Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2014;36(12):541-547
DOI 10.1590/So100-720320140005051
To identify the profile of use of medication during the first trimester of pregnancy with emphasis on safety assessment and on the adoption of folic acid and ferrous sulfate by pregnant women attended at a Basic Health Unit in Brazil.
This was a cross-sectional study nested in a cohort of pregnant women. Medications were classified according to the Anatomical Therapeutic Chemical (ATC), and their safety was evaluated according to the Food and Drug Administration (FDA) and the Brazilian Health Surveillance Agency (ANVISA). The adoption of ferrous sulfate and folic acid was investigated according to the protocol set forth by the Brazilian Ministry of Health.
The survey included 212 pregnant women, 46.7% of whom were taking medications at the time of pregnancy diagnosis, and 97.6% used medication during the first trimester after diagnosis. The highest percentage of self-medication occurred before the beginning of prenatal care (64.9%). According to the FDA criteria, there was a high level of exposure to D and X risk drugs before the beginning of prenatal care (23.0%), which was also observed for drugs not recommended by ANVISA (36.5%). Of the surveyed sample, 32.5% did not follow the protocol of the Brazilian Ministry of Health. In all, 67.9% of pregnant women had inadequate drug exposure. There was a difference between the proportions of drugs used according to the ATC, and the main anatomical groups identified were the drugs that act on blood and blood-forming organs, and anti-infective medications for systemic use. When pregnancy was diagnosed, the use of a large number of medications that act on the genitourinary system and sex hormones (16.2%) was identified, such as oral contraceptives, a fact probably related to the percentage of unplanned pregnancies (67.0%), on the same occasion 4 pregnant women used folic acid and 3 used ferrous sulphate.
The present results show that a large number of medications are used during pregnancy. Even if there was little exposure to drugs at the time of diagnosis, there is an overuse of potentially risky medications and self-medication during the first trimester of pregnancy.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2014;36(12):535-540
DOI 10.1590/So100-720320140005086
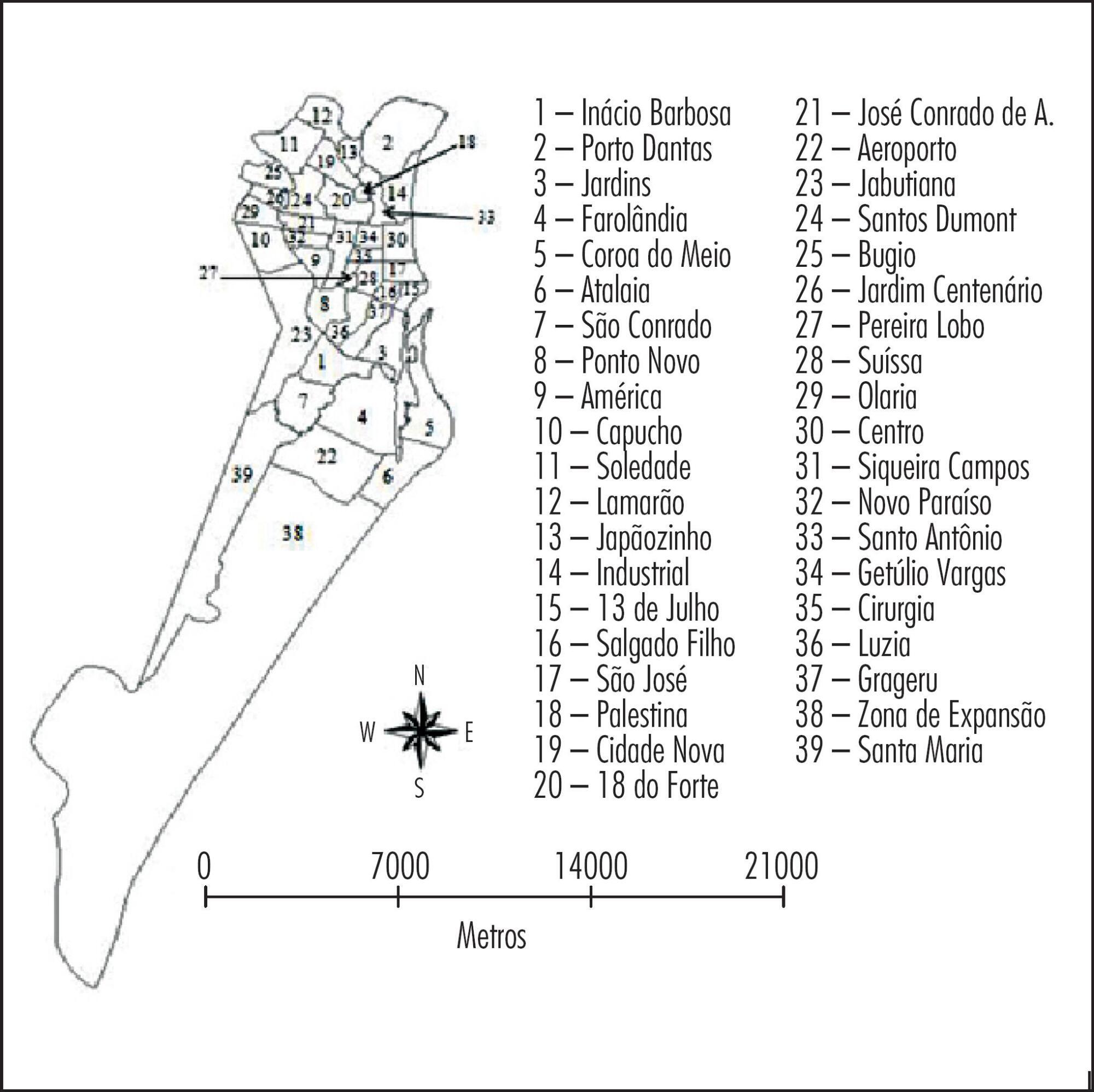
