Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2022;44(3):245-250
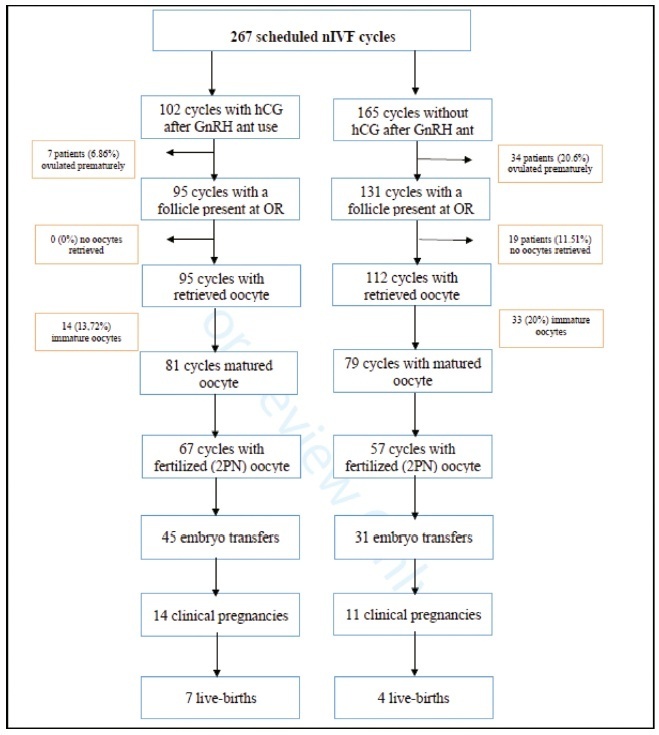
The aim of the present retrospective study was to investigate the effectiveness of single-dose gonadotropin releasing hormone (GnRH) antagonist administration, the day after human chorionic gonadotropin (hCG) triggering for final oocyte maturation, on the prevention of premature luteinization in patients with diminished ovarian reserve in in-vitro fertilization (IVF) cycles. The secondary objective of the study was to search the effect of this protocol on pregnancy outcomes.
This is a retrospective study including 267 infertile patients who have single antral follicle seen with ultrasonography on the 2nd or 3rd day of the menstrual cycle before starting IVF treatment. We randomized patients into two groups. The case group comprised patients who had single-dose GnRH antagonist injection the day after hCG triggering formed, and the patients who had the standard treatment regime formed the control group. In both groups, the oocytes were collected 36 hours after hCG injection.
The premature ovulation rate was significantly low in the case group compared with the control group (6.86 versus 20.6% per scheduled cycle) (p=0.022). Also, the oocyte retrieval rate (93.14 versus 67.87% per scheduled cycle) (p=0.013), the oocyte maturity rate (79.42 versus 47.87%) (p=0.041), the fertilization rate (65.68 versus 34.54%) (p=0.018), and the embryo transfer rate per scheduled cycle (44.11 versus 18.78%) (p=0.003) were higher in the GnRH antagonist group than in the control group.
The administration of GnRH antagonist the day after hCG trigger in IVF treatments of patients with diminished ovarian reserve enabled a significant decrease in the rate of premature ovulation but had no effect on live birth rate.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2022;44(3):238-244
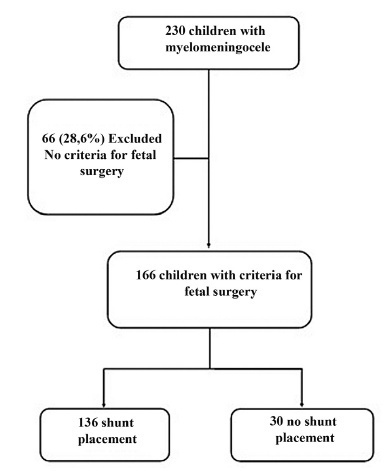
To analyze the historical clinical outcomes of children with myelomeningocele (MMC) meeting the criteria for fetal surgery, but who underwent postnatal primary repair.
