Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2024;46:e-rbgo35
We aimed to translate and determine cultural validity of the Vaginal Changes Sexual and Body Esteem Scale (VSBE) for Brazilian Portuguese language in postpartum women who underwent vaginal delivery with or without perineal laceration and cesarean section.
A cross-sectional study conducted virtually, with online data collection through a survey with 234 postpartum women of 975 that were invited. Clinical, sociodemographic, and psychometric variables from the VSBE questionnaire were analyzed (content validity index, internal consistency, test-retest reliability, construct/structural and discriminant validity). Multivariate analysis was performed to explore associated factors with the presence of perineal laceration.
One-hundred fifty-eight women experienced vaginal delivery, of which 24.79% had an intact perineum, 33.33% had perineal laceration, and 9.4% underwent episiotomy; and 76 participants had cesarean sections. Women with perineal laceration were older, presented dyspareunia and previous surgeries than women without perineal laceration (p<0.05). For VSBE, a high internal consistency (Cronbach's α > 0.7) was observed, but it did not correlate with Body Attractiveness Questionnaire and Female Sexual Function Index; however, it correlated with the presence of women sutured for perineal laceration. Moreover, VSBE presented good structural validity with two loading factors after exploratory factor analysis. VSBE also demonstrated discriminant validity between the presence or absence of perineal laceration. The presence of urinary incontinence (UI) (OR=2.716[1.015-4.667];p=0.046) and a higher VSBE total score (OR=1.056[1.037-1.075];p<0.001) were the only factors associated with perineal laceration.
Vaginal Changes Sexual and Body Esteem Scale demonstrated appropriate translation and good internal consistency, discriminant/construct validity and reliability. Vaginal Changes Sexual and Body Esteem Scale total score and presence of UI were associated with women that underwent perineal laceration.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2021;43(6):436-441
The aim of the present study was to evaluate the risk factors for cesarean section (C-section) in low-risk multiparous women with a history of vaginal birth.
The present retrospective study included low-risk multiparous women with a history of vaginal birth who gave birth at between 37 and 42 gestational weeks. The subjects were divided into 2 groups according to the mode of delivery, as C-section Group and vaginal delivery Group. Risk factors for C-section such as demographic characteristics, ultrasonographic measurements, smoking, weight gain during pregnancy (WGDP), interval time between prior birth, history of macrosomic birth, and cervical dilatation at the admission to the hospital were obtained fromthe charts of the patients. Obstetric and neonatal outcomes were compared between groups.
The most common C-section indications were fetal distress and macrosomia (33.9% [n=77 and 20.7% [n=47] respectively). A bivariate correlation analysis demonstrated that mothers aged>30 years old (odds ratio [OR]: 2.09; 95% confidence interval [CI]: 1.30-3.34; p=0.002), parity >1 (OR: 1.81; 95%CI: 1.18-2.71; p=0.006), fetal abdominal circumference (FAC) measurement>360mm (OR: 34.20; 95%CI: 8.04 -145.56; p<0.001)) and<345mm (OR: 3.06; 95%CI: 1.88-5; p<0.001), presence of large for gestational age (LGA) fetus (OR: 5.09; 95%CI: 1.35-19.21; p=0.016), premature rupture of membranes (PROM) (OR: 1.52; 95%CI: 1-2.33; p=0.041), and cervical dilatation<5cm at admission (OR: 2.12; 95%CI: 1.34-3.34; p=0.001) were associated with the group requiring a C-section.
This is the first study evaluating the risk factors for C-section in low-risk multiparous women with a history of vaginal birth according to the Robson classification 3 and 4. Fetal distress and suspected fetal macrosomia constituted most of the Csection indications.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2020;42(11):712-716
To determine whether there was any difference in neonatal and maternal outcomes between breech vaginal delivery and cephalic vaginal delivery.
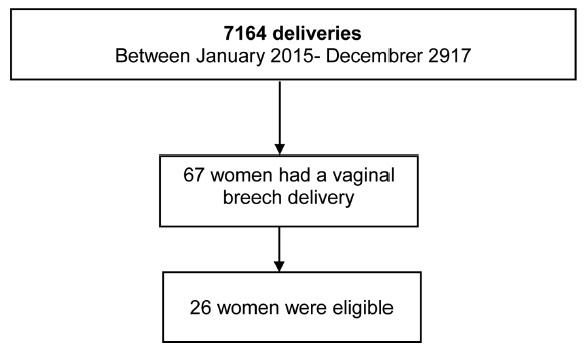
A retrospective, case-control study was conducted between January 2015 and December 2017 in a Portuguese hospital. A total of 26 cases of breech vaginal delivery were considered eligible and 52 pregnant women formed the control group.
