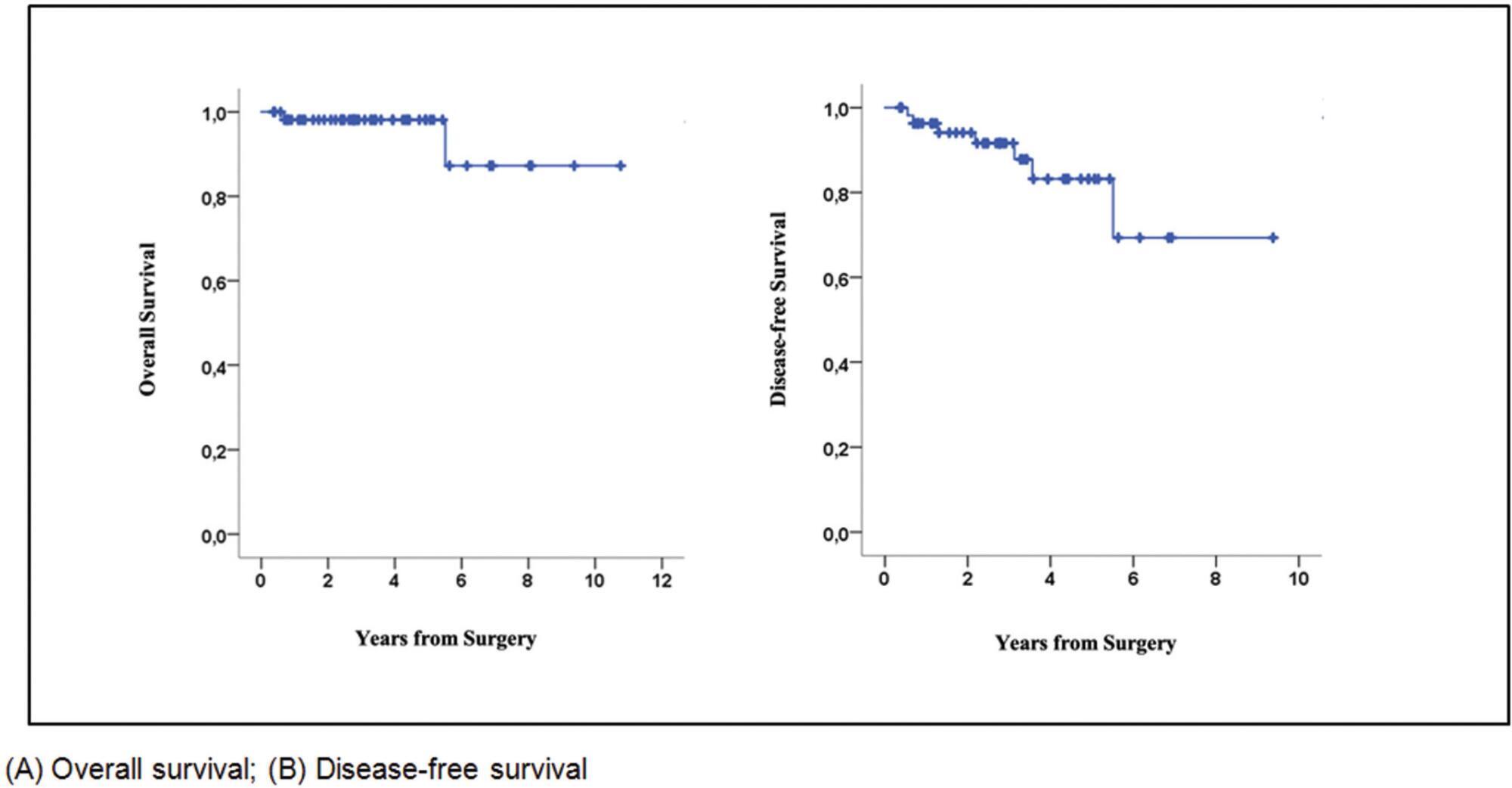
This retrospective cohort study included unselected patients with invasive carcinoma or ductal carcinoma in situ (DCIS) who underwent NSM in 2010 to 2020. The endpoints were locoregional recurrence, disease-free survival (DFS), and overall survival (OS), irrespective of tumor size or tumor-to-nipple distance.
