Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2024;46:e-rbgo85
To evaluate the role of being human immunodeficiency virus (HIV) positive for predicting the risk of recurrence in women with a cervical high grade squamous intraepithelial lesion (HSIL) diagnosis.
Retrospective observational case-control study, comprising HIV positive (case) and HIV negative (control) women in a 1:4 ratio. Women assisted by the Erasto Gaertner Hospital, between 2009-2018, with cervical HSIL diagnosis, submitted to treatment by Loop electrosurgical excision procedure (LEEP), and with a minimum follow-up of 18 months, were included. The immunological status, number and time to recurrence were analyzed, with p<0.05 considered significant. In a second analysis, only patients with free margins were evaluated.
The sample consisted of 320 women (64 cases and 256 controls). Presence of HIV, CD4 levels <200 and detectable viral load (CV) were associated with high risk of recurrence, with odds ratio (OR) of 5.4 (p<0.001/95CI:2.8-10); 3.6 (p<0.001 /IC95:0.6-21.1) and 1.8 (p=0.039 /IC95:0.3-9.3), respectively. In the sample with free margins (n=271), this risk was also higher among seropositive patients, with OR 4.18 (p=0.001/95CI:1.8-9.2).
HIV is an independent risk factor for cervical HSIL recurrence and reduced disease-free survival time. Glandular involvement, compromised margins, undetectable CV and CD4<200 also increase the risk of relapse.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2024;46:e-rbgo14
Postpartum hemorrhage (PPH) is the leading cause of maternal death globally. Therefore, prevention strategies have been created. The study aimed to evaluate the occurrence of PPH and its risk factors after implementing a risk stratification at admission in a teaching hospital.
A retrospective cohort involving a database of SISMATER® electronic medical record. Classification in low, medium, or high risk for PPH was performed through data filled out by the obstetrician-assistant. PPH frequency was calculated, compared among these groups and associated with the risk factors.
The prevalence of PPH was 6.8%, 131 among 1,936 women. Sixty-eight (51.9%) of them occurred in the high-risk group, 30 (22.9%) in the medium-risk and 33 (25.2%) in the low-risk group. The adjusted-odds ratio (OR) for PPH were analyzed using a confidence interval (95% CI) and was significantly higher in who presented multiple pregnancy (OR 2.88, 95% CI 1.28 to 6.49), active bleeding on admission (OR 6.12, 95% CI 1.20 to 4.65), non-cephalic presentation (OR 2.36, 95% CI 1.20 to 4.65), retained placenta (OR 9.39, 95% CI 2.90 to 30.46) and placental abruption (OR 6.95, 95% CI 2.06 to 23.48). Vaginal delivery figured out as a protective factor (OR 0.58, 95% CI 0.34 to 0.98).
Prediction of PPH is still a challenge since its unpredictable factor arrangements. The fact that the analysis did not demonstrate a relationship between risk category and frequency of PPH could be attributable to the efficacy of the strategy: Women classified as "high-risk" received adequate medical care, consequently.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2024;46:e-rbgo18
Despite the literature on dydrogesterone, studies on dydrogesterone utilization patterns are largely lacking in Indian patients.