Induced labor was more frequent in the breech vaginal delivery group (46% versus 21%, p = 0.022). Episiotomy was more common in the breech vaginal delivery group (80% versus 52%, p = 0.014), and one woman had a 3rd degree perineal laceration. Newborns in the study group had a lower birthweight (2,805 g versus 3,177 g, p < 0.001). There was no significant difference in the neonatal outcomes.
The present study showed that breech vaginal delivery at term compared with cephalic presentation was not associated with significant differences in neonatal and maternal morbidity. It also suggests that breech vaginal delivery remains a safe option under strict selection criteria and in the presence of an experienced obstetrician.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2020;42(4):181-187
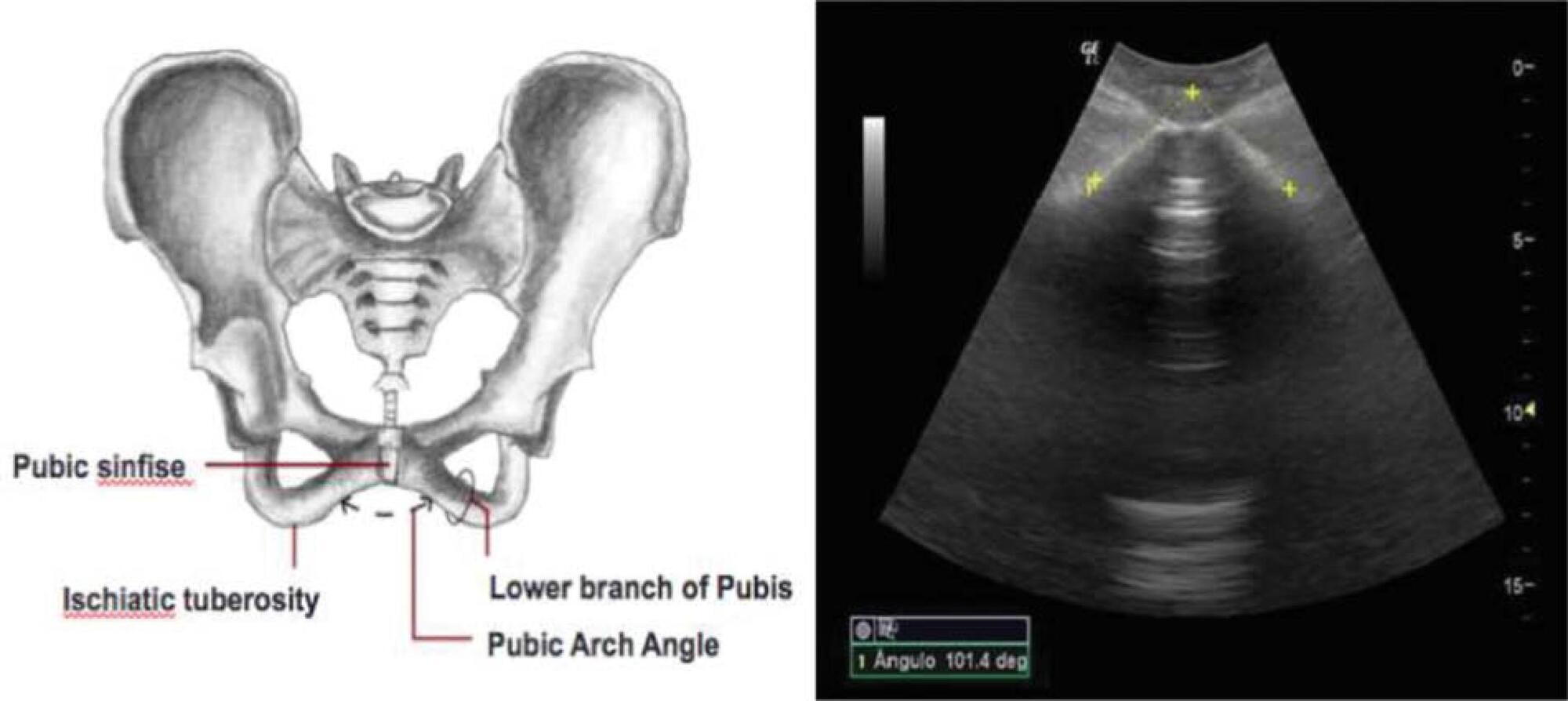
To evaluate the ability of the pubic arch angle (PAA) as measured by transperineal ultrasonography during labor to predict the delivery type and cephalic pole disengagement mode.
