Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2019;41(6):371-378
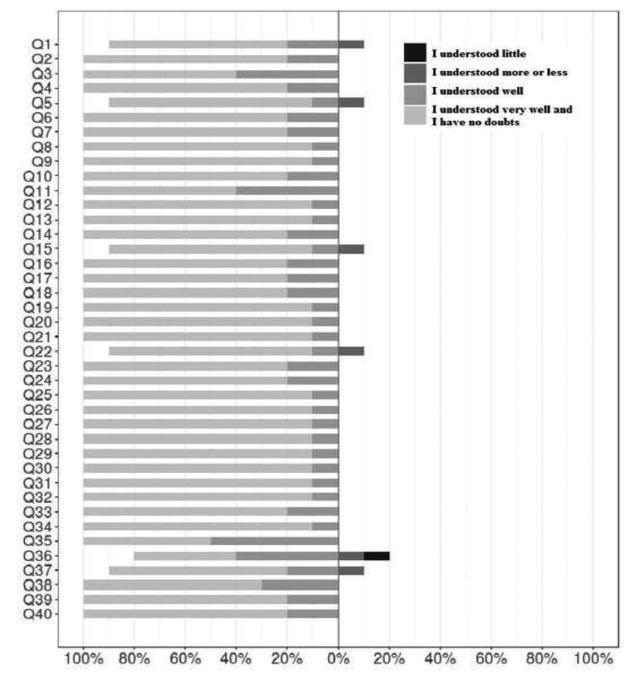
The aim of this study was to determine the content and face validity of the Mackey Childbirth Satisfaction Rating Scale (MCSRS) questionnaire cross-culturally adapted to Brazilian Portuguese.
The MCSRS is a questionnaire with 34 items related to childbirth satisfaction. The forward- and back-translated versions were compared with the original material, and 10 experts analyzed each item according to the following criteria: clarity, semantic equivalence, appropriateness, and cultural relevance. The final version was presented to 10 mothers for face validation to ensure the questionnaire would suit the target population.
The total of 34 items assessed by experts for clarity, semantic equivalence, appropriateness, and relevance showed positive agreement of 0.85, 0.92, 0.97 and 0.97; negative agreement of 0.13, 0.09, 0.04 and 0.04; and total agreement of 0.75; 0.85, 0.94 and 0.94, respectively. Multilevel linear modeling was applied with crossed random effects and with nested random effects for each judge. The intercept of each criterion was as follows: clarity, 0.87; semantic equivalence, 0.92; appropriateness, 0.96; and cultural relevance, 0.96. The overall mean of agreement was 92.8%. The face validity measurement yielded 80% of agreement on the items, all of them clearly understood.
The final version of the Brazilian Portuguese MCSRS questionnaire had face and content validity confirmed. This instrument of evaluation of maternal satisfaction during childbirth was validated to be applied in the Brazilian female population.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2019;41(6):363-370
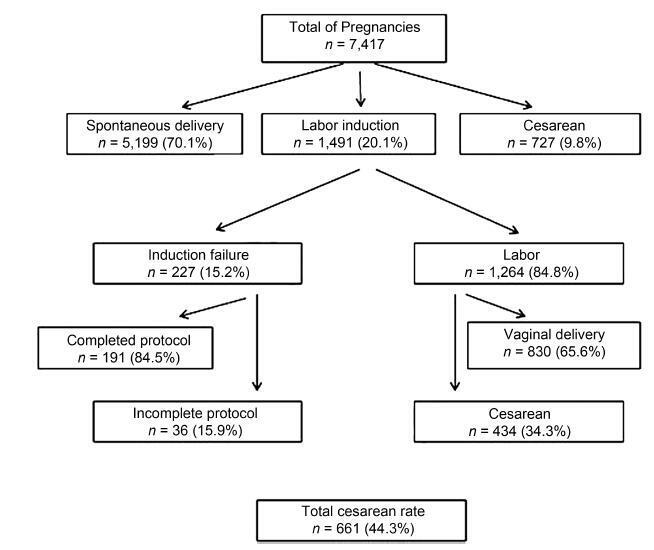
To evaluate the results of induced labor and to determine the main factors associated with intrapartum cesarean section after patients being submitted to this procedure at the Hospital Universitário of the Universidade Federal de Santa Catarina (HU/UFSC, in the Portuguese acronym), Florianópolis, state of Santa Catarina, Brazil.