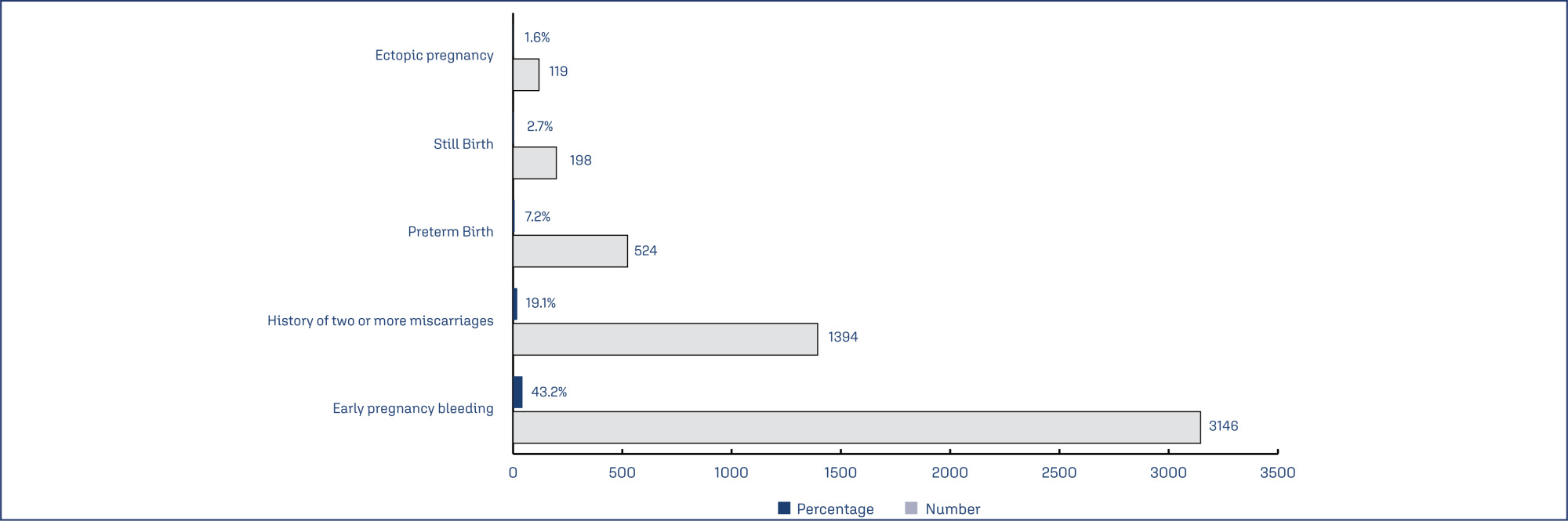
This was a multi-center, retrospective, observational, cross-sectional, and descriptive study across 817 centers in India. Data of patients who received dydrogesterone in past and provided consent for future use of their medical record for research purpose was were retrieved and analyzed.
Data of 7287 subjects (aged 29.55±4.84 years) was analyzed. Threatened abortion was the most common indication for which the subjects received dydrogesterone (46.9%) followed by recurrent pregnancy loss. Polycystic ovary syndrome (PCOS), thyroid disorders and anemia were the most common comorbid conditions and prior pregnancy loss, advanced maternal age and obesity were the most common risk factors seen in subjects who received dydrogesterone. Total 27.5% of subjects received a loading dose of dydrogesterone, and majority (64%) received 40 mg as loading dose. 10 mg dose was used as maintenance or regular dose in 81.4% of the subjects. Twice daily (BID) was the most common dosing frequency (66.6%). The most common concomitant medications being taken by the subjects on dydrogesterone included folic acid (45.1%), iron supplements (30.3%) and calcium and vitamin D3 supplements (25.5%). Another progesterone preparation (oral, injection, vaginal, tubal) other than dydrogesterone was used concurrently in 7.8% of subjects.
The study helped to identify the patient population that is benefitted by dydrogesterone and the preferred indications, risk factors, comorbid conditions and concomitant medication used in this patient population at real-life scenario.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2024;46:e-rbgo62
To report the prevalence of malignant transformation of vulvar lichen sclerosus (VLS) and possible risk factors.
