Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2005;27(10):580-587
DOI 10.1590/S0100-72032005001000003
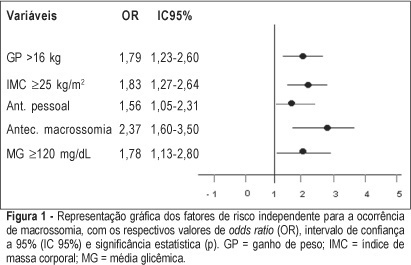
PURPOSE: to identify risk factors for fetal macrosomia in pregnant women with diabetes or daily hyperglycemia. METHODS: retrospective study, control-case, including 803 pairs of mothers and newborns belonging to this specific population, divided into two groups - macrosomic (cases, n=242) and non-macrosomic (controls, n=561). Variables regarding age, parity, weight and body mass index (BMI), weight gain (WG), diabetes history, high blood pressure and tabagism, diabetes type and classification, and glycemic control indicators in the third trimester were compared. The means were evaluated by the F test and the categorized variables were submitted to univariate analysis using the chi² test. The significative results were included in the multiple regression model for the identification of macrosomia independent risk considering OR, 95% CI and p value. The statistical significance limit of 5% was established for all analyses. RESULTS: there was a significative association between macrosomia and WG >16 kg, BMI >25 kg/m², personal, obstetric and macrosomic history, classification in the Rudge groups (IB and IIA + IIB), glycemic mean (GM) >120 mg/dL and postprandial glycemic mean >130 mg/dL in the third trimester. In the multiple regression analysis, WG >16 kg (OR=1,79; 95% CI: 1,23-1.60), BMI >25 kg/m² (OR=1.83; 95% CI: 1.27-2.64), personal history of diabetes (OR=1.56; 95% CI: 1.05-2.31) and of macrosomia (OR=2.37; 95% CI: 1.60-3.50) and GM >120 mg/dL in the third trimester (OR=1.78; 95% CI: 1.13-2.80) confirmed to be independent risk factors for macrosomia in these pregnancies. CONCLUSION: WG >16 kg, BMI >25 kg/m², GM >120 mg/dL in the third trimester and personal history of macrosomia and diabetes were identified as risk factors for fetal macrosomia in pregnant women with diabetes or daily hyperglycemia.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2005;27(6):331-339
DOI 10.1590/S0100-72032005000600007
PURPOSE: to evaluate the epidemiologic data and signs of trophoblastic hyperplasia in patients with complete hydatidiform mole (CHM) and to estimate the risk associated with the persistence of the disease. METHODS:: we evaluated 214 patients with CHM submitted to uterine evacuation between 1980 and 2001. The patients were included prospectively. All patients were followed until negative bHCG with weekly clinical evaluation and bHCG quantification. We considered persistence when the patient needed another treatment after uterine evacuation. The risk factors for persistence were evaluated through univariate and multivariate analysis, and the odds ratio (OR) was calculated for each one. RESULTS: among the epidemiologic factors, only negative Rh was significant (OR=2.28). All signs of trophoblastic hyperplasia, represented by uterine size larger than expected, sonographic uterine volume, tecaluteinic cysts, and betaHCG higher than 10(5) were associated with risk for the presistence of the disease. The presence of at least one sign of trophoblastic hyperplasia showed sensitivity of 82% and predictive positive value of 35.1% (OR=4.8). The logistic regression identified larger uterine size than expected and bHCG higher than 10(5) as risk factors for persistence of the gestational trophoblastic disease (OR=4.1 and 5.5, respectively). CONCLUSIONS: the signs of trophoblastic hyperplasia showed good sensitivity to predict persistence of the disease; however, the low predictive positive value does not allow using these criteria to change treatment. It is very important to reinforce the importance of serial betaHCG quantification in these high-risk patients.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2000;22(3):175-179
DOI 10.1590/S0100-72032000000300009
Purpose: to evaluate the route of delivery in a group of low-income primipara pregnant women with a previous cesarean section, and the factors associated with the repetition of the cesarean section on the second delivery. Patients and Methods: it was a case-control study including 356 women who were assisted at the Maternity of CAISM/UNICAMP during the period between January 1993 and January 1996. The cases were 153 women whose second delivery was through a cesarean section and the controls were 203 women whose second delivery was vaginal. For analysis, means, standard deviation, Student's t-test, Mann-Whitney test, chi² test and odds ratio (OR) with 95% CI for each factor possibly associated with cesarean section on the second delivery were used. Results: the route of the second delivery was vaginal for 57% of the women. Among the several variables studied, those which showed to be significantly associated with a cesarean section on the second delivery were: higher maternal age (for women over 35 years, OR = 16.4), previous abortions (OR = 2.09), induced labor (OR = 3,83), premature rupture of membranes (OR = 2.83), not having an epidural analgesia performed during labor (OR = 5.3), the finding of some alteration in fetal well-being (OR = 2.7) and the delivery occurring during the afternoon (OR = 1.92). Conclusions: these results indicate that the factors associated with the repetition of cesarean section in women with a previous scar of cesarean section in this population are predominantly medical; however, there is still the possibility of proposing interventions directed to decreasing the rates of repeated cesarean sections.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2005;27(5):268-274