A retrospective cross-sectional study that included all the pregnancies that resulted in single-fetus births, whose gestational-age was > 22 weeks and that had been submitted to labor induction at the HU/UFSC in the period from 2013 to 2016.
During the proposed period, 1,491 pregnant women were submitted to the labor induction protocol. In 1,264 cases (84.8%), induction resulted in labor, with 830 (65.7%) progressing to vaginal delivery. Gestational age ≥ 41 + 0 weekswas themost common indication for induced labor (55.2%), and vaginal administration of misoprostol was themost commonly usedmethod (72.0%). Among these pregnant women, the cesarean section rate was of 34.3%. Considering the cases of induction failure, the cesarean section rate rose to 44.3%. The factors associated with cesarean section were: previous history of cesarean delivery (PR [prevalence ratio] = 1.48; 95%CI [confidence interval]: 1.51-1.88), fetuses with intrauterine growth restriction (IUGR) (PR = 1.82; 95%CI: 1.32-2.19), Bishop score ≤ 6 (PR = 1.33; 95%CI: 1.01-1.82), and induction time either < 12 hours (PR = 1.44; 95%CI: 1.17-1.66) or > 36 hours (PR = 1.51; 95% CI 1.22-1.92) between the beginning of the induction and the birth.
Labor induction was successful inmost patients. In the cases in which the final outcome was a cesarean section, the most strongly associated factors were: previous history of cesarean delivery, presence of fetuses with IUGR, and either excessively short or excessively long periods of induction.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2019;41(5):312-317
To evaluate the quality of life among university students with premenstrual syndrome (PMS).
The cross-sectional study was conducted at the Faculdade Pernambucana de Saúde, in Recife, Brazil, between August 2016 and July 2017. Sociodemographic, gynecological, and lifestyle variables, and PMS occurrence, were investigated among 642 students. The short form of the World Health Organization Quality of Life (WHOQOL Bref) questionnaire was used to evaluate four domains of the quality of life of the students: physical, mental, social relationships, and environmental. The American College of Obstetricians and Gynecologists’ criteria were used to define PMS.
Of the 642 students, 49.9% had PMS, 23.3% had mild PMS and 26.6% had premenstrual dysphoric disorder (PMDD). Most of the students were between 18 and 24 years old, had regular menstrual cycles, and practiced physical activity. Regarding the physical and mental domains of the WHOQOL-Bref questionnaire, a statisticallysignificant difference was observed between the students who did not have and those who had mild or PMDD (p < 0.001). A difference was also found between the students who did not have PMS and those who had mild PMS in the social relationships (p = 0.001) and environmental domains (p = 0.009).
Mild PMS and PMDD are prevalent among university students on healthrelated courses, and the syndrome can affect the students’ self-assessment of all the domains of quality of life.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2019;41(5):306-311
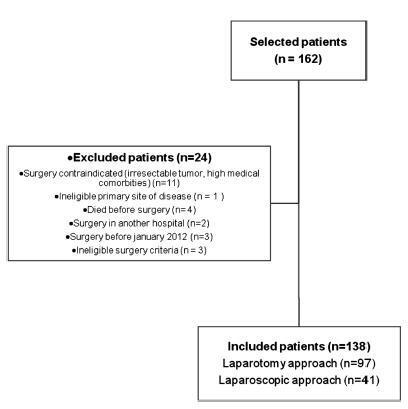
To compare laparoscopy with laparotomy for surgical staging of endometrial cancer.
