Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2021;43(3):178-184
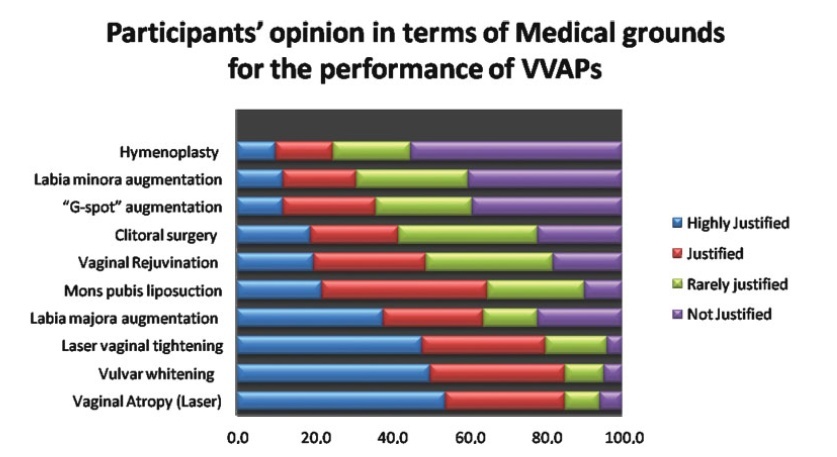
The present study aimed to explore the opinion and ethical consideration of vulvovaginal aesthetics procedures (VVAPs) among health professionals and medical students in Saudi Arabia.
This is a cross-sectional study performed between January 2020 and April 2020. Data was collected through electronic media, WhatsApp, and emails. The results were analyzed by applying the Students t-test, and correlations were considered significant if they presented a p-value<0.05.
There is significant demand to educate doctors, health professionals, medical students, and gynecologists for the VVAPs to have a solid foundation, justified indications, and knowledge about various aesthetic options. Although female doctors, medical students, young doctors, and gynecologists have more knowledge about VVAPs, all health professionals ought to be aware of recent trends in vulvovaginal aesthetics (VVA). The present analysis determined that VVA should be under the domain of gynecologists, rather than under that of plastic surgeons, general surgeons, and cosmetologists. Themajority of the participants considered that vaginal rejuvenation, “G-spot” augmentation, clitoral surgery, and hymenoplasty are not justifiable on medical grounds.
The decision to opt for different techniques for vaginal tightening and revitalization should be taken very carefully, utilizing the shared decision-making approach. Ethical aspects and moral considerations are important key factors before embarking in the VVAPs purely for cosmetic reasons. Further research is required to determine the sexual, psychological, and body image outcomes for women who underwent elective VVAPs. Moreover, medical educators must consider VVAPs as part of the undergraduate and postgraduate medical curriculum.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2014;36(11):484-488
DOI 10.1590/S0100-720320140004952
To evaluate sexual function in women undergoing assisted reproductive techniques.
This is a case-control study including 278 women assisted in Human Reproduction services and at the Gynecology Clinic of the University Hospital, Federal University of Goiás, Brazil. The women were divided into a study group (168 infertile women) and a control group (110 fertile women), and they answered the Female Sexual Function Index (FSFI) questionnaire used the assess the sexual function. We calculated the odds ratio (OR) for the chance of sexual dysfunction in infertile women (p<0.05).
Out of the analyzed women, 33.09% reported sexual dysfunction, with no difference in the FSFI score between groups (p=0.29). The prevalence of sexual dysfunction was of 36.30% among infertile women and 28.18% among fertile women; however, there was no difference between FSFI scores (p=0.36). The desire and arousal domains were significantly different among infertile women (p=0.01). Infertile women had the same chances of having sexual dysfunction as fertile women (OR=1.4, 95%CI 0.8–2.4; p=0.2).
There were no differences between infertile and fertile women. Infertile women undergoing assisted reproduction techniques require professional approach to sexual health regarding desire and arousal.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2014;36(3):107-112
DOI 10.1590/S0100-72032014000300003
To evaluate the impact of sexual and reproductive health theme insertion in the undergraduate medical curriculum at a Brazilian public university.
We developed an instrument for cognitive assessment in sexual and reproductive health based on the subjects addressed in the optional curriculum component Reproductive Health, resulting in an objective multiple choice test containing 27 items. The selected topics were: human, sexual and reproductive rights (HSRR), sexuality, institutional violence, gender, sexual violence, conception, contraception, abortion/legal interruption of pregnancy, maternal mortality and sexually transmitted infections (STIs) - HIV/AIDS. The subjects were grouped into three dimensions of knowledge: HSRR, legal/institutional and biomedical. Two multivariate models were adjusted in the analysis of covariance.
