Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2019;41(7):463-466
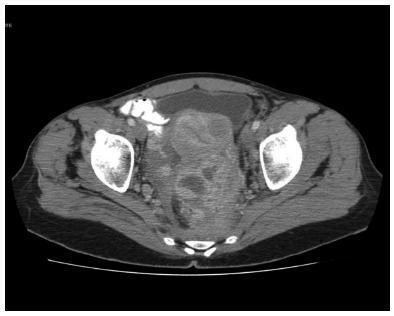
Asymptomatic female genital tract colonization with Actinomyces spp is not uncommon, particularly among intrauterine device users. Pelvic actinomycosis is an extremely rare disease. The clinical picture can resemble an advanced ovarian malignancy. We report a case of pelvic actinomycosis mimicking ovarian malignancy diagnosed postoperatively. Preoperative diagnosis is possible if there is a high index of suspicion, obviating extensive surgery and preserving fertility, since long term antibiotic treatment can be completely effective. Pelvic actinomycosis should be included in the differential diagnosis of women presenting a pelvic mass, especially if there is intrauterine device use history.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2019;41(6):412-416
Extramammary Paget disease is a rare neoplastic condition that more commonly affects postmenopausal Caucasian women. Although the vulvar area is the most frequently affected location, it corresponds solely to 1 to 2% of all vulvar malignancies. A 72-year-old female patient was observed in our outpatient clinic with a 2-year history of an erythematous and pruritic plaque on the vulva. Histopathology and immunohistochemistry studies were compatible with extramammary Paget disease of the vulva. Associated neoplastic conditions were excluded. Due to multiple relapses, the patient was submitted to three surgical interventions, including a total vulvectomy, and to external radiotherapy. The present case illustrates the chronic and recurrent nature of extramammary Paget disease despite aggressive procedures as well as the challenge in obtaining tumor-free resection margins.

Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2019;41(6):409-411
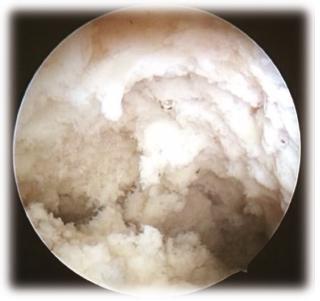
Endometrial tuberculosis is a rare diagnosis in the postmenopausal period, and it can mimic a carcinoma. The present article describes the case of a 54-year-old female patient with weight loss, abdominal pain, and ascites. An ultrasonography showed endometrial thickening, and a video hysteroscopy revealed a uterine cavity with formations with cotton aspect covering the entire endometrial surface and the tubal ostia. An anatomopathological evaluation diagnosed endometrial tuberculosis. The treatment was with a standardized therapeutic scheme (ethambutol, isoniazid, pyrazinamide and rifampicin), and the patient evolved with clinical improvement and normal uterine cavity at hysteroscopy. Considering the lack of pathognomonic hysteroscopic findings of the disorder, it is important to disclose the images of the case.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2019;41(5):352-356
Pentalogy of Cantrell (PC) is a rare congenital anomaly characterized by changes in the mesodermal median structures and congenital heart disease, often with a poor prognosis. In 1958, Cantrell et al2 defined the full spectrum of the syndrome with the following anomalies: defects of the anterior diaphragm, of the lower part of the sternum, of the supraumbilical region and the abdominal wall, of the diaphragmatic pericardium, and various intracardiac congenital abnormalities. The present report describes a case of ectopia cordis associated with PC and the importance of the participation of a multidisciplinary team in the treatment of this condition.

Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2019;41(5):348-351
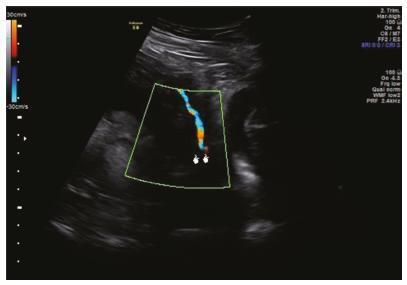
Vasa previa (VP) is a dangerous obstetric condition associated with perinatal mortality and morbidity. In vitro fertilization (IVF) is a risk factor for VP due to the high incidence of abnormal placentation. The diagnosis should be made prenatally, because fetal mortality can be extremely high. We report two cases to demonstrate the accuracy of transvaginal ultrasound in the prenatal diagnosis of VP. A 40-year-old primiparous Caucasian woman with IVF pregnancy was diagnosed with VP at 29 weeks of gestation and was hospitalized for observation at 31 weeks of gestation. She delivered a male newborn weighing 2,380 g, with an Apgar score of 10 at 5 minutes, by elective cesarean section at 34 weeks + 4 days of gestation, without complications. A 36-yearold primiparous Caucasian woman with IVF pregnancy was diagnosed with placenta previa, bilobed placenta increta and VP. The cord insertion was velamentous. She was hospitalized for observation at 26 weeks of gestation. She delivered a female newborn weighing 2,140 g, with an Apgar score of 9 at 5 minutes, by emergency cesarean section at 33 weeks + 4 days of gestation due to vaginal bleeding. The prenatal diagnosis of VP was associated with a favorable outcome in the two cases, supporting previous observations that IVF is a risk factor for VP and that all IVF pregnancies should be screened by transvaginal ultrasound.