The present prospective cross-sectional study included 221 women in singleton-gestational labor ≥ 37 weeks with cephalic fetuses who underwent PAA measurement using transperineal ultrasonography. These measurements were correlated with the delivery type, cephalic pole disengagement mode, and fetal and maternal characteristics.
Out of the subjects, 153 (69.2%) had spontaneous vaginal delivery, 7 (3.2%) gave birth by forceps, and 61 (27.6%) delivered by cesarean section. For the analysis, deliveries were divided into two groups: vaginal and surgical (forceps and cesarean). The mean PAA was 102 ± 7.5º (range, 79.3-117.7º). No statistically significant difference was observed in delivery type (102.6 ± 7.2º versus 100.8 ± 7.9º, p = 0.105). The occipitoanterior position was seen in 94.1% of the fetuses and the occipitoposterior position in 5.8%. A narrower PAA was found in the group of surgical deliveries (97.9 ± 9.6º versus 102.6 ± 7.3º, p = 0.049). Multivariate regression analysis showed that PAA was a predictive variable for the occurrence of head disengagement in occipital varieties after birth (odds ratio, 0.9; 95% confidence interval, 0.82-0.99; p = 0.026).
Ultrasonographic measurement of the PAA was not a predictor of delivery type, but was associated with the persistence of occipital varieties after birth.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2018;40(1):04-10
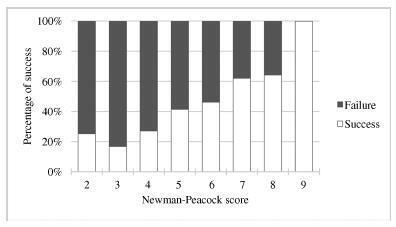
External cephalic version (ECV) is a maneuver that enables the rotation of the non-cephalic fetus to a cephalic presentation. The Newman-Peacock (NP) index, which was proposed by Newman et al. in a study published in 1993, was described as a prediction tool of the success of this procedure; it was validated in a North-American population, and three prognostic groups were identified.
To evaluate the value of the NP score for the prediction of a successful ECV in a Portuguese obstetrical population, and to evaluate maternal and fetal safety.
We present an observational study conducted from 1997-2016 with pregnant women at 36-38 weeks of pregnancy who were candidates for external cephalic version in our department. Demographic and obstetrical data were collected, including the parameters included in the NP index (parity, cervical dilatation, estimated fetal weight, placental location and fetal station). The calculation of the NP score was performed, and the percentages of success were compared among the three prognostic groups and with the original study by Newman et al. The performance of the score was determined using the Student t-test, the Chi-squared test, and a receiver operating characteristic (ROC) curve.
In total, 337 women were included. The overall success rate was of 43.6%. The univariate analysis revealed that multiparity, posterior placentation and a less engaged fetus were factors that favored a successful maneuver (p < 0.05). Moreover, a higher amniotic fluid index was also a relevant predictive factor (p < 0.05). The Newman-Peacock score had a poorer performance in our population compared with that of the sample of the original study, but we still found a positive relationship between higher scores and higher prediction of success (p < 0.001). No fetal or maternal morbidities were registered.