To analyze the spatial distribution of the prevalence of anti-toxoplasma gondii antibodies in pregnant women from a Brazilian Northeast city, and to correlate such prevalence with average maternal age and place of residence.
A descriptive, analytical and ecological study was conducted from January 1st to December 31st 2012. Data were obtained retrospectively from the Medical Specialties Center database and processed with the Epi info statistical package (Epi 7, Centers for Disease Control and Prevention, Atlanta, USA) and with Microsoft Excel 2010. The X2 test was applied to assess the association between the prevalence of antibodies to toxoplasma gondii and the average age. Spatial analysis of infection prevalence was performed using the TerraView software, version 4.2.2, with Kerneldensity estimation, which estimates the quantity of events through maps in order to identify areas with the highest concentration of cases in the city.
The seroprevalence of IgG was 68.5% (95%CI 67.2-69.8) and the prevalence of IgM was 0.36% (95%CI 0.23-0.6). A higher IgG prevalence was associated with increased age in the oldest neighborhoods of the state capital, whereas a higher IgG prevalence among younger women was detected in suburban neighborhoods. The spatial concentration of IgM antibodies was higher in suburban neighborhoods, with no significant correlation between seroprevalence and age.
Geoprocessing allowed the identification of areas with the highest prevalence, as well as the most susceptible average age and it was also useful as an instrument for the evaluation and implementation of appropriate preventive measures for this municipality and for other regions of Brazil.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2014;36(12):575-580
DOI 10.1590/SO100-720320140005158
To compare the distributions of patients with clinical-pathological subtypes of luminal B-like breast cancer according to the 2011 and 2013 St. Gallen International Breast Cancer Conference Expert Panel.
We studied 142 women with breast cancer who were positive to estrogen receptor and had been treated in São Paulo state, southeast Brazil. The expression of the following receptors was assessed by immunohistochemistry: estrogen, progesterone (PR) and Ki-67. The expression of HER-2 was measured by fluorescent in situ hybridization analysis in tissue microarray.
