Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2019;41(1):62-64
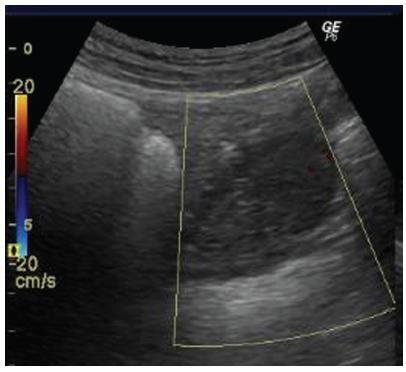
Renal artery aneurysms (RAAs) are rare and usually asymptomatic; ~ 90% of them are unilateral. Once diagnosed during pregnancy, they may rupture, presenting a high maternal-fetal risk. The present study reports the case of a 32-year-old pregnant woman with a 30-week gestational age and a ruptured unilateral RAA.

Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2019;41(1):59-61
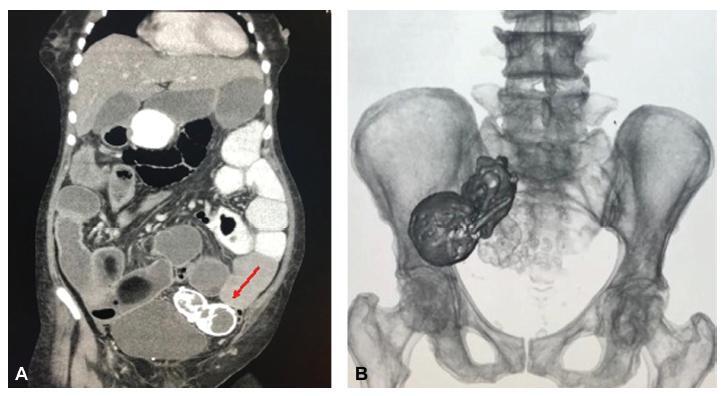
Lithopedion (lithos = rock and paidion = child) is a rare condition that only occurs in 1.5 to 1.8% of extrauterine pregnancies and in 0.00045% of all pregnancies. It consists of an ectopic pregnancy in which the fetus dies but cannot be reabsorbed by the mother’s body, which then coats it in a calcium-rich substance.We present the case of a 77-year-old woman with an incidental diagnosis of a lithopedion, which had been retained in her left pelvis for presumably 40 years.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2018;40(11):726-730
Recurrent adnexal torsion is a rare gynecological emergency. We report a case of recurrent ipsilateral adnexal torsion in a woman with polycystic ovaries, previously submitted to a laparoscopic plication of the utero-ovarian ligament. Due to the recurrence after the plication of the utero-ovarian ligament, the authors performed a laparoscopic oophoropexy to the round ligament, which is an underreported procedure. The patient was asymptomatic for 1 year, after which she had a new recurrence and needed a unilateral laparoscopic adnexectomy. Since then, she regained the quality of life without any gynecological symptoms.