Data from children undergoing postnatal MMC repair between January 1995 and January 2015 were collected from the Neurosurgery Outpatient Clinic’s medical records. Children were included if they had ≥1 year of postoperative follow-up andmet the criteria for fetal surgery. The children’s data were then stratified according to whether they received a shunt or not. The primary outcome was mortality, and secondary outcomes were educational delays, hospitalization, recurrent urinary tract infections (UTIs), and renal failure.
Over the 20-year period, 231 children with MMC were followed up. Based on clinical data recorded at the time of birth, 165 (71.4%) qualify of fetal surgery. Of the 165 patients, 136 (82.4%) underwent shunt placement. The mortality rate was 5.1% in the group with shunt and 0% in the group without, relative risk (RR) 3.28 (95% confidence interval, 95% CI, 0.19-55.9). The statistically significant RRs for adverse outcomes in the shunted group were 1.86 (95% CI, 1.01-3.44) for UTI, 30 (95% CI, 1.01-537) for renal failure, and 1.77 (95% CI, 1.09-2.87) for hospitalizations.
Children with MMC qualifying for fetal surgery who underwent shunt placement were more likely to have recurrent UTIs, develop renal failure, and be hospitalized. Since approximately half of the shunt procedures could be avoided by fetal surgery, there is a clinical benefit and a possible financial benefit to the implementation of this technology in our setting.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2022;44(3):231-237
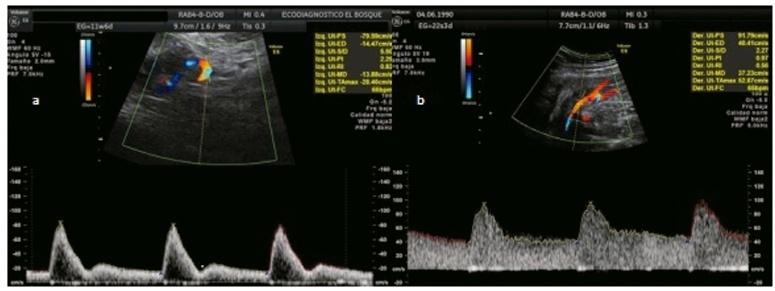
To analyze whether acetylsalicylic (ASA) intake modifies the mean uterine arteries pulsatility index (UtA-PI) at the 2nd or 3rd trimester in a cohort of pregnant women with abnormal mean UtA-PI at between 11 and 14 weeks of gestation.
This is a retrospective cohort study. Singleton pregnancies with abnormal mean UtA-PI at between 11 and 14 weeks of gestation were studied. The participants were divided into 3 groups: 1) If the participant did not take ASA during pregnancy; 2) If the participant took ASA before 14 weeks of gestation; and 3) If the participant took ASA after 14 weeks of gestation. The mean UtA-PI was evaluated at the 2nd and 3rd trimesters, and it was considered to improve when it decreased below the 95th percentile. The prevalence ratio (PR) and the number needed to treat (NNT) werecalculated.
A total of 72 participants with a mean UtA-PI>95th percentile at the 1st trimester of gestation were evaluated. Out of the 18 participants who took ASA, 8 participants started it before 14 weeks of gestation and 10 after. A total of 33.3% of these participants had improved the mean UtA-PI at the 2nd and 3rd trimesters of gestation, although it was not statistically significant (p=0.154). The prevalence ratio was 0.95 (95% confidence interval [CI]: 0.31-1.89), but between the 1st and 2nd trimesters of gestation, the PR was 0.92 (95%CI: 0.21-0.99) and it was statistically significant.
