Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2011;33(5):211-218
DOI 10.1590/S0100-72032011000500002
PURPOSE: the aim of this study was to analyze conjoined twins in terms of antenatal, delivery and postnatal aspects. METHODS: a retrospective descriptive analysis of prenatally diagnosed conjoined twins. Prenatal ultrasound and echocardiography, delivery details, postnatal follow-up, surgical separation and post mortem data were reviewed. The twins were classified according to the type of fusion between fetal structures. The following data were analyzed: ultrasound and echocardiographic findings, antenatal lethality and possibility of surgical separation, delivery details and survival rates. RESULTS: forty cases of conjoined twins were included in the study. There were 72.5% cases of thoracophagus, 12.5% of paraphagus, 7.5% of omphalo-ischiophagus, 5.0% of omphalophagus, and 2.5% of cephalophagus. Judicial termination of pregnancy was requested in 58.8% of the cases. Cesarean section was performed in all cases in which pregnancy was not terminated. The mean gestational age at delivery was 35 weeks; all twins were live births with a mean birth weight of 3,860 g and 88% died postnatally. Ten percent of the live borns were submitted to surgical separation with a 60% survival rate. The total survival rate was 7.5% and postnatal survival was 12%. Antenatal evaluation of lethality and possibility of surgical separation were precise. There were no maternal complications related to delivery. CONCLUSION: conjoined twins present a dismal prognosis mainly related to the complex cardiac fusion present in the majority of cases with thoracic sharing. At referring centers, prenatal ultrasound and echocardiographic evaluation accurately delineate fetal prognosis and the possibility of postnatal surgical separation.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2010;32(2):61-65
DOI 10.1590/S0100-72032010000200002
PURPOSE: to analyze the occurrence of conjoined twins at a tertiary perinatology reference university hospital over a period of 25 years (January 1982 to January 2007) and to describe the successful separation of one of the pairs. METHODS: we consulted retrospectively the database of the University Hospital of the Medical School of Ribeirão Preto, University of São Paulo, Brazil, in order to determine the number of pairs of conjoined twins, their frequency, classification, gender, type of pregnancy resolution, attempted surgical separation, prenatal diagnosis and survival. RESULTS: we detected 14 pairs of conjoined twins (1/22,284 live births and 1/90 pairs of twin live births) born during this period (six males, seven females and one of indeterminate sex). The prenatal diagnosis was performed in all twins and all births were accomplished by cesarean section. The separation was possible in only one pair, which survives in excellent health conditions after eight years. Of the remaining 13, ten died on the day of birth and three survived only a few months (less than one year). CONCLUSION: Although our study revealed an abnormally high number of conjoined twins, this is a rare phenomenon, with a poor perinatal prognosis depending on the organs shared by the twins and associated malformations, especially those related to the fetal heart. Due to the poor prognosis of these pairs and to the maternal reproductive impairment caused by the need to perform body cesareans, we suggest that, based on these numbers, early interruption of these pregnancies be legally granted, as in the case of other diseases incompatible with fetal survival outside the uterus. Thus, the confirmation of a diagnosis of conjoined twins and the resolution of pregnancy should be performed at a tertiary obstetric and perinatal care center, and an authorization for the interruption of pregnancy should be obtained by judicial means.

Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2009;31(4):164-170
DOI 10.1590/S0100-72032009000400002
PURPOSE: to determine factors associated to amniotic fluid volume and frequencies of fetal anomalies, in a reference center in Pernambuco. METHODS: a transversal study performed in high-risk pregnant women submitted to obstetrical morphological ultrasound, from March 2002 to March 2006, at an institution from Recife, Pernambuco, Brasil. The intrauterine diagnosis was confirmed after birth. Sociodemographic and obstetrical characteristics, amniotic liquid volume and presence of fetal anomalies were the variables studied. Fisher's exact, χ2, and Student's t tests, at a significance level of 5% were applied to verify the correlation among the variables. Prevalence rate and confidence interval at 95% were calculated. Multiple logistic regression analysis was performed at a significance level of 5%. RESULTS: Two hundred and fifty-seven pregnant women (56.2%) with congenital anomalies and 200 (43.8%) without anomalies, confirmed in the postnatal, were included in the study. The average of maternal ages and gestation periods were 24.8±6.5 years and 35.9±3.7 weeks, respectively. The fetal anomalies were discovered in the central nervous system (50.6%) and genitourinary tract (23.0%). The presence of congenital anomalies were significantly linked with reduced liquid/oligohydramnios (p=0.0002) and increased liquid/polyhydramnios (p<0.0001). Intrauterine mortality was more frequent in the group with anomalies, as compared to the healthy fetuses (10.5 versus 2.5%; p<0.01). CONCLUSIONS: The rate of congenital anomalies in the high-risk pregnant women group was 56.2%. Most of the central nervous system malformations were diagnosed intrauterus. Changes in the amniotic fluid were the factors more strongly associated with congenital anomalies.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2009;31(2):90-93
DOI 10.1590/S0100-72032009000200007
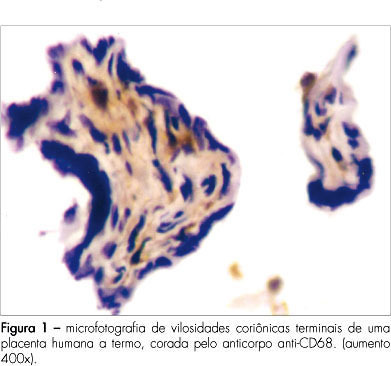
PURPOSE: to verify the amount of CD68+ cells in chorionic villosities in placentae from gestations submitted or not to labor. METHODS: transversal study with healthy near-term pregnant women, among whose placentae, 31 have been examined by immunohistochemical technique. Twenty placentae were obtained after vaginal delivery (VAGG) and eleven after elective cesarean sections (CESG). Slides were prepared with chorionic villosities samples and labeled with anti-CD68 antibody, specific for macrophages. Labeled and nonlabeled cells were counted inside the villosities. Non-parametric statistical tests were used for the analysis. RESULTS: among the 6,424 cells counted in the villosities' stroma from the 31 placentae, 1,135 cells (17.6%) were stained by the CD68+. The mean of cells labeled by the anti-CD68 was 22±18 for the VAGG group and 20±16 for the CESG, in each placentary sample. CONCLUSIONS: there were no significant differences in the percentage of macrophages (CD68+) in association with labor.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2007;29(12):647-653
DOI 10.1590/S0100-72032007001200008
Screening for major chromosomal abnormalities can be provided in the first trimester of pregnancy. Screening by a combination of fetal nuchal translucency and maternal serum free human chorionic gonadotropin and pregnancy-associated plasma protein-A can identify 90% of fetuses with trisomy 21 and other major chromosomal abnormalities for a false-positive rate of 5%. This is superior to the 30% detection rate achieved by maternal age and 65% by second-trimester maternal serum biochemistry. A further improvement in the effectiveness of first-trimester screening is likely to be achieved by a risk-orientated two-stage approach. In this approach, the patients are subdivided into a high-risk group, requiring invasive testing; a low-risk group, which can be reassured that an abnormality is unlikely, and an intermediate-risk group (risk of 1 in 101 to 1 in 1000), in which further assessment is performed by first-trimester ultrasound examination (for presence/absence of the nasal bone or presence/absence of tricuspid regurgitation or normal/abnormal Doppler velocity waveform in the ductus venosus), and chorionic villus sampling is performed if their adjusted risk becomes 1 in 100 or more. Those performing first-trimester scans should be appropriately trained and their results subjected to external quality assurance. This process was well established by the Fetal Medical Foundation several years ago and is widely accepted internationally.

Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2007;29(7):358-365
DOI 10.1590/S0100-72032007000700006
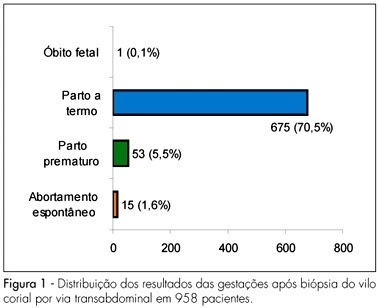
PURPOSE: to evaluate fetal maternal complications after chorionic villus sampling (CVS) for prenatal diagnosis of genetic disorders in pregnant women of Salvador (BA), Brazil. METHODS: case-series study of 958 pregnancies with high risk for chromosomal abnormality submitted to CVS transabdominal between the ninth to the 24th week of gestation, using an ultrasound-guided 18G 3½ spinal needle, from 1990 to 2006. The variables for the analysis of immediate complications were uterine cramps, subchorionic hematoma, accidental amniotic cavity punction, pain in the punction area, amniotic fluid leakage, abdominal discomfort, fetal arrhythmias and vaginal bleeding, and of late complication, abdominal pain, vaginal bleeding, amniotic fluid leakage, infection and spontaneous miscarriage. Premature labor, obstetrical complications (abruption placenta and placenta previa) and newborn malformation were also studied. Qui-square, Student’s "t" or Mann-Whitney tests were used for the statistical analysis; the significance level was 5%. RESULTS: maternal mean age was 36.3±4.9 years old. Immediate complications ware found in 182 (19%) cases (uterine cramp in 14%, subchorionic hematoma in 1.8% and accidental amniotic cavity punction in 1.3%). Late complications were found in 32 (3.3%) cases (vaginal bleeding in 1.6%, abdominal pain in 1.4%, amniotic fluid leakage in 0.3% and spontaneous miscarriage in 1.6% cases). There was no case of abruption placentae, placenta previa or fetal malformation. CONCLUSIONS: CVS is a simple and safe procedure. CVS should be performed in high risk pregnant patients who need prenatal diagnosis of fetal chromosomal abnormalities.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 1998;20(1):47-49
DOI 10.1590/S0100-72031998000100008
We report a case in which there was spontaneous regression of hydrops fetalis. Hydrops was probably caused by fetal infection with parvovirus B19. Anemia and hypokinesia of the heart were also observed. Diagnosis was accomplished by the ultrasound, virus detection in maternal serum, complete fetal blood count, and analysis of hepatic enzymes.

Summary
Revista Brasileira de Ginecologia e Obstetrícia. 1998;20(7):381-387
DOI 10.1590/S0100-72031998000700003
Objective: to evaluate the diagnosis, characteristics of pregnancy, maternal complications and perinatal outcome in cases of congenital hydrocephalus, and to associate them with pregnancy and delivery variables. Methods: 116 pregnancies with this diagnosis were evaluated before or after delivery, 112 of them occurring at the Maternity ward of CAISM/UNICAMP during the period between 1986 and 1995. For perinatal variables, complete data of 82 newborns were used. For data analysis, distributions and means were calculated and c² and Fisher exact tests were applied. Results: generally the diagnosis was made before delivery, confirmed by ultrasound and the delivery was through a cesarean section in cases. Cephalocentesis was performed in 11 cases and complications were more frequent in vaginal delivery than cesarean section. Low Apgar scores were more frequent among newborn babies delivered vaginally. Congenital hydrocephalus was also associated with important neonatal and perinatal morbidity and mortality, with other malformations, and a very low number of children without sequelae. Conclusions: the evaluation of these factors may be of great value for the obstetrician who is following pregnant women with this fetal malformation. This could better support the decisions that, although medical and ethical, should take into account the risk-benefit ratio of measures to be taken.