Seventy-six patients (mean age 46.1 years) (58 invasive carcinomas/18 DCIS) were included. The most invasive carcinomas were hormone-positive (60%) (HER2 overexpression: 24%; triple-negative: 16%), while 39% of DCIS were high-grade. Invasive carcinomas were T2 in 66% of cases, with axillary metastases in 38%. Surgical margins were all negative. All patients with invasive carcinoma received systemic treatment and 38% underwent radiotherapy. After a mean of 34.8 months, 3 patients with invasive carcinoma (5.1%) and 1 with DCIS (5.5%) had local recurrence. Two patients had distant metastasis and died during follow-up. The 5-year OS and DFS rates for invasive carcinoma were 98% and 83%, respectively.
In unselected cases, the 5-year oncological outcomes following NSM were found to be acceptable and comparable to previous reports. Further studies are required.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2022;44(11):1047-1051
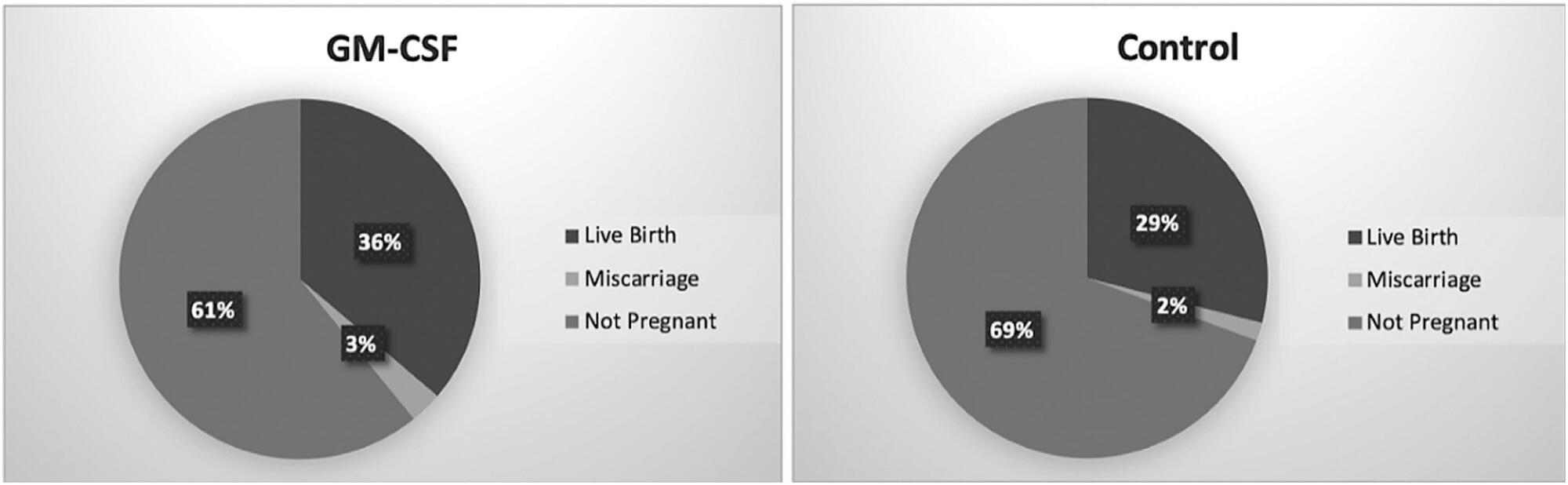
The use of granulocyte macrophage colony-stimulating factor (GM-CSF)-containing medium, which is a commercial medium that is used for cultivation of embryos in in vitro fertilization (IVF) treatments, has been suggested to increase the efficiency of this procedure in patients with previous multiple unsuccessful attempts. In this retrospective study, we analyzed GM-CSF-containing embryo culture media compared with traditional culture media in terms of development of embryos, pregnancy, and ongoing pregnancy success and live birth rates.
This is a prospective case control study conducted in a single center. A total of 131 unexplained infertility patients were included in the study. A cohort of 69 patients whose embryos were cultured in GM-CSF-containing medium and a control group of 62 age-matched patients whose embryos were cultured in conventional Sage One Step medium were included in the study. The major study outcomes were achievement of pregnancy and ongoing pregnancy rate at 12 weeks of gestation.