The present work demonstrates a modification of the mean UtA-PI in participants who took ASA compared with those who did not. It is important to check if ASA can modify the normal limits of uterine arteries because this could have an impact on surveillance.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2022;44(3):220-230
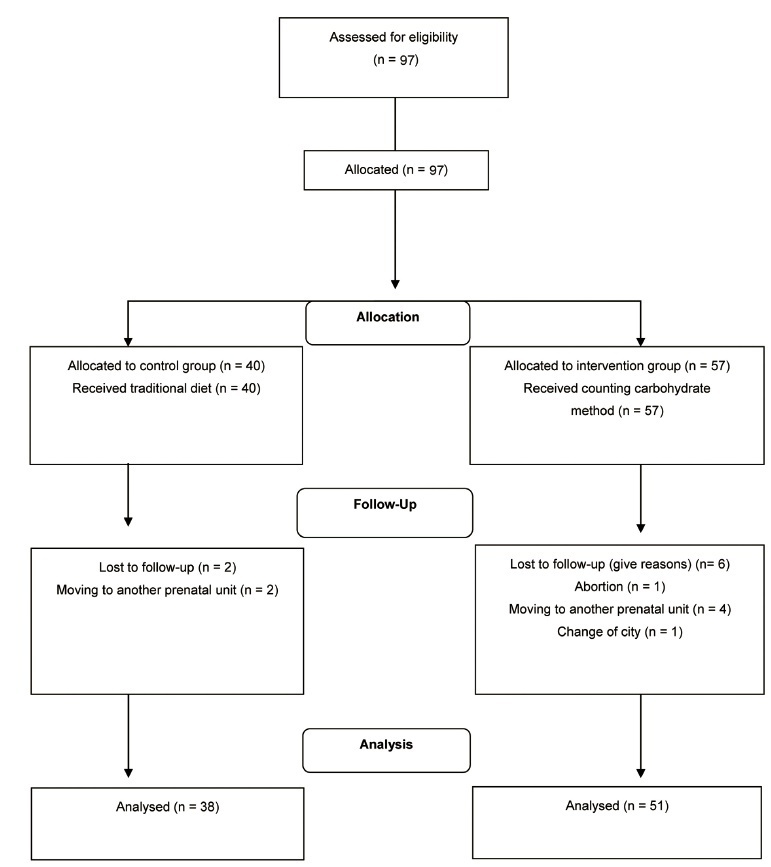
To evaluate the effect of the carbohydrate counting method (CCM) on glycemic control,maternal, and perinatal outcomes of pregnant women with pregestational diabetes mellitus (DM).
Nonrandomized controlled clinical trial performed with 89 pregnant women who had pregestational DMand received prenatal care in a public hospital in Rio de Janeiro, state of Rio de Janeiro, Brazil, between 2009 and 2014, subdivided into historic control group and intervention group, not simultaneous. The intervention group (n=51) received nutritional guidance from the carbohydrate counting method (CCM), and the historical control group (n=38), was guided by the traditionalmethod (TM). The Mann-Whitney test or the Wilcoxon test were used to compare intra- and intergroup outcomes andanalysis of variance (ANOVA) for repeated measures, corrected by the Bonferroni post-hoc test,was used to assess postprandial blood glucose.
Only the CCM group showed a reduction in fasting blood glucose. Postprandial blood glucose decreased in the 2nd (p=0.00) and 3rd (p=0.00) gestational trimester in the CCM group, while in the TM group the reduction occurred only in the 2nd trimester (p=0.015). For perinatal outcomes and hypertensive disorders of pregnancy, there were no differences between groups. Cesarean delivery was performed in 82% of the pregnant women and was associated with hypertensive disorders (gestational hypertension or pre-eclampsia; p=0.047).
Both methods of nutritional guidance contributed to the reduction of postprandial glycemia of women and no differences were observed for maternal and perinatal outcomes. However, CCM had a better effect on postprandial glycemia and only this method contributed to reducing fasting blood glucose throughout the intervention. ReBEC Clinical Trials Database The present study was registered in the ReBEC Clinical Trials Database (Registro Brasileiro de Ensaios Clínicos, number RBR-524z9n).
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2022;44(4):343-351
To evaluate the emotional and clinical aspects observed in women with gestational trophoblastic disease (GTD) followed-up in a reference center (RC) by a multidisciplinary team.
Retrospective cohort study of the clinical records of 186 women with GTD and of the emotional aspects (EA) observed in these women by a teamof psychologists and reported by the 389 support groups conducted from 2014 to 2018.