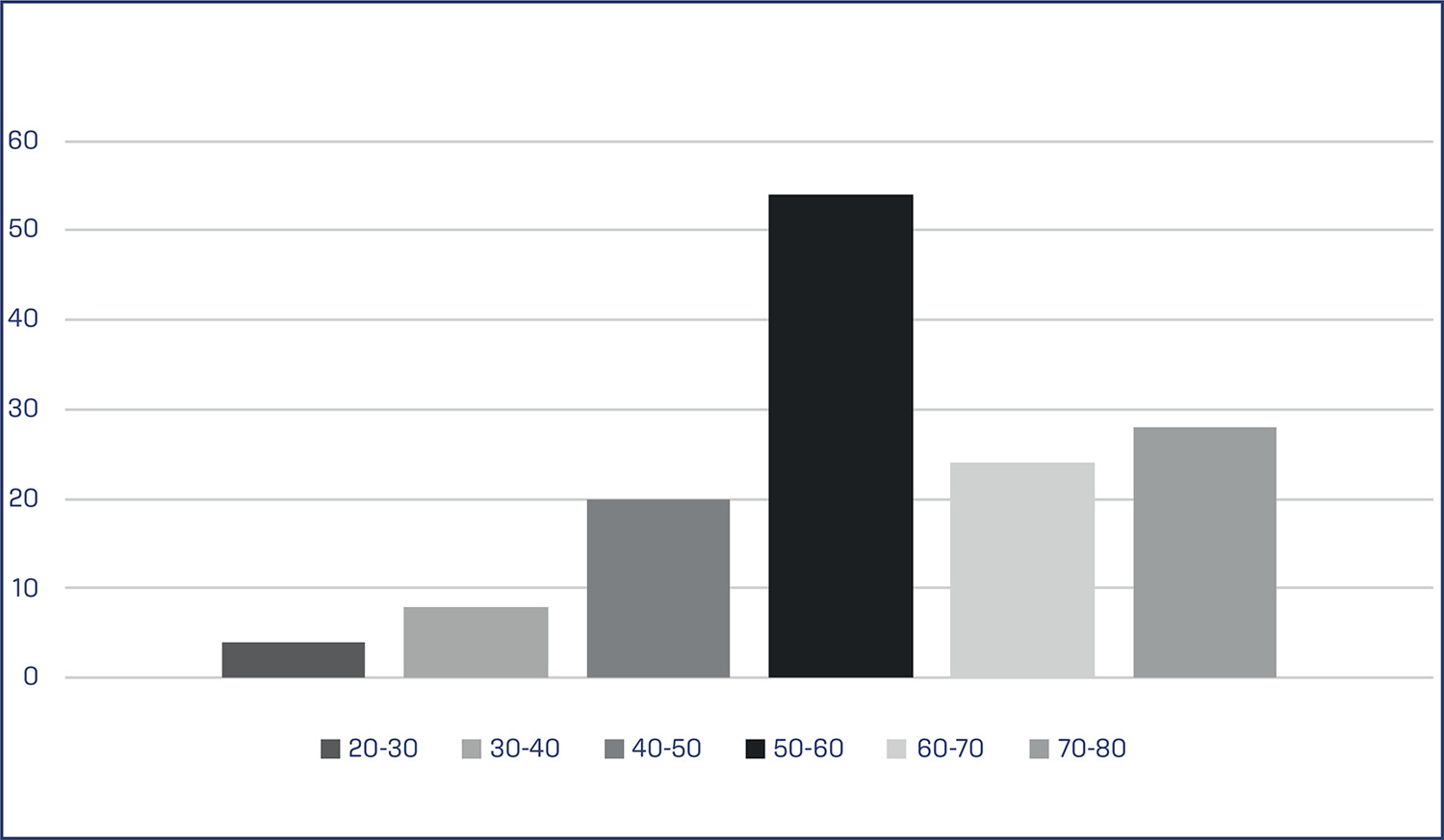
This is a cohort study with data analysis from medical records of 138 patients with histological diagnosis of VLS registered at the Vulvar Pathology Outpatient Clinic of the University Hospital, between 2007 and 2017. Predominance of risk factors was performed using logistic regression analysis. The variables studied were the length of follow-up, age, regular or irregular follow up; presence of symptoms (dyspareunia, pruritus and/or vulvar burning); histology characteristics, the presence of epithelial hyperplasia; and the presence of autoimmune diseases.
There were 138 patients included in the study, and among them five progressed to malignant transformation. The patients had a median age of 59 years and 83% were symptomatic. The most frequent symptom was itching with 72%. Autoimmune diseases were present in 11.6%, the most prevalent being thyroid disease. All five case of malignant transformation (0.6%) had an irregular follow up. The logistic regression analysis was used among the studied variables, and no statistical significance was found among them (p ≥ 0.05). The relationship between hyperplasia and the clinical outcome of malignant transformation, in which non-significant but acceptable p value close to 0.05 was observed.