The pregnancy and ongoing pregnancy rates of the patients whose embryos were cultured in GM-CSF-containing medium were 39.13% and 36.23%, respectively. These were higher than the rates of the control group, which were 30.65% and 29.03%, respectively, although this difference was not statistically significant. In addition, the 5th-day embryo transfer percentage in the GM-CSF group was higher than in the control group (34.78% versus 27.4%).
The main findings of our study were that there was no difference between the GM-CSF-enhanced medium and the control group in terms of our major study outcomes. However, blastomere inequality rate and embryo fragmentation rates were lower in the GM-CSF group.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2022;44(11):1040-1046
The purpose was to assess the rates of postoperative complications and the need of temporary stoma of laparoscopic surgical treatment for bowel endometriosis in a referral center.
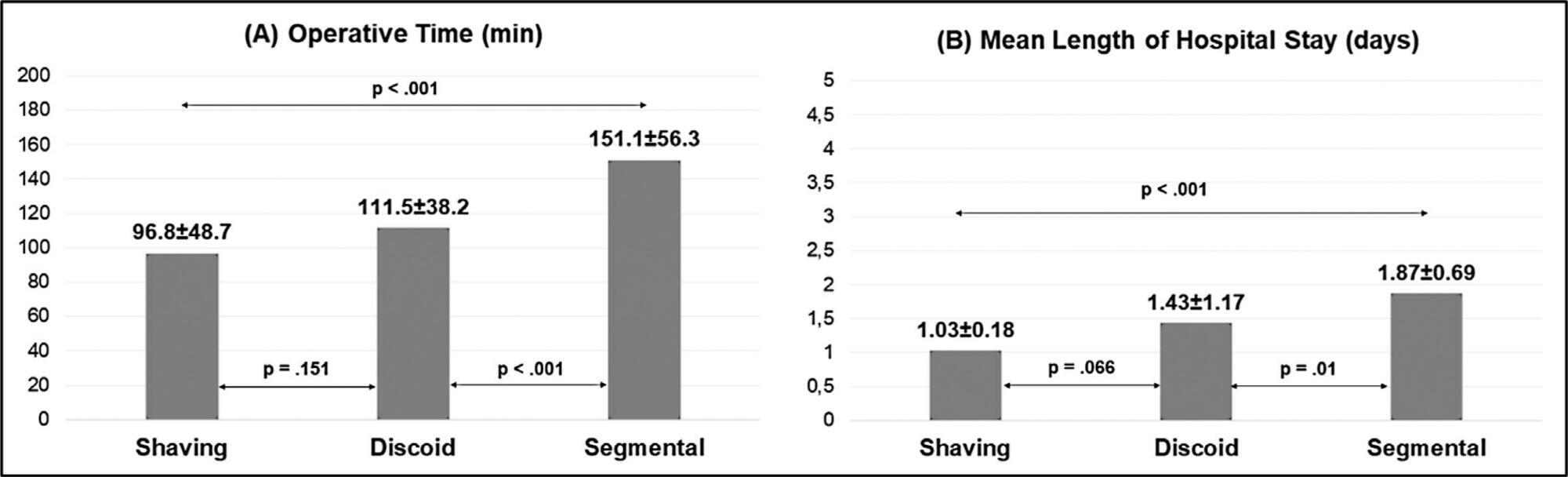
The surgical indication, type of operation, operative time, length of hospital stay, need for a temporary stoma, rate of conversion to open surgery, postoperative complications were evaluated.
One-hundred and fifty patients were included. The average duration of surgery was significantly longer for segmental resection (151 minutes) than for disc excision (111.5 minutes, p < 0.001) and shaving (96.8 minutes, p < 0.001). Patients with segmental resection had longer postoperative lengths of hospital stay (1.87 days) compared with patients with disc excision (1.43 days, p < 0.001) and shaving (1.03 days, p < 0.001). A temporary stoma was performed in 2.7% of patients. Grade II and III postoperative complications occurred in 6.7% and 4.7% patients, respectively.
Laparoscopic intestinal resection has an acceptable postoperative complication rate and a low need for a temporary stoma.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2022;44(11):1021-1031
To develop and validate a protocol for the use of the Dietary Guidelines for the Brazilian Population (DGBP) in the individual dietary advice for pregnant women assisted in primary healthcare (PHC).