The women were young (mean age: 31.2 years), 47% had no living child, 60% had planned the pregnancy, and 50% participated in two or more SG. Most women (n=137; 73.6%) reached spontaneous remission ofmolar gestation in a median time of 10 weeks and had a total follow-up time of seven months. In the group of 49 women (26.3%) who progressed to gestational trophoblastic neoplasia (GTN), time to remission after chemotherapy was 18 weeks, and total follow-up time was 36 months. EA included different levels of anxiety and depression,more evident in 9.1% of the women; these symptoms tended to occur more frequently in women older than 40 years (p=0.067), less educated (p=0.054), and whose disease progressed to GTN (p=0.018), as well as in those who had to undergo multi-agent chemotherapy (p=0.028) or hysterectomy (p=0.001) adjuvant to clinical treatment.
This study found several EA in association with all types of GTD. It also highlights the importance of specialized care only found in a RC, essential to support the recovery of the mental health of these women.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2022;44(4):336-342
To evaluate clinical characteristics, maternal and fetal outcomes in pregnant women who underwent surgery for adnexal torsion (AT).
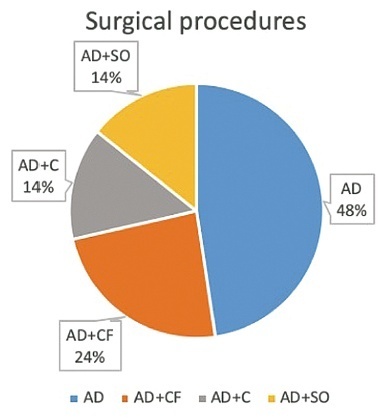
All patients, who underwent surgical operation due to AT during pregnancy at the Department of Obstetrics and Gynecology, School of Medicine, Ege University between 2005 and 2020 were retrospectively investigated. Main clinical and perioperative outcomes were evaluated.
A total of 21 patients who underwent surgery due to AT during pregnancy were included. Of all patients, 61.9% underwent laparoscopy and the remaining 38.1% underwent laparotomy. The most common surgical procedure was adnexal detorsion in both groups (48%). Mean gestational age at the time of diagnosis, duration of surgery and hospitalization were significantly lower in the laparoscopy group, when compared with the laparotomy group (p=0.006, p=0.001, and p=0.001, respectively.) One of the patients had an infection during the postoperative period. Spontaneous abortion was only observed in one case.
It can be concluded that the surgical intervention implemented for the exact diagnosis and treatment of AT (laparotomy or laparoscopy) did not have an unfavorable effect on pregnancy outcomes such as abortion, preterm delivery, and fetal anomaly. However, laparoscopy may be superior to laparotomy in terms of advantages.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2022;44(3):214-219
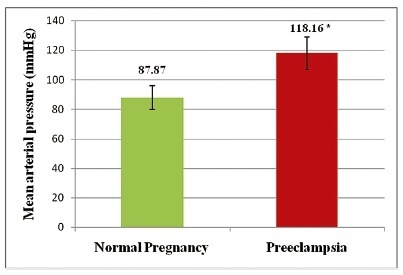
To assess the influence of oxidative stress on the gene expression of nitric oxide synthases (NOS 3 and NOS 2) and, hence, the cardiovascular responses in preeclampsia.
This was a case control study in which patients with preeclampsia (PE group) and normal pregnancy controls (NP group) were included according to the guidelines of the American College of Obstetricians and Gynecologists (ACOG). The serum levels of malondialdehyde (MDA), total antioxidant capacity, and nitric oxide (NO) were estimated, and the heart rate andmean arterial pressure were recorded. The gene profiling of NOS3 and NOS2 was performed through real-time polymerase chain reaction (RT-PCR). The statistical analysis was performed using the Student t-test, and values of p<0.05 were considered statistically significant.
The serum levels of malondialdehyde were increased (p<0.0001), and the total antioxidant capacity was reduced in the PE group (p=0.034), indicating oxidative stress. In the PE group, themean arterial pressure was significantly higher (p<0.0001), but the serum levels of NO did not show a statistically significant reduction (p=0.20). The gene expression profiling of NOS3 and NOS2 revealed a down regulation in the PE group by 8.49 and 51.05 times respectively.
Oxidative stress may lead to endothelial dysfunction, which could result in increased mean arterial pressure. Nitric oxide may play a role in this mechanism, but interactions with other vasoactive /biological substances cannot be overlooked, as the gene expression of NOS3 and NOS2 has been reduced.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2021;43(12):988-993