The study included 183 students, 127 of the group who took the elective curriculum course reproductive health (RH Group) and 56 who did not (Non-RH Group). Ninety-six students (52.5%) were males and 87 (47.5%) were females. Mean age was 24.7±1.9 years for the RH Group and 24.4±2.6 for the Non-RH Group. The average performance of the SR Group was higher than that of Non-RH subjects regarding the following subjects: HSRR, sexuality, institutional violence, sexual violence, abortion/legal interruption, and STDs - HIV/AIDS. There was no gender difference in performance, except for the theme maternal mortality, in which males scored worse than females (6.9±0.2 and 7.8±0.2, respectively; p<0.05).
The participation of students in the elective curriculum component Reproductive Health was associated with better performance in some dimensions of cognitive assessment, suggesting a positive impact of this initiative on general medical education.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2008;30(2):55-60
DOI 10.1590/S0100-72032008000200002
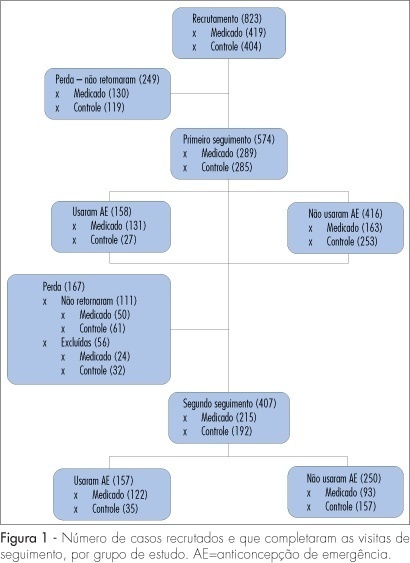
PURPOSE: to compare two strategies of access to emergency contraception: only information and information with previous delivery of this contraceptive method, and its relationship with the use of this method and the regular use of contraceptives. METHODS: from August 2004 to January 2005, 18 to 49-year-old volunteers, attended at reproductive health clinics from six Brazilian towns were recruited. The subjects were randomly distributed in a group getting information about emergency contraception (Control Group), or in a group getting information about this method and previous delivery of the contraceptive (Medicated Group). Follow-up visits occurred into four and eight months. Person and McNemar's tests were used for the statistical analysis. RESULTS: from the 823 recruited subjects, 407 completed the 8-month-observation period and were the sample analyzed. Most of the subjects (61%) did not use the emergency contraceptive. The subjects from the Medicated Group used more emergency contraceptives (57%) than the ones from the Control Group (18%), and they did it more precociously, concerning the time since the unprotected sexual intercourse. There was a significant increase of regular use of contraceptives among the subjects who used emergency contraceptives in the Medicated Group (88% versus 97%) and a statistically nonsignificant decrease in the Control Group. CONCLUSIONS: information and previous delivery intensified the access and use of emergency contraceptives, and did not reduce the regular use of contraceptives, including condoms.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2007;29(1):34-40
DOI 10.1590/S0100-72032007000100006
PURPOSE: to determine the cesarean section (CS) rate in Campinas (SP) and to identify its risk factors. METHODS: a cross-sectional study that analyzed data obtained from Live Birth Certificates in 2001. The dependent variable was the type of delivery and the independent variables were: mothers’ characteristics and those related to their pregnancies, deliveries and to newborns. The assessment of the association among variables was performed through the chi2 test, and crude and adjusted odds ratio (OR) values were calculated. RESULTS: the CS rate was 54.9%. The chances of having CS increased 1.9 times for women from 20-34 years old (adjOR-1.9; 95% CI:1.7-2.1); 3.7 times for those over 35 years old (adjOR-3.8; 95% CI:3.2-4.5); 1.5 times for those who studied from 8-11 years (adjOR-1.5; 95% CI:1.4-1.6); 2.5 times for those who studied more than 11 years (adjOR-2.6; 95% CI:2.2-2.9); 1.3 times for those who were married (adjOR-1.3; 95 % CI:1.2-1.4); 1.6 times for those who had jobs (adjOR-1.6; 95% CI:1.5-1.8); 1.2 times for who had good living conditions (adjOR-1.2; 95% CI:1.0-1.3); 2.2 times for primiparous (adjOR-2.2; 95% CI:1.9-2.5), 1.6 times for multiparous (adjOR-1.6; 95% CI:1.4-1.9) and 2.7 times in twin gestations (adjOR-2.7; 95% CI:1.9-3.9). The women who had inadequate prenatal care were protected for CS (adjOR-0.6; 95% CI:0.5-0.7). CONCLUSION: the chance of having CS was greater among women with better socio-economic conditions, with adequate prenatal care, for primiparous, for multiparous and in twin gestations, suggesting that the basis for indication of cesarean sections were not restricted to clinical factors but influenced by non-medical reasons.