The Newman-Peacock score had a poorer performance among our population compared to its performance in the original study, but the results suggest that this score is still a useful tool to guide our clinical practice and counsel the candidate regarding ECV.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 1998;20(6):342-349
DOI 10.1590/S0100-72031998000600007
Objectives: to determine prognostic factors for vaginal delivery in pregnant women after previous cesarean section admitted to CAM-IMIP in labor.Patients and Methods: a case-control study was performed, analyzing all deliveries of patients with previous cesarean section admitted to CAM-IMIP between January 1991 and December 1994. Patients who had a cesarean section (n=156) were considered cases while patients with a vaginal birth were the controls (n=338). Inclusion criteria were: gestational age > 36 weeks, previous cesarean section at least 1 year before, alive fetus, spontaneous labor and vertex presentation. Patients with high-risk pregnancies, acute fetal distress and a previous vaginal delivery after cesarean section were excluded. Statistical analysis was performed with in Epi-Info 6.0 and Epi-Soft, using c² test, Fisher's exact test and Student's "t" test. Odds ratio and its 95% confidence interval was calculated and multiple logistic regression analysis was performed for the control of confounding factors. Results: overall rate of cesarean section was 31.6%. Maternal factors significantly associated with vaginal delivery were age < 20 years (OR = 2.07, 95% CI = 1.18-3.66) or > 35 years (OR = 0.54, 95% CI = 0.36-0.82), history of vaginal delivery (OR = 1.6, 95% CI = 1.01-2.55) and complications of pregnancy as indication for previous cesarean section (OR = 3.67, 95% CI =1.19-12.02). A significant association with vaginal delivery could not be detected for other variables: interval between previous cesarean section and present delivery, other indications for cesarean section and type of uterine suture. In a multiple logistic regression model the variables that remained associated with vaginal delivery were maternal age and previous vaginal delivery. Conclusions: maternal age below 20 years, previous cesarean section indicated due to gestational complications and previous vaginal delivery were favorably associated with vaginal delivery in patients with prior cesarean section. Risk of repeated cesarean section is increased in pregnant women aged 35 years or above. These factors should be contemplated when obstetrical evaluation of the delivery route is performed.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2004;26(10):781-786
DOI 10.1590/S0100-72032004001000005
PURPOSE: to assess the obstetric and perinatal outcomes in cases of term newborns in breech presentation, in patients with previous vaginal deliveries, comparing them to term newborns in vertex presentation. METHODS: 8,350 deliveries retrospectively from March 1998 to July 2003 were analysed. Of 419 deliveries (5.1%) in breech presentation, 58 cases were selected for the study (breech group), according to the following criteria: patients who had had one or more babies through vaginal delivery, gestational age ³37 weeks, no fetal malformation, no complications in the current pregnancy, birth weight between 2,500 and 3,750 g, and no previous cesarean section. The breech group was matched to 1,327 newborns in vertex position from pregnant women with no previous cesarean section (vertex group). Maternal age, parity, gestational age, delivery way, birth weight, meconium-stained amniotic fluid, 1- and 5-min Apgar score, need of neonatal intensive care unit, and small- and big-for-gestational age newborns were analyzed. Statistical analysis was performed by the c² test and by Student's t test, with the level of significance set at p<0.05. RESULTS: when breech and vertex groups were compared, they showed significant differences regarding the following variables: birth weight (3,091±538 g vs 3,250±497 g; p<0.01), vaginal delivery (63.8 vs 95.0%; p<0.0001), cesarean section (36.2 vs 5.0%; p<0,0001), and 1-min Apgar score (p<0.0001), respectively. CONCLUSIONS: we conclude that in term fetuses in breech position from pregnant women with previous vaginal deliveries, birth weight, delivery way, and 1-min Apgar score were different compared to fetuses in vertex position from women with the same characteristics.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2004;26(1):9-13
DOI 10.1590/S0100-72032004000100002
PURPOSE: to compare maternal and neonatal outcomes between spontaneous vaginal and Simpson-Braun forceps deliveries in nulliparous women. METHOD: a retrospective study including two groups of nulliparous women, who had vaginal delivery under peridural anesthesia in the obstetric unit of the CAISM-UNICAMP: the forceps group included 119 women who had Simpson-Braun forceps delivery, and the normal group included 114 women who delivered spontaneously. Neonatal outcomes, such as Apgar score and the evolution in the first days of life, were studied. Data were compared in both groups and, for statistical analysis, c² test, Fisher exact, and Student t tests were used. The differences were considered significant when p<0.05. RESULTS: the indications for Simpson-Braun forceps delivery were maternal-fetal relief (90 cases) and abbreviation of the expulsive period (29 cases). In the forceps group there were 8 cases (6.7%) of vaginal injuries; a similar result was observed in the normal group. The number of hospitalization days for the parturient and the newborns was identical, 2.4 days. The newborns in the two groups had similar Apgar scores inferior to 7 at the first minute (7.5 vs 4.3%) and at the fifth minute (1.6 vs1.7%). The weight in the two groups had similar results (3,146 and 3,016 g). The first days of life did not differ between the groups. CONCLUSIONS: the use of Simpson-Braun forceps was safe, when compared to spontaneous vaginal delivery.