Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2021;43(4):297-303
To evaluate the number of patients with early-stage breast cancer who could benefit from the omission of axillary surgery following the application of the Alliance for Clinical Trials in Oncology (ACOSOG) Z0011 trial criteria.
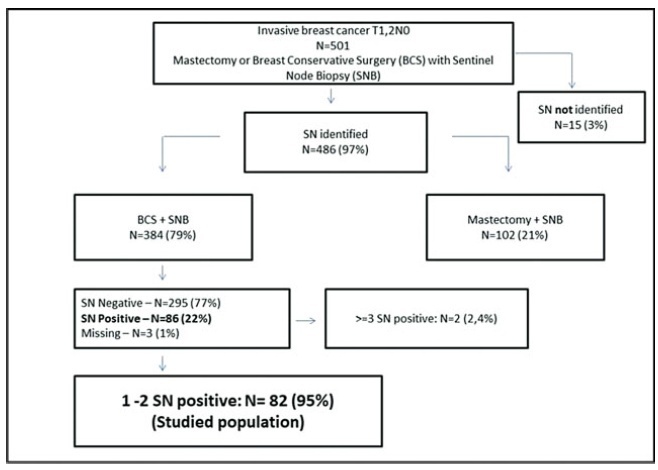
A retrospective cohort study conducted in the Hospital da Mulher da Universidade Estadual de Campinas. The study population included 384 women diagnosed with early-stage invasive breast cancer, clinically negative axilla, treated with breast-conserving surgery and sentinel lymph node biopsy, radiation therapy, chemotherapy and/or endocrine therapy, from January 2005 to December 2010. The ACOSOG Z0011 trial criteria were applied to this population and a statistical analysis was performed to make a comparison between populations.
A total of 384 patients underwent breast-conserving surgery and sentinel lymph node biopsy. Of the total number of patients, 86 women underwent axillary lymph node dissection for metastatic sentinel lymph nodes (SNLs). One patient underwent axillary node dissection due to a suspicious SLN intraoperatively, thus, she was excluded fromthe study. Among these patients, 82/86 (95.3%) had one to two involved sentinel lymph nodes andmet the criteria for the ACOSOG Z0011 trial with the omission of axillary lymph node dissection. Among the 82 eligible women, there were only 13 cases (15.9%) of lymphovascular invasion and 62 cases (75.6%) of tumors measuring up to 2 cm in diameter (T1).
The ACOSOG Z0011 trial criteria can be applied to a select group of SLNpositive patients, reducing the costs and morbidities of breast cancer surgery.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2014;36(3):118-123
DOI 10.1590/S0100-72032014000300005
To assess the feasibility and diagnostic accuracy of preoperative ultrasound combined with ultrasound-guided fine-needle aspiration (US-FNA) cytology and clinical examination of axillary lymph node in patients with breast cancer.
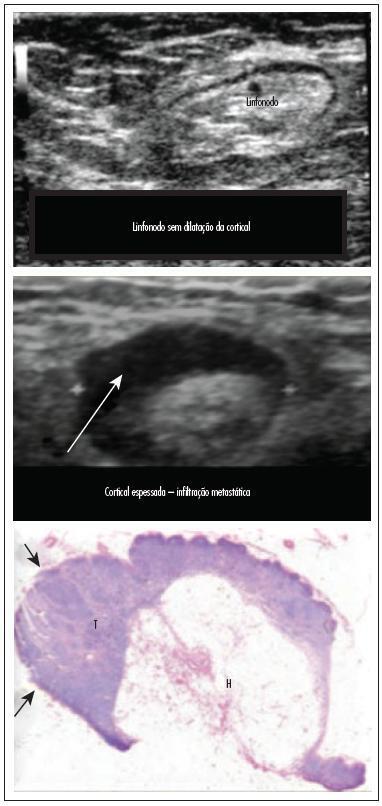
In this prospective study, 171 axillae of patients with breast cancer were evaluated by clinical examination and ultrasonography (US) with and without fine needle aspiration (FNA). Lymph nodes with maximum ultrasonographic cortical thickness > 2.3 mm were considered suspicious and submitted to US-FNA.
Logistic regression analysis showed no statistically significant correlation between clinical examination and pathologically positive axillae. However, in axillae considered suspicious by ultrasonography, the risk of positive anatomopathological findings increased 12.6-fold. Cohen's Kappa value was 0.12 for clinical examination, 0.48 for US, and 0.80 for US-FNA. Accuracy was 61.4% for clinical examination, 73.1% for US and 90.1% for US-FA. Receiver Operating Characteristics (ROC) analysis demonstrated that a cortical thickness of 2.75 mm corresponded to the highest sensitivity and specificity in predicting axillary metastasis (82.7 and 82.2%, respectively).
Ultrasonography combined with fine-needle aspiration is more accurate than clinical examination in assessing preoperative axillary status in women with breast cancer. Those who are US-FNA positive can be directed towards axillary lymph node dissection straight away, and only those who are US-FNA negative should be considered for sentinel lymph node biopsy.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2010;32(10):486-490
DOI 10.1590/S0100-72032010001000003
PURPOSE: to determine the efficacy of intraoperative injection of Dextran-500-99m-technetium (Tc) for the identification of the sentinel lymph node (SLN) in breast cancer and analyze time to label the SLN in the axillary region. METHODS: a prospective study between April 2008 and June 2009, which included 74 sentinel lymph node biopsies (SLNB) in patients with breast cancer in stages T1N0 and T2N0. After induction of anesthesia, 0.5 to 1.5 mCi of Dextran-500-99m-Tc filtered 0.22 µm in a volume of 5 mL was injected intraoperative using the subareolar technique for SLNB. After labeling with the radioisotope, 2 mL of patent blue was injected. The time elapsed between injection and the axillary hot spot, the in vivo and ex vivo counts of the hottest nodes, the background count, and the number of SLN identified were documented. Data were analyzed using descriptive statistics with SPSS program, version 18. RESULTS: we identified the SLN in 100% of cases. The rate of SLN identification with the probe was 98% (73/74 cases). In one case (1.35%) the SLN was labeled only with the blue dye. The mean dose of radioisotope injected was 0.97±0.22 mCi. The average time to label the SLN was 10.7 minutes (±5.7 min). We identified on average of 1.66 SLN labeled with the radioisotope. CONCLUSION: the procedure for SLN identification with an intraoperative injection of the radioisotope is oncologically safe and comfortable for the patient, providing agility to the surgical team.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2007;29(3):158-164
DOI 10.1590/S0100-72032007000300008
Axillary nodal metastasis is still the most important breast cancer prognostic factor. As in approximately 80% of the patients with tumors measuring less than 2 cm the axillary lymph nodes are negative, it has been proposed sentinel lymph node biopsy, reducing surgical morbidity in the patients with negative result. Recently, this technique has been widely used in Brazil, but there are two questions that need to be answered: what is the probability of a false-negative result (not diagnosing a positive lymph node) and if the understaging by false-negative result exposes the patient to the risk of axillary recurrence or even distant metastases, due to less effective surgical and adjuvant therapy. The literature shows that the false-negative rate varies from 5 to 10%, being the surgeon's experience the major factor that contributes to improved results. Although axillary relapse is rare, it is not yet possible to evaluate the long term effect of not removing positive lymph nodes, due to short follow-up. The recommendation is that sentinel lymph node biopsy should only be performed by surgeons with experience confirmed by a low false-negative rate.