A cohort of women with preoperative diagnosis of endometrial cancer who underwent surgical staging was retrospectively evaluated. The main study end points were: morbidity and mortality, hospital length of stay, perioperative adverse events and recurrence rate. Data analysis was performed with the software SPSS v25 (IBM Corp., Armonk, NY, USA), categorical variables using a Chi-square and Fisher test, and continuous variables using the Student t-test.
Atotal of 162 patientswere analyzed. 138 patientsmet the inclusion criteria, 41of whom underwent staging by laparoscopy and 97 by laparotomy. Conversions from laparoscopy to laparotomy happened in 2 patients (4.9%) and were secondary to technical difficulties and poor exposure. Laparoscopy had fewer postoperative adverse events when compared with laparotomy (7.3% vs 23.7%, respectively; p = 0.005), but similar rates of intraoperative complications, despite having a significantly longer operative time (median, 175 vs 130 minutes, respectively; p < 0.001). Hospital stay was significantly lower in laparoscopy versus laparotomy patients (median, 3 vs 7 days, respectively; p < 0.001). No difference in recurrence or mortality rates were observed.
Laparoscopic surgical staging for endometrial cancer is feasible and safe. Patients have lower postoperative complication rates and shorter hospital stays when compared with the approach by laparotomy.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2019;41(5):298-305
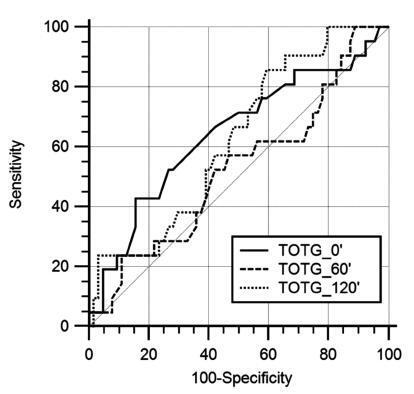
Gestational diabetes mellitus (GDM) is associated with a higher risk of perinatal morbidity and mortality, and its main complication is the occurrence of large for gestational age (LGA) newborns. The present study aims to characterize pregnant women with GDM and to identify factors associated with the occurrence of LGA newborns in this population.
A cross-sectional study was performed based on medical records of women whose prenatal care and delivery were performed at the Maternal and Child Unit of the HospitalUniversitário of theUniversidade Federal doMaranhão, state of Maranhão, Brazil.A total of 116 pregnant women diagnosed with GDMwere included according to the criteria of the International Association of Diabetes and Pregnancy Study Groups (IADPSG).
The variables associated with LGA newborns after multivariate analysis were: obesity prior to pregnancy (OR = 11.6; 95% CI: 1.40-95.9), previous macrosomia (OR = 34.7; 95% CI: 4.08-295.3), high blood glucose levels in the 3rd trimester (OR = 2,67; 95% CI: 1.01-7.12) and combined change in the oral glucose tolerance test (OGTT) (fasting + postdextrose) (OR = 3.53;95%CI:1.25-14.2) = 1.17-10.6).Otherwise, insufficientweight gain during pregnancy reduced the risk for LGA newborns (OR = 0.04; 95% CI: 0.01-0.32).
Obesity prior to pregnancy, previous macrosomia, high blood glucose levels in the 3rd trimester, and combined change in the OGTT were independent predictive factors for LGA newborns in pregnant women with GDM.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2019;41(5):291-297
To evaluate the level of information possessed by pregnant adolescents regarding the human papillomavirus (HPV).
Descriptive study developed in the adolescent prenatal outpatient clinic of a tertiary hospital fromthe state of São Paulo, Brazil. Data were collected between June and December 2017 following approval from the ethics and research committee (CAAE: 1.887.892/2017). Pregnant adolescents, ≤18 years old, who attended the abovementioned outpatient section, composed the sample. Those diagnosed with a psychiatric disorder and those with hearing or cognitive disabilities were excluded. After acceptance to participate in the present study, the pregnant adolescents signed an Informed Consent Form. Regarding the statistical analysis, the chi-squared test and the Fisher exact test were used.