There were 29 cases of luminal A breast cancers according to the 2011 St. Gallen International Breast Cancer Conference Expert Panel that were classified as luminal B-like in the 2013 version. Among the 65 luminal B-like breast cancer cases, 29 (45%) were previous luminal A tumors, 15 cases (20%) had a Ki-67 >14% and were at least 20% PR positive and 21 cases (35%) had Ki-67 >14% and more than 20% were PR positive.
The 2013 St. Gallen consensus updated the definition of intrinsic molecular subtypes and increased the number of patients classified as having luminal B-like breast cancer in our series, for whom the use of cytotoxic drugs will probably be proposed with additional treatment cost.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2014;36(12):569-574
DOI 10.1590/SO100-720320140005068
The aim of this study was to evaluate the clinical features and prognostic implications of patients with recurrent cervical cancer.
By reviewing the medical records we evaluated all patients with cervical cancer at stages IA to IVA who started treatment at a specialized hospital in the Southeast region of Brazil from 2007 to 2009. Recurrence episodes were categorized according to location of disease and information was collected regarding the type of treatment and survival of these patients. The sample was characterized by descriptive statistics and association analyses were performed using Fisher's exact test.
Fifty cases of recurrence were identified among 469 selected records, with 31 patients being symptomatic at diagnosis of recurrence (62%); and 19 being asymptomatic (38%). Among women with symptoms, eight requested anticipation of the previously scheduled appointment because of the presence of clinical complaints. Patients with symptoms at the diagnosis of recurrence had lower rates of overall two-year survival (39.4 versus 67.6%) (p=0.081). None of the patients with recurrence at distance received curative intent treatment, but all received surgical treatment or radiotherapy aiming at full remission of the disease. Women who requested anticipation of the appointment because of the presence of symptoms had a significant reduction of overall two-year survival after recurrence (0 versus 60.4%; p<0.001) compared to those who attended the consultation on the scheduled date, and none of them received curative intent treatment. As expected, the patients who underwent palliative treatment with the main objective of improving quality of life and increasing survival but with no perspective of cure had a significant reduction in overall survival compared to those who were treated with curative intent (76.7 versus 35.4%; p<0.001).
The benefit of detecting asymptomatic recurrence of cervical cancer has the potential to improve the prognosis of patients with local and regional recurrence, but studies on larger series are necessary to confirm this possibility.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2014;36(11):519-524
DOI 10.1590/S0100-720320140005100
To validate a questionnaire to be applied in order to learn and describe the perceptions of specialists in obstetrics and gynecology about their experience and self-confidence in the emergency care for vaginal delivery.
This was a prospective study for the validation of an instrument that contains statements about emergency obstetrical care: breech delivery (n=23), shoulder dystocia (n=20), postpartum haemorrhage (n=24), forceps delivery (n=32), and vacuum extractor (n=5). Participants gave their opinions on each item by applying the Likert scale (0=strongly disagree, 1=partially disagree, 2=indifferent, 3=partially agree and 4=strongly agree). The questionnaire was applied to 12 specialists in obstetrics and gynecology and it was expected to be found a level of comprehension exceeding 80%. A five-point scale was used to assess the understanding of each question (from 0=did not understand anything to 5=understood perfectly and I have no doubt). A score above 4 was considered to indicate sufficient understanding. The instrument used was specially designed to suit the specific demands. The analysis of internal reliability was done using the Cronbach alpha coefficient. For external validation, we calculated the proportion of items with full understanding for each subscale. For research purposes, the alpha should be greater than 0.7.
Participants had a mean age of 33.3 years, with 5.0 standard deviation (SD), and an average interval time since graduation from medical school of 5.8 years (SD=1.3 years). All were specialists with residency in obstetrics and gynecology. The mean proportion of participants who fully understood the items in each emergency was 97.3% for breech delivery, 96.7% for shoulder dystocia, 99.7% for postpartum hemorrhage, 97.4% for forceps delivery, and 98.3% for the use of a vacuum extractor. The results of Cronbach's alpha for the items in each emergency studied were: 0.85 for breech delivery, with 0.72 lower limit of 95% confidence interval ((%%CI), 0.74 for shoulder dystocia (lower limit of 95%CI=0.51), 0.79 for postpartum hemorrhage (lower limit of 95%CI=0.61), 0.96 for forceps delivery (lower limit of 95%CI=0.92), and 0.90 for the vacuum extractor (lower limit of 95%CI=0.79).
