Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2012;34(5):228-234
DOI 10.1590/S0100-72032012000500007
PURPOSE: To evaluate habits of sun exposure and sun protection of pregnant women in a public hospital, to assess orientation about photo protection during the prenatal care, and to detect the presence of melasma and its impact on their quality of life. METHODS: A descriptive cross sectional study conducted among women of 18 years old and older, after delivery, who participated in a program of prenatal care in the South Region of Brazil. The sample was non-probabilistic by convenience. Data collection occurred from July to August 2011 through direct interview using a structured questionnaire to obtain personal information and photo protection habits during pregnancy, skin assessment and photographic record of lesions through informed consent. The skin was classified per Fitzpatrick's phototypes and the melasma was diagnosed clinically. In the patients with melasma, the MELASQoL-PB version was applied. The analysis was performed using Statistica®, version 8.0, and the significance level of p<0.05. RESULTS: In the sample (109 mothers) predominated white women (60.6% phototype III), young (average age 24.4 years SD=6.1) and housewives (59.6%). The majority (80%) stayed exposed to sunlight for 1-2 hours per day between 10 am and 3 pm, and from those (72%) did not apply any photoprotection due to lack of sunscreen habit. Other physical means of sun protection were used by 15% of these patients. Information during prenatal care about the risks of sun exposure was reported by 34% of the mothers interviewed. There was a trend toward a significant association between prenatal guidance and daily use of sunscreen (p=0.088). About 20% of mothers had melasma. The average score MELASQol-PB (25) showed a negative impact on quality of life of these patients. CONCLUSION: In these women, sun exposure occurred at inappropriate times, without proper guidance and without the use of an effective sunscreen. The mothers with melasma complained about the appearance of their skin, frustration and embarrassment.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2012;34(3):118-121
DOI 10.1590/S0100-72032012000300005
PURPOSE: To report the use of colpotomy for the treatment of ectopic pregnancies. METHODS: This was a retrospective cross-sectional study conducted on all women hospitalized with a clinical-laboratory suspicion of ectopic pregnancy who did not fulfill the criteria for drug treatment with methothrexate, during the period from February 2007 to August 2008. Demographic variables, gynecologic history and characteristics associated with treatment were obtained by reviewing the medical records. RESULTS: Eighteen women were included in the study. Mean age was 27±5.2 years. All patients presented ruptured ectopic pregnancy and all were submitted to partial salpingectomy. Surgical time ranged from 30 to 120 minutes (mean: 64.5 minutes) calculated from the moment when the patient entered the operating room to the moment when she left it. No patient presented postoperative infection. Mean time of hospitalization was 40±14.3 hours. The medications used during the postoperative period were similar in all cases, being based on nonsteroid anti-inflammatory drugs, dipyrone, paracetamol and meperidine, as needed. The diet was reintroduced 8 hours after the end of surgery. CONCLUSIONS: The use of colpotomy in the treatment of ectopic pregnancy showed good results, with the absence of important complications and a short hospitalization time. The basic surgical instruments needed for this procedure are relatively common to all hospitals, and the surgical technique is reproducible.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2012;34(3):107-112
DOI 10.1590/S0100-72032012000300003
PURPOSE: To analyze the influence of maternal nutritional status, weight gain and energy consumption on fetal growth in high-risk pregnancies. METHODS: A prospective study from August 2009 to August 2010 with the following inclusion criteria: puerperae up to the 5th postpartum day; high-risk singleton pregnancies (characterized by medical or obstetrical complications during pregnancy); live fetus at labor onset; delivery at the institution; maternal weight measured on the day of delivery, and presence of medical and/or obstetrical complications characterizing pregnancy as high-risk. Nutritional status was assessed by pregestational body mass index and body mass index in late pregnancy, and the patients were classified as: underweight, adequate, overweight and obese. A food frequency questionnaire was applied to evaluate energy consumption. We investigated maternal weight gain, delivery data and perinatal outcomes, as well as fetal growth based on the occurrence of small for gestational age and large for gestational age neonates. RESULTS: We included 374 women who were divided into three study groups according to newborn birth weight: adequate for gestational age (270 cases, 72.2%), small for gestational age (91 cases, 24.3%), and large for gestational age (13 cases, 3.5%). Univaried analysis showed that women with small for gestational age neonates