Oophoropexy to the round ligament may be considered when other techniques fail or, perhaps, as a first option in selected cases of adnexal torsion, as it may allow the prevention of recurrence without increasing morbidity while preserving the adnexa.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2018;40(11):722-725
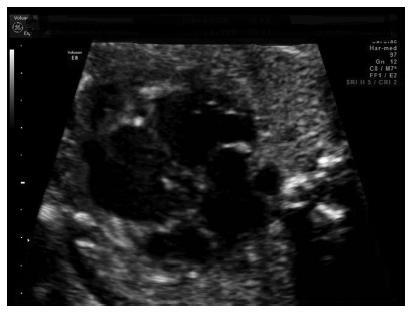
Noncompaction cardiomyopathy (NCCM) and left ventricular noncompaction (LVNC), in their isolated form, are rare cardiomyopathies. They are characterized by a thickened myocardium due to the presence of deep trabeculae recesses, and to thick trabeculae. This condition is associated with a variable clinical phenotype including heart failure, thromboembolism, and sudden death. We report a case of LVNC at 26 weeks and 4 days of gestation revised on the basis of what is currently reported in the literature. A review of the literature was performed to better describe this rare condition. Left ventricular noncompaction is a rare fetal condition and it should be suspected in case of cardiomyopathy.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2018;40(9):570-575
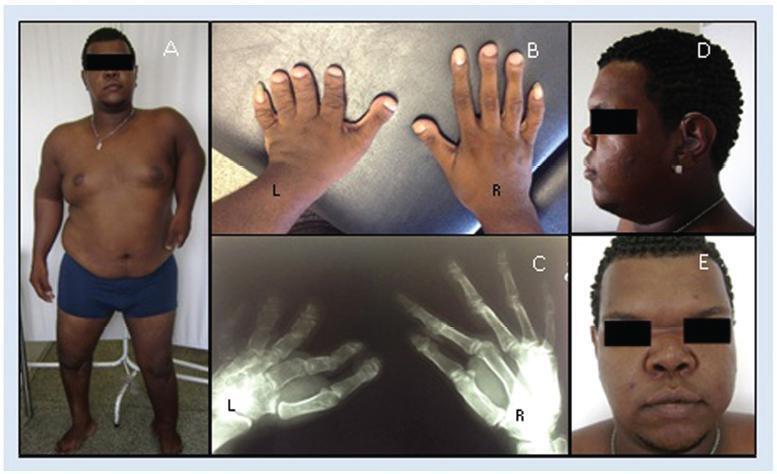
Atelosteogenesis type I (AOI) is an autosomal dominant skeletal dysplasia caused by mutations in the filamin B (FLNB) gene with classic and well-recognizable clinical findings. However, parents affected with a mild phenotype, probably with somatic mosaicism, can generate offspring with a much more severe phenotype of AOI. In the present report, we describe a female newborn with classic AOI leading to early neonatal death, whose diagnostic was based on prenatal radiological findings and on the physical examination of the father. Since her father had limb deformities and corporal asymmetry, suggesting somatic mosaicism, his biological samples were analyzed through a gene panel for skeletal dysplasias. A missense mutation not previously described in the literature was detected in the FLNB gene, affecting ~ 20% of the evaluated cells and, therefore, confirming the diagnosis ofmosaic AOI in the father. The molecular analysis of the father was crucial to suggest the diagnosis of AOI in the newborn, since she died early and there were no biological samples available.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2018;40(9):563-569
To describe a case of vesicouterine fistula and to review the literature related to this condition.
For the review, we accessed the MEDLINE, BIREME and LILACS databases; the references of the searched articles were also reviewed.
A 38-year-old woman, in the 1st day after her 3rd cesarean, presented heavy hematuria, which was considered secondary to a difficult dissection of the bladder. A total of 6 months after delivery, she failed to resume her regular menstrual cycles and presented cyclic menouria and amenorrhea. At this time, she had two episodes of urethral obstruction by blood clots. She remained without a correct diagnosis until about two years postdelivery, when a vesicouterine fistula was confirmed through cystoscopy. A surgical correction through open abdominal route, coupled with hysterectomy, was performed. After the surgery, the symptoms disappeared. The review showed a tendency of change in the relative frequency of the different types of genitourinary fistulae. Vesicovaginal fistulae, usually caused by inadequate care during labor, are becoming less frequent than those secondary tomedical procedures, such as vesicouterine fistulae. The most common cause of this latter kind of fistula is cesarean section, especially repeated cesarean sections. The diagnosis is confirmed through one or more imaging exams, or through cystoscopy. The most common treatment is surgical, and the routes are: open abdominal, laparoscopic, vaginal or robotic. There are some reports of success with the conservative treatment.
Vesicouterine fistulae are becoming more common because of the increase in the performance of cesarean sections, and the condition must be considered a possible complication thereof.

Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2016;38(4):201-206
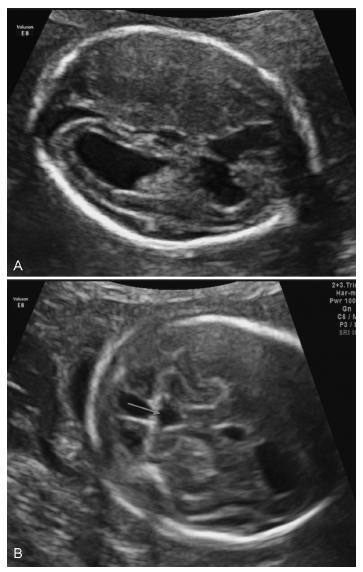
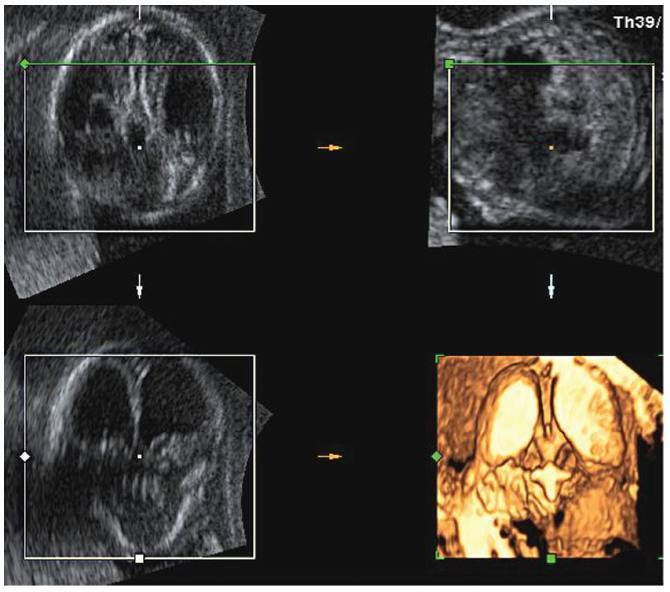
Lissencephaly is a genetic heterogeneous autosomal recessive disorder characterized by the classical triad: brain malformations, eye anomalies, and congenital muscular dystrophy. Prenatal diagnosis is feasible by demonstrating abnormal development of sulci and gyri. Magnetic resonance imaging (MRI) may enhance detection of developmental cortical disorders as well as ocular anomalies. We describe a case of early diagnosis of lissencephaly type 2 detected at the time of routine second trimester scan by three-dimensional ultrasound and fetal MRI. Gross pathology confirmed the accuracy of the prenatal diagnosis while histology showed the typical feature of cobblestone cortex. As the disease is associated with poor perinatal prognosis, early and accurate prenatal diagnosis is important for genetic counseling and antenatal care.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2016;38(4):196-200
Cytomegalovirus (CMV) is the most common congenital viral infection, causing hearing, visual and psychomotor impairment. Preexisting maternal CMV immunity substantially reduces, but not eliminates, the risk of fetal infection and affectation. This article is about a case of nonprimary maternal CMV infection during pregnancy, with vertical transmission, resulting in severe fetal affectation. Preconceptional analysis indicated maternal CMV past infection. Pregnancy progressed uneventfully until the 20th week ultrasound (US), which revealed cerebral abnormalities: thin and hyperechogenic cerebral cortex with prominent lateral ventricles, bilateral periventricular hyperechogenicities, cerebellar vermis hypoplasia and absent corpus callosum. The MRI suggested these findings were compatible with congenital infection rather than primary brain malformation.
The fetal karyotype was normal. The title of CMV's IgG antibodies almost tripled. Since the first semester,analysisof the polymerasechainreaction(PCR)forCMVDNAintheamniotic fluid was negative. The pregnancy was terminatedat 23weeks. Neuropathologicalfindings at autopsy showed severe brain lesions associated with CMV infection.