Methodological study that involved the elaboration of a protocol in six steps: definition of the format, definition of the instrument to evaluate food consumption, systematization of evidence on food and nutrition needs of pregnant women, extraction of DGBP recommendations, development of messages of dietary guidelines and content, and face validity. The analyses of the validation steps were carried out by calculating the Content Validity Index (CVI) and thematic content analysis.
As products of the steps, the protocol structure was defined and the dietary advice for pregnant women were elaborated, considering physiological changes, food consumption, nutritional and health needs, and socioeconomic conditions of this population. The protocol was well evaluated by experts and health professionals in terms of clarity, relevance (CVI > 0.8), and applicability. In addition, the participants made some suggestions to improve the clarity of the messages and to expand the applicability of the instrument with Brazilian pregnant women.
The instrument developed fills a gap in clinical protocols on dietary advice for pregnant women focused on promoting a healthy diet, contributing to a healthy pregnancy. In addition, it demonstrates potential to contribute to the qualification of PHC professionals and to the implementation of the DGBP recommendations.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2022;44(11):1014-1020
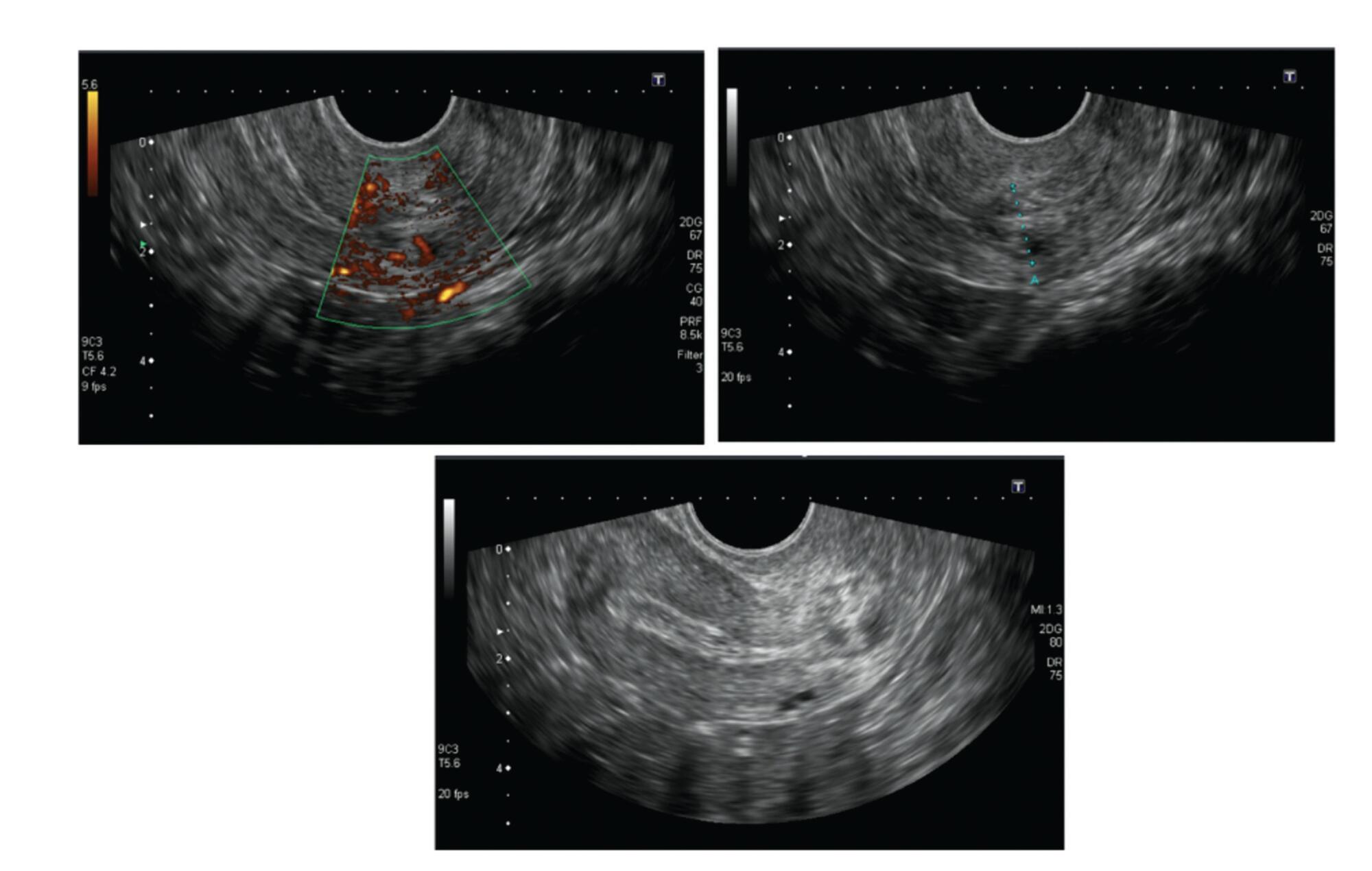
Cervical pregnancy is challenging for the medical community, as it is potentially fatal. The treatment can be medical or surgical; however, there are no protocols that establish the best option for each case. The objective of the present study was to describe the cases of cervical pregnancy admitted to a tertiary university hospital over a period of 18 years.