Summary
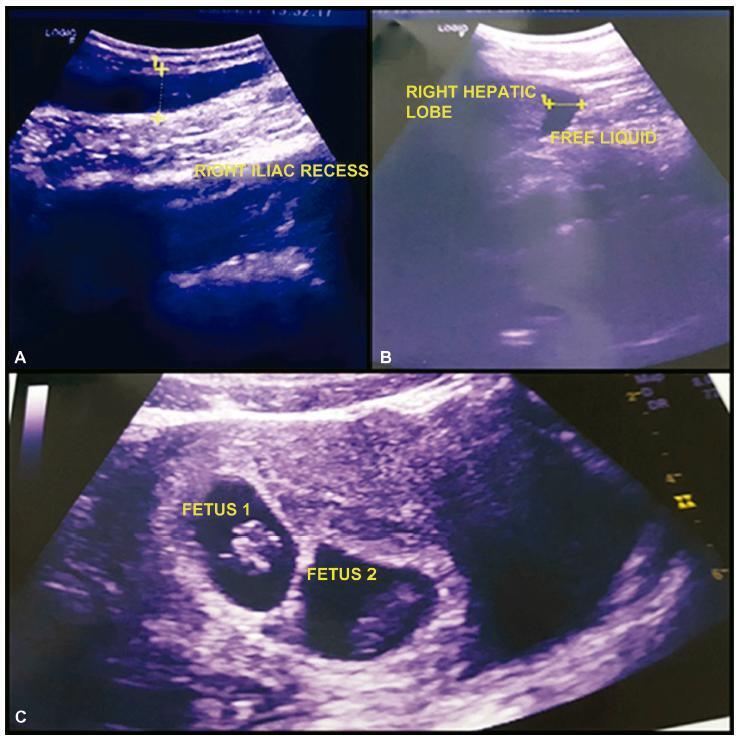
Revista Brasileira de Ginecologia e Obstetrícia. 2019;41(4):268-272
Heterotopic pregnancy (HP) is defined as the simultaneous development of an intra- and an extra uterine gestation. The occurrence of a spontaneous triplet HP is an exceptionally rare medical condition. We report the case of a young woman with spontaneous heterotopic triplets at 8weeks of gestation, with amisdiagnosis of topic twins and acute appendicitis. The ectopic tubal pregnancy was ruptured and a salpingectomy was performed by laparotomy. The intrauterine pregnancy progressed uneventfully. The two healthy babies were delivery by cesarean section at 36 ± 2 weeks of gestation. Heterotopic triplets with ruptured tubal ectopic pregnancy represent a special diagnostic and therapeutic challenge for the obstetrician. A high rate of clinical suspicion and timely treatment by laparotomy or laparoscopy can preserve the intrauterine gestation with a successful outcome of the pregnancy.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2019;41(3):203-205
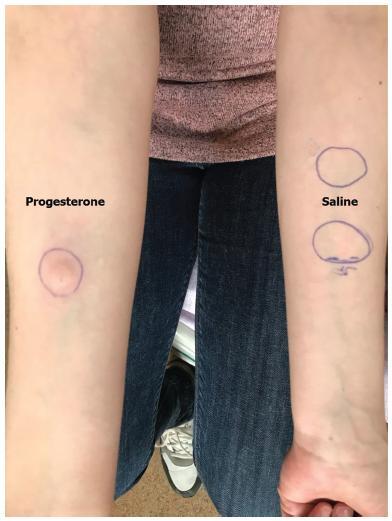
Autoimmune progesterone dermatitis (APD) is a rare autoimmune dermatosis characterized by recurrent cutaneous and mucosal lesions during the luteal phase of the menstrual cycle that disappear some days after the menses.
Report A 34-year-old primipara woman with no significant past medical history and no prior exogenous hormone use, who presented with cyclic skin eruptions starting 1 year after the delivery. The lesions occurred 6 days before the menses and disappeared in between 1 and 2 days after the menstruation ceased. The patient was diagnosed after a positive response to an intradermal test with progesterone and was successfully treated with combined oral contraceptives. The skin eruptions have not returned since the initiation of this therapy.
Dermatologists, gynecologists, and obstetricians should be aware of this rare entity. Furthermore, if this condition is suspected, a thorough history taking on the menstrual cycle and results of the intradermal progesterone test are mandatory.