The validated questionnaire is useful for learning and describing the perception of physicians about their experience and self-confidence in emergency care for vaginal births.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2014;36(11):514-518
DOI 10.1590/S0100-720320140005007
To describe the epidemiologic and obstetric characteristics of women with recurrent miscarriages.
A descriptive and analytical study whose inclusion criterion was every woman that was attended at the clinic for recurrent miscarriage (loss group), between January 2006 and December 2010. Patients that did not live in Salvador, Bahia, Brazil, and those who were not reached by telephone or whose number was not included in the medical record were not included. The Control Group consisted of 204 pregnant women seen at the low-risk prenatal care unit between May 2007 and April 2008. Women who did not accept to be interviewed and those with obstetric risk were excluded from the Control Group. The analyzed variables were: age, education, occupation, marital status, alcohol consumption, body mass index, obstetric history and the gestational age when the losses occurred. The SPSS 18.0 program was used for statistical analysis. Means and standard deviations of continuous variables were compared using the Student's t-test and the frequencies of the nominal variables were compared by the χ2 test.
The mean age of women in the loss group was higher than in the Control Group (32.3±6.3 versus 26.5±6.4 years old, p<0.01). Consumption of alcoholic beverages predominated in the loss group (36.9 versus 22.1%, p=0.01), as well as marital status (93.2 versus 66.7% were married or living in a stable union, p<0.01). The pre-pregnancy body mass index was higher in the loss group (26.9 versus 23.5%, p<0.01). Regarding obstetric history, 103 women with recurrent miscarriage reported 334 pregnancies. Fifty-six of them had 2 or more miscarriages in the first quarter and in 31 of them, 2 or more pregnancies progressed to late abortions/extremely preterm infants.
Some risk factors were identified in women with recurrent losses, such as more advanced age and higher body mass index. These observations agree with more recent proposals regarding recurrent losses that consider the inclusion of losses in various gestational ages.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2014;36(11):509-513
DOI 10.1590/S0100-720320140005024
To evaluate the influence of maternal obesity on pregnancy, childbirth, and neonatal outcomes.
A cross-sectional study with 298 postpartum women. Information was obtained through interviews and access to patients' medical records. The patients were divided into three groups according to their pre-gestational body mass index: normal weight (18.5–24.9 kg/m2), overweight (25.0–29.9 kg/m2), and obese (≥30.0 kg/m2). Data are reported as adjusted odds ratios with 95% confidence interval (95%CI) following multinomial logistic regression analysis to account for confounding variables.
Compared to pregnant women with normal body mass index, overweight women had greater chances of having cesarean delivery, odds ratio (OR) of 2.2 and 95%CI 1.3–3.9, and obese women even more (OR=4.2; 95%CI 2.1–8.1). The chances of gestational diabetes increased in the Overweight (OR=2.5; 95%CI 1.1–5.6) and Obese groups (OR=11.1; 95%CI 5.0–24.6). The occurrence of hypertensive syndrome was also higher in overweight (OR=3.2; 95%CI 1.2–8.1) and obese pregnant women (OR=7.5; 95%CI 2.9–19.1). Major postpartum hemorrhage only showed greater values in the obese women group (OR=4.1; 95%CI 1.1–15.8). Regarding the newborns, the probability of a low Apgar score at first minute was higher in the Obese Group (OR=5.5; 95%CI 1.2–23.7) and chances of macrosomia were higher in the Overweight Group (OR=2.9; 95%CI 1.3–6.3). Data regarding neonatal hypoglycemia were not conclusive.
Excessive weight (overweight and obesity) during pregnancy increases the chance of maternal complications (gestational diabetes, hypertensive syndrome, and major postpartum hemorrhage) and neonatal outcomes (cesarean delivery, macrosomia, and low Apgar score).