A retrospective study based on a review of the medical records of all cervical pregnancies admitted to the Women's Hospital at Universidade Estadual de Campinas, Southeastern Brazil, from 2000 to 2018.
We identified 13 cases of cervical pregnancy out of a total of 673 ectopic pregnancies; only 1 case was initially treated with surgery because of hemodynamic instability. Of the 12 cases treated conservatively, 7 were treated with single-dose intramuscular methotrexate, 1, with intravenous and intramuscular methotrexate, 1, with intravenous methotrexate, 1, with 2 doses of intramuscular methotrexate, and 2, with intra-amniotic methotrexate. Of these cases, one had a therapeutic failure that required a hysterectomy. Two women received blood transfusions. Four women required cervical tamponade with a Foley catheter balloon for hemostasis. There was no fatal outcome.
Cervical pregnancy is a rare and challenging condition from diagnosis to treatment. Conservative treatment was the primary method of therapy used, with satisfactory results. In cases of increased bleeding, cervical curettage was the initial treatment, and it was associated with the use of a cervical balloon for hemostasis.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2022;44(10):945-952
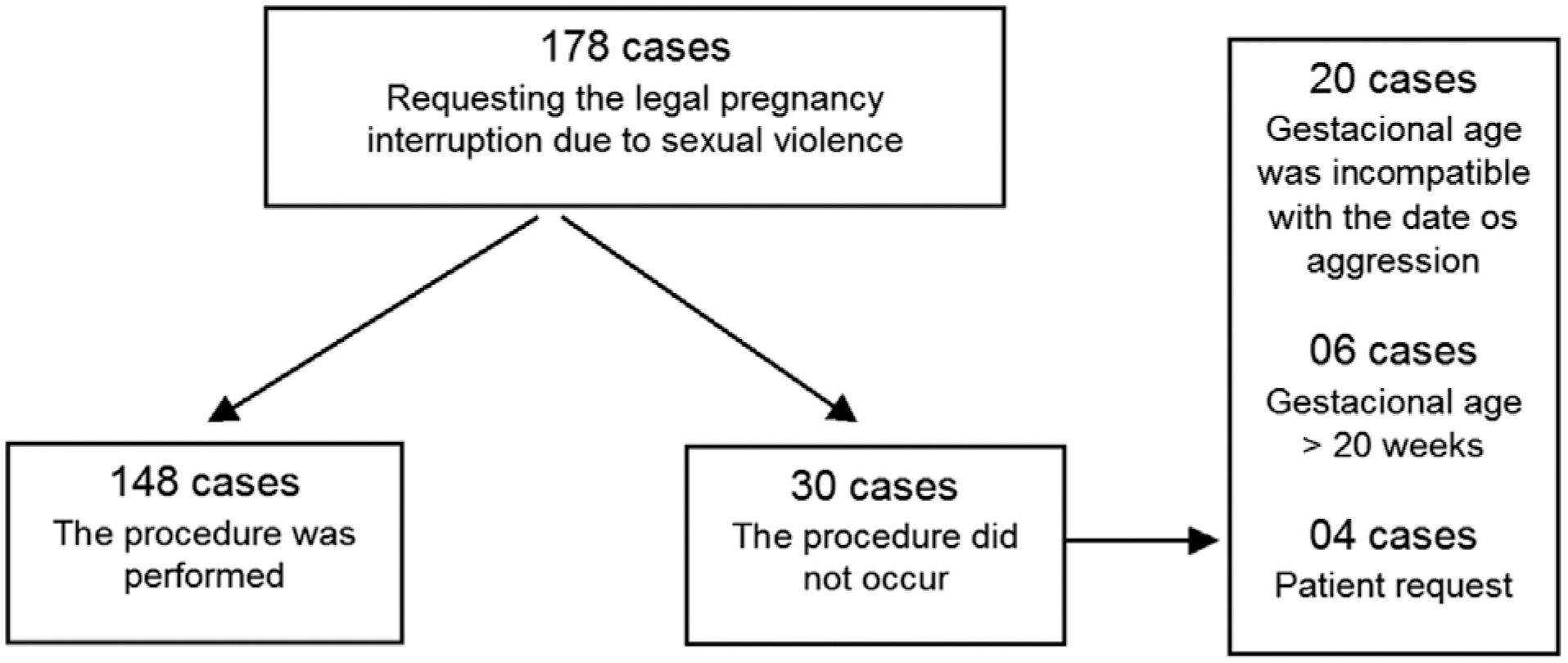
To analyze the cases of all women who attend to a service of legal termination of pregnancy in cases of sexual violence in a public reference hospital and to identify the factors related to its execution.
Cross-sectional observational study with information from medical records from January 2014 to December 2020. A total of 178 cases were included, with an evaluation of the data referring to the women who attended due to sexual violence, characteristics of sexual violence, hospital care, techniques used, and complications. The analysis was presented in relative and absolute frequencies, medians, means, and standard deviation. Factors related to the completion of the procedure were assessed using binary logistic regression.