had a significantly lower mean pregestational body mass index (23.5 kg/m², p<0.001), mean index during late pregnancy (27.7 kg/m², p<0.001), and a higher proportion of maternal underweight at the end of pregnancy (25.3%, p<0.001). Women with large for gestational age neonates had a significantly higher mean pregestational body mass index (29.1 kg/m², p<0.001), mean index during late pregnancy (34.3 kg/m², p<0.001), and a higher proportion of overweight (30.8%, p=0.02) and obesity (38.5%, p=0.02) according to pregestational body mass index, and obesity at the end of pregnancy (53.8%, p<0.001). Multivariate analysis revealed the index value during late pregnancy (OR=0.9; CI95% 0.8-0.9, p<0.001) and the presence of hypertension (OR=2.6; 95%CI 1.5-4.5, p<0.001) as independent factors for small for gestational age. Independent predictors of large for gestational age infant were the presence of diabetes mellitus (OR=20.2; 95%CI 5.3-76.8, p<0.001) and obesity according to body mass index during late pregnancy (OR=3.6; 95%CI 1.1-11.7, p=0.04). CONCLUSION: The maternal nutritional status at the end of pregnancy in high-risk pregnancies is independently associated with fetal growth, the body mass index during late pregnancy is a protective factor against small for gestational age neonates, and maternal obesity is a risk factor for large for gestational age neonates.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2012;34(1):22-27
DOI 10.1590/S0100-72032012000100005
PURPOSE: Evaluate the effects of ipriflavone during fetogenesis, since no studies have been conducted to assess its effect during this period. METHODS: 60 pregnant rats were divided randomly into four groups (n=15). G-control (1 mL of distilled water) and three groups treated intragastrically with ipriflavone from the 16th to the 20th post coitus (PC) day: G-300 (300 mg/kg), G-1,500 (1,500 mg/kg) and G-3,000 (3,000 mg/kg). The animals were weighed, anaesthetized intraperitoneally with xylazine and ketamine at doses of 180 mg/kg and 10 mg/kg, respectively, and sacrificed by total exsanguination on the 21st day. A complete blood count was performed and serum cholesterol, triglycerides, AST, ALT, urea, creatinine, and glucose were determined in pregnant rats. After laparotomy, the liver, kidneys, adrenals, spleen and ovaries were removed and weighed; fetuses and placentas were also weighed to obtain the average weight of the litters. Four fetuses (two males and two females) were chosen at random for the determination of the length and weight of brain, liver, kidneys and lungs. Statistical analysis: ANOVA followed by Dunnett's test. For raw data without normal distribution and homoscedasticity, we used the Kruskal-Wallis test followed by the Mann-Whitney test. Proportions were analyzed by the χ² test (p<0.05). RESULTS: Triglyceride levels (mg/dL) were: Control-G (138.8±21.8), G-300 (211.2±63.9) G-1,500 (251.5±65.2) G-3,000 (217.7±49.6); p<0.05. The body weight of fetuses (g) was: G-Control (male 3.3±0.3; female 3.1±0.3), G-300 (male 3.4±0.2; female 3.1±0.4), G-1,500 (male 3.5±0.3; female 3.2±0.3), G-3,000 (male 3.4±0.5; female 3.1±0.4). CONCLUSION: Ipriflavone did not cause maternal toxicity, but increased triglyceride levels and reduced hematocrit at higher doses. The body and organ weights of the fetuses did not change with dam treatment. There were no external malformations or fetal deaths.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2011;33(12):388-394
DOI 10.1590/S0100-72032011001200003
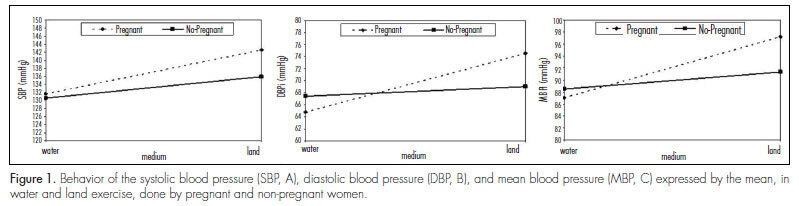
PURPOSE: to compare the blood pressure and oxygen consumption (VO2) responses between pregnant and non-pregnant women, during cycle ergometer exercise on land and in water. METHODS: ten pregnant (27 to 29 weeks of gestation) and ten non-pregnant women were enrolled. Two cardiopulmonary tests were performed on a cycle ergometer (water and land) at the heart rate corresponding to VO2, over a period of 30 minutes each. Exercise measurements consisted of recording blood pressure every five minutes, and heart rate and VO2 every 20 seconds. Two-way ANOVA was used and α=0.05 (SPSS 17.0). RESULTS: there was no difference in cardiovascular responses between pregnant and non-pregnant women during the exercise. The Pregnant Group demonstrated significant differences in systolic (131.6±8.2; 142.6±11.3 mmHg), diastolic (64.8±5.9; 74.5±5.3 mmHg), and mean blood pressure (87.0±4.1; 97.2±5.7 mmHg), during water and land exercise, respectively. The Non-pregnant women Group also had a significantly lower systolic (130.5±8.4; 135.9±8.7 mmHg), diastolic (67.4±5.7; 69.0±10.1 mmHg), and mean blood pressure (88.4±4.8; 91.3±7.8 mmHg) during water exercise compared to the land one. There were no significant differences in VO2 values between water and land exercises or between pregnant and non-pregnant women. After the first five-minute recovery period, both blood pressure and VO2 were similar to pre-exercise values. CONCLUSIONS: for pregnant women with 27 to 29 weeks of gestation, water exercise at the heart rate corresponding to VO2 is physiologically appropriate. These women also present a lower blood pressure response to exercise in water than on land.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2011;33(11):348-353