Regarding the knowledge about HPV, 123 (80.92%) of the participants had already heard about the subject; for 77 (50.66%), their schools had been the source of the information; 101 (66.45%) did not know how they could be infected by the virus. Age variation did not influence their knowledge on how to prevent themselves from HPV (p = 0.2562). The variable vaccine is associated with HPV prevention (p < 0.0001).
The pregnant adolescents composing the sample have shown to have knowledge about HPV. However, they do not prevent themselves from it appropriately, given that little more than half of the sample was vaccinated, had not reported an understanding that the use of preservatives and vaccination are effective means of prevention, and did not correlate HPV with uterine cervical cancer.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2019;41(5):280-290
To evaluate and compare the prevalence of structural congenital anomalies (CAs) according to maternal body mass index (BMI).
The present cross-sectional study involved pregnant women with fetuses diagnosed with structural CAs through morphological ultrasonography between November 2014 and January 2016. The nutritional status of the pregnant women was classified according to the gross value of the body mass index. The pregnant women were categorized into four groups: low weight, adequate weight, overweight, and obesity. Statistical analysis was performed using Stata/SE version 12.0 (Stata Corporation, College Station, TX), with values of p ≤ 0.05 considered statistically significant.
A total of 223 pregnant women had fetuses diagnosed with CAs. The prevalence of structural CAs in pregnant women with lowweight was of 20.18%, of 43.50% in pregnant women with adequate weight, of 22.87% in pregnant women with overweight, and of 13.45% in pregnant women with obesity. The prevalence of central nervous system (CNS) anomalies and of genitourinary systemanomalieswas high for the four groups of pregnant women. A positive association was observed between multiple anomalies in pregnant women with adequate weight (prevalence ratio [PR] = 1.65; p ≤ 0.004) and between anomalies of the lymphatic system in obese pregnant women (PR = 4.04, p ≤ 0.000).
The prevalence of CNS and genitourinary systemanomalies was high in all of the BMI categories. Obese pregnancies were associated with lymphatic system anomalies. Therefore, screening and identification of the risk factors for CAs are important, regardless of the maternal BMI. Our findings reinforce the importance of discussing with pregnant women maternal nutrition and its effect on fetal development and on neonatal outcome.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2019;41(3):176-182
The aim of the present study was to describe and analyze data of 57 women with borderline ovarian tumors (BOTs) regarding histological characteristics, clinical features and treatment management at the Department of Obstetrics and Gynecology of the Universidade Estadual de Campinas (Unicamp, in the Portuguese acronym).
The present retrospective study analyzed data obtained from clinical and histopathological reports of women with BOTs treated in a single cancer center between 2010 and 2018.
A total of 57 women were included, with a mean age of 48.42 years old (15.43- 80.77), of which 30 (52.63%) were postmenopausal, and 18 (31.58%) were < 40 years old. All of the women underwent surgery. A total of 37 women (64.91%) were submitted to complete surgical staging for BOT, and none (0/57) were submitted to pelvic or paraortic lymphadenectomy. Chemotherapy was administered for two patients who recurred. The final histological diagnoses were: serous in 20 (35.09%) cases, mucinous in 26 (45.61%), seromucinous in 10 (17.54%), and endometrioid in 1 (1.75%) case. Intraoperative analyses of frozen sections were obtained in 42 (73.68%) women, of which 28 (66.67%) matched with the final diagnosis. The mean follow-up was of 42.79 months (range: 2.03-104.87 months). Regard ingthe current status of the women, 45(78.95%) are alive without disease, 2(3.51%) arealive with disease, 9 (15.79%) had their last follow-up visit > 1 year beforethe performanceof the present study but arealive, and 1 patient(1.75%) died of another cause.
Women in the present study were treated according to the current guidelines and only two patients recurred.