The prevalence of malignant transformation in patients with VLS was 0.6%, and common factors were the lack of adherence to medical treatments and the loss of follow-up.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2024;46:e-rbgo53
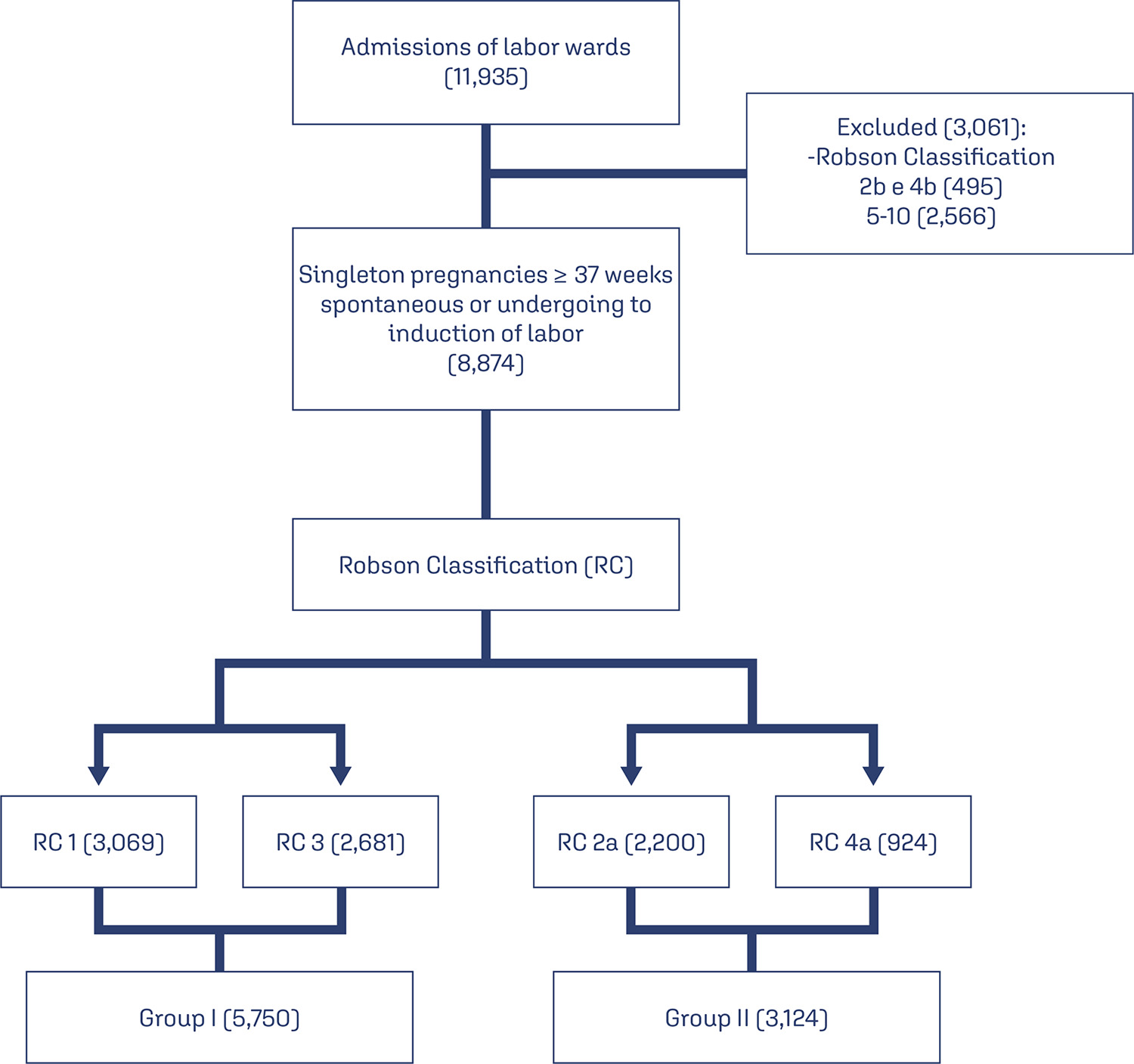
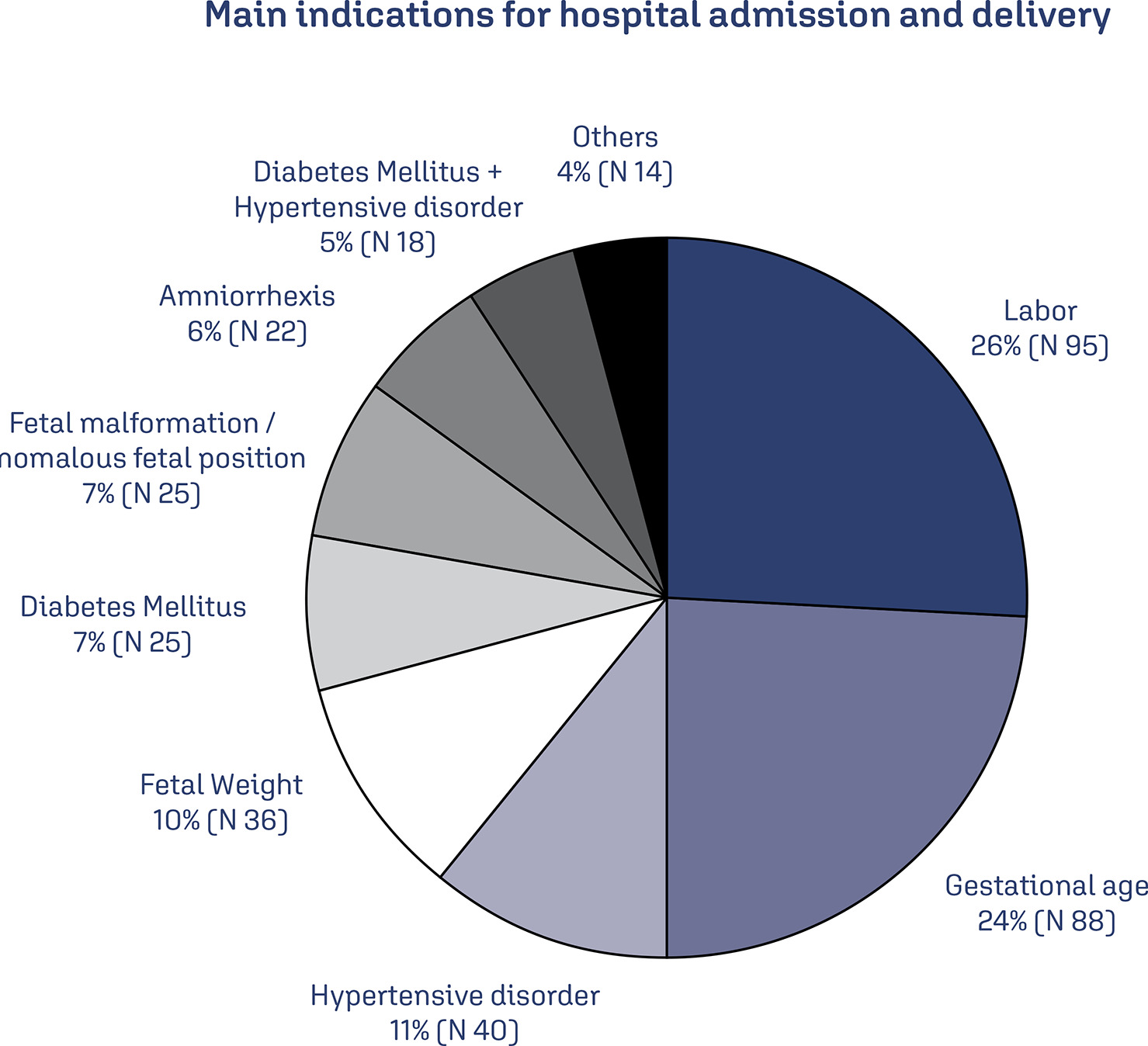
To evaluate the risk factors for postpartum hemorrhage (PPH) according to the Robson Classification in a low-risk maternity hospital.
We conducted retrospective cohort study by analyzing the medical records of pregnant women attended in a low-risk maternity hospital, during from November 2019 to November 2021. Variables analyzed were: maternal age, type of delivery, birth weight, parity, Robson Classification, and causes of PPH. We compared the occurrence of PPH between pregnant women with spontaneous (Groups 1 and 3) and with induction of labor (2a and 4a). Chi-square and Student t-tests were performed. Variables were compared using binary logistic regression.