DOI 10.1590/S0100-72032011001100005
PURPOSE: To describe the obstetric outcome of women with overweight/obesity treated at the prenatal care clinic of a public maternity hospital in Rio de Janeiro. METHODS: A descriptive cross-sectional study which investigated 433 women (³20 years-old, without any chronic diseases) and their newborns treated at public hospitals in Rio de Janeiro. Information was collected from medical records and through interviews. The characteristics of mothers and newborns evaluated were divided into maternal (social habits, anthropometric measurements and clinical, obstetric, and prenatal care) and newborn groups (birth conditions). Data regarding the categories of nutritional status were analyzed using the odds ratio (OR) and 95% confidence interval (CI). RESULTS: The prevalence of overweight/obesity in this sample was 24.5% (n=106). There was an association between inadequate weight gain and the prevalence of overweight/obesity (OR 2.7, 95%CI 1.5-4.9, p<0.05). Overweight/obese women had an increased risk for preeclampsia (OR 3.3, 95%CI 1.1--9.9, p=0.03). Regarding birth conditions, mean birth weight was 3291.3 g (±455.2), with rates of low birth weight of 4.7% (n=5) and rates of macrosomia of 2.8% (n=3). CONCLUSIONS: There was an alarming prevalence of inadequate nutritional status before and during pregnancy, which may be associated with increased risk of perinatal morbidity and mortality. This suggests the need for nutritional monitoring of these pregnant women.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2011;33(11):341-347
DOI 10.1590/S0100-72032011001100004
PURPOSE: To evaluate the pregnancy rate in intrauterine insemination (IUI), and to determine possible prognostic factors of successful pregnancy. METHODS: A retrospective study of IUI cycles performed in the Reproductive Medicine Unit of Vila Nova de Gaia Hospital, between January 2007 and July 2010. The IUI cycles were preceded by ovarian stimulation and monitored by vaginal ultrasound. Clinical pregnancy rates were analyzed according to the woman’s age, type and duration of infertility, spermatozoa parameters assessed in the spermogram, number of mature follicles and the drug used for ovarian stimulation. Statistical analysis was performed using the Statistical Package for the Social Sciences (SPSS17), with the level of significance set at p<0.05. RESULTS: The study comprised 139 couples who underwent 220 IUI cycles. The absolute pregnancy rate per cycle was 18.6%. Of the 41 clinical pregnancies, 5 were twin pregnancies (12.1%). The pregnancy rate was higher at ages <30 years (28.5 vs 15.7%; p=0.024), duration of infertility <3 years (23.8 vs 13.9%; p=0.05), normal sperm motility (23.2 vs 10.3%; p=0.01) and with two follicles at the time of insemination (27.7 vs 14.2% for monofollicular growth; p=0.030). The pregnancy rates obtained with clomiphene citrate, gonadotropins and combined clomiphene citrate/gonadotropin were 13.0, 26.1 and 28.6%, respectively, with a statistically significant difference in clinical pregnancy rate between clomiphene citrate and gonadotropin. CONCLUSIONS: IUI remains a natural starting point for conveniently selected couples with infertility. Younger age and normal sperm motility are good prognostic factors. Gonadotrophin stimulation seems to be an important tool for improving the pregnancy rate of IUI.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2011;33(10):280-285
DOI 10.1590/S0100-72032011001000002
PURPOSE: To analyze the results of assessment of fetal well-being in pregnancies complicated by moderate or severe maternal thrombocytopenia. METHODS: Data from April 2001 to July 2011 of 96 women with a diagnosis of thrombocytopenia in pregnancy were retrospectively analyzed. We analyzed the following tests performed during the antepartum period for fetal assessment: cardiotocography, fetal biophysical profile, amniotic fluid index and umbilical artery Doppler velocimetry. RESULTS: A total of 96 pregnancies with the following diagnoses were analyzed: gestational thrombocytopenia (n=37, 38.5%) hypersplenism (n=32, 33.3%), immune thrombocytopenic purpura (ITP, n=14, 14.6%), secondary immune thrombocytopenia (n=6, 6.3%), bone marrow aplasia (n=3, 3.1%), and others (n=4, 4.1%). Cardiotocography showed normal results in 94% of cases, a fetal biophysical profile with an index of 8 or 10 in 96.9% and an amniotic fluid index >5.0 cm in 89.6%. Doppler umbilical artery velocimetry showed normal results in 96.9% of cases. In the analysis of the major groups of thrombocytopenia, the diagnosis of oligohydramnios was found to be significantly more frequent in the group with ITP (28.6%) compared to the other groups (gestational thrombocytopenia: 5.4% and hypersplenism: 9.4%, p=0.04). CONCLUSIONS: This study indicates that in pregnancies complicated by moderate or severe maternal thrombocytopenia, even though the fetal well-being remains preserved in most cases, fetal surveillance is important in pregnant women with ITP, with emphasis on amniotic fluid volume evaluation due to its association with oligohydramnios.