Termination of pregnancy was performed in 83.2% of the cases; in 75.7% of the cases, the technique used was the association of transvaginal misoprostol and intrauterine manual aspiration. There were no deaths, and the rate of complications was 1.4%. Gestational age at the time the patient's sought assistance was the determining factor for the protocol not being completed. Pregnancies up to 12 weeks were associated with a lower chance of the interruption not occurring (odds ratio [OR]: 0.41; 95% confidence interval [CI]: 0.12–0.88), while cases with gestational age > 20 weeks were associated with a greater chance of the interruption not happening (OR: 29.93; 95%CI: 3.91–271.50).
The service studied was effective, with gestational age being the significant factor for resolution.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2022;44(10):938-944
To assess the association between two colposcopic indices, the Swede score and the 2011 International Federation of Cervical Pathology and Colposcopy (IFCPC) Nomenclature as well as to determine the efficacy of the Swede score with cutoffs of 7 and 8.
In the present cross-sectional pilot study, 34 women who had at least 1 colposcopy-directed biopsy due to abnormal cytology were enrolled. The colposcopic findings were scored by both the Swede score and the 2011 IFCPC Nomenclature and were compared with each other. The Kappa coefficient and the McNemar test were used. Accuracy, sensitivity, specificity, and positive and negative predictive values (NPV and PPV, respectively) were calculated, as well as the effectiveness with cutoffs of 7 and 8 in identifying cervical intraepithelial neoplasm (CIN) 2+ when using the Swede score.
The correlation between the 2 colposcopic indices was 79.41%. The Kappa coefficient and the McNemar p-value were 0.55 and 0.37, respectively. The IFCPC Nomenclature had sensitivity, specificity, accuracy, PPV, and NPV of 85.71, 55.00, 67.64, 57.14, and 84.61%, respectively. The Swede score had sensitivity, specificity, accuracy, PPV, and NPV of 100, 63.15, 79.41, 68.18, and 100%, respectively. A Swede score cutoff of 7 for CIN 2+ detection had a specificity of 94.73%, while with a cutoff of 8 it increased to 100%. The sensitivity for both values was 60%. The PPV and NPV for cutoffs of 7 and 8 were 90 and 75 and 100 and 76%, respectively.
Although both colposcopic indices have good reproducibility, the Swede score showed greater accuracy, sensitivity, and specificity in identifying CIN 2 + , especially when using a cutoff of 8.