There were 11,935 deliveries during the study period. According to Robson’s Classification, 48.2% were classified as 1 and 3 (Group I: 5,750/11,935) and 26.1% as 2a and 4a (Group II: 3,124/11,935). Group II had higher prevalence of PPH than Group I (3.5 vs. 2.7%, p=0.028). Labor induction increased the occurrence of PPH by 18.8% (RR: 1.188, 95% CI: 1.02-1.36, p=0.030). Model including forceps delivery [x2(3)=10.6, OR: 7.26, 95%CI: 3.32-15.84, R2 Nagelkerke: 0.011, p<0.001] and birth weight [x2(4)=59.0, OR: 1.001, 95%CI:1.001-1.001, R2 Nagelkerke: 0.033, p<0.001] was the best for predicting PPH in patients classified as Robson 1, 3, 2a, and 4a. Birth weight was poor predictor of PPH (area under ROC curve: 0.612, p<0.001, 95%CI: 0.572-0.653).
Robson Classification 2a and 4a showed the highest rates of postpartum hemorrhage. The model including forceps delivery and birth weight was the best predictor for postpartum hemorrhage in Robson Classification 1, 3, 2a, and 4a.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2024;46:e-rbgo48
Evaluate the prevalence of macrosomic newborns (birth weight above 4000 grams) in a high-risk maternity from 2014 to 2019, as well as the maternal characteristics involved, risk factors, mode of delivery and associated outcomes, comparing newborns weighing 4000-4500 grams and those weighing above 4500 grams.
This is an observational study, case-control type, carried out by searching for data in hospital’s own system and clinical records. The criteria for inclusion in the study were all patients monitored at the service who had newborns with birth weight equal than or greater than 4000 grams in the period from January 2014 to December 2019, being subsequently divided into two subgroups (newborns with 4000 to 4500 grams and newborns above 4500 grams). After being collected, the variables were transcribed into a database, arranged in frequency tables. For treatment and statistical analysis of the data, Excel and R software were used. This tool was used to create graphs and tables that helped in the interpretation of the results. The statistical analysis of the variables collected included both simple descriptive analyzes as well as inferential statistics, with univariate, bivariate and multivariate analysis.
From 2014 to 2019, 3.3% of deliveries were macrosomic newborns. The average gestational age in the birth was 39.4 weeks. The most common mode of delivery (65%) was cesarean section. Diabetes mellitus was present in 30% of the deliveries studied and glycemic control was absent in most patients. Among the vaginal deliveries, only 6% were instrumented and there was shoulder dystocia in 21% of the cases. The majority (62%) of newborns had some complication, with jaundice (35%) being the most common.
Birth weight above 4000 grams had a statistically significant impact on the occurrence of neonatal complications, such as hypoglycemia, respiratory distress and 5th minute APGAR less than 7, especially if birth weight was above 4500 grams. Gestational age was also shown to be statistically significant associated with neonatal complications, the lower, the greater the risk. Thus, macrosomia is strongly linked to complications, especially neonatal complications.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2024;46:e-rbgo64
To evaluate whether there were differences in the presentation of patients with tubal ectopic pregnancy (EP) during the first year of the COVID-19 pandemic.
We performed a retrospective cohort study of all cases of tubal EP between March 2019 and March 2020 (pre-pandemic) and between March 2020 and March 2021 (pandemic). We compared between these two groups the risk factors, clinical characteristics, laboratory data, sonographic aspects, treatment applied and complications.
We had 150 EP diagnoses during the two years studied, of which 135 were tubal EP. Of these, 65 were included in the pre-pandemic and 70 in the pandemic period. The prevalence of lower abdominal pain was significantly higher in the pandemic compared to the pre-pandemic period (91.4% vs. 78.1%, p=0.031). There was no significant difference in shock index, initial beta-hCG level, hemoglobin level at diagnosis, days of menstrual delay, aspect of the adnexal mass, amount of free fluid on ultrasound, and intact or ruptured presentation between the groups. Expectant management was significantly higher during the pandemic period (40.0% vs. 18.5%, p=0.008), surgical management was lower during the pandemic period (47.1% vs. 67.7%, p=0.023), and number of days hospitalized was lower in the pandemic period (1.3 vs. 2.0 days, p=0.003).
We did not observe a significant difference in patient history, laboratory and ultrasound characteristics. Abdominal pain was more common during the pandemic period. Regarding treatment, we observed a significant increase in expectant and a decrease in surgical cases during the pandemic period.