DOI 10.1590/S0100-72032005000500007
PURPOSES: to analyze the frequency, associated risk factors for the occurrence of spina bifida and differences between the newborns carrying this malformation and the newborns' morbidities. METHODS: data were obtained through interview of 47 cases and 47 controls, born in the five maternities of the city of Pelotas, during the period from January 1, 1990 to December 31, 2003. This is a population-based case-control study, comprising all births occurred in hospitals. The control was the normal newborn that was born after each case with spina bifida. All data were obtained by using the model ECLAMC questionnaire. The planning of analysis of data included the use of the Student's t test, chi² and odds ratio. RESULTS: in this period there were approximately 77,000 births. Of these, 1,043 (1.35%) presented some type of congenital malformation. Among these, 47 of 162 anomalies of the neural tube (29%) were spina bifida cases. Significant differences have been found in the number of previous stillborn babies, as well as a higher rate of spina bifida cases in females. In this study, many factors such as the use of medical drugs; acute and chronic illnesses; number of gestations; age, education and occupation of the parents, among others, did not influence the occurrence of spina bifida. CONCLUSIONS: spina bifida must be considered as an important factor of risk for perinatal morbidity, and its occurrence is associated with a history of previous stillborn babies.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2005;27(4):189-196
DOI 10.1590/S0100-72032005000400005
PURPOSE: to create a predictive model for cesarean section at the "Professor Monteiro de Morais Maternity" after evaluation of antepartum risk factors of the pregnant women who delivered from September 1, 1999 to August 31, 2000, and then, to verify the efficacy of indication for cesarean section. METHODS: a longitudinal, case control study with 3.626 pregnant women was performed to identify the antepartum risk factors for cesarean section in the period from September 1, 1999 to August 31, 2000. Thereafter an ideal model able to quantify the risk for cesarean section for each patient in the presence of one or more risk factor was created. Then, the model was applied to the patients of the study in order to verify the efficacy of indication for cesarean section. RESULTS: the baseline risk for cesarean section was 15.2%. The concordance between the percentage estimated through logistic model and cesarean delivery was 86.6%. CONCLUSIONS: the logistic model was able to identify the baseline risk for cesarean section and to quantify the increase in risk for cesarean section in each patient when risk factors were introduced in the model. The model can be considered efficient and able to predict cesarean section because the agreemant between the prediction and the correct indication was 86.6%, and 53.6% of the patients who had vaginal delivery did not have any risk factor for cesarean section.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2003;25(7):507-512
DOI 10.1590/S0100-72032003000700007
PURPOSE: to evaluate the prevalence of osteoporosis in climacteric women and analyze the influence of general and reproductive risk factors on bone mineral density. METHODS: a cross-sectional study with the evaluation of the 473 hospital records of climacteric women followed up at the Menopause Outpatient Facility of CAISM/Unicamp, between 03/28/2000 and 04/17/2001. These women were at least 12 months in amenorrhea and presented the results of a bone densitometry study performed at the Nuclear Medicine Department of HC/Unicamp. The following variables were evaluated: age, color, body mass index, level of education, smoking, use of medication, age at menopause, parity, use and length of hormone replacement therapy and its effect on bone mineral density. Statistical analyses were performed using logistic regression ajusted by age and hormone replacement therapy use. RESULTS: the mean age of the studied women was 53.9 years (± 7.1 SD) with mean age at menopause being 45.9 years (± 6.9 SD). Osteoporosis occurred in 14.7% and osteopenia in 38% of the cases in the lumbar vertebrae (L2-L4 interspace) and in 3.8 and 32.7% in the femur, respectively. Logistic regression adjusted to age and hormone therapy showed an association between the following variables: level of education, age at menopause and body mass index. CONCLUSION: there was a high prevalence of osteoporosis and osteopenia in the studied population. Advanced age, lower level of education, late menarche, early menopause and lower body mass index were identified as risk factors for developing decreased bone mass in the studied population.