Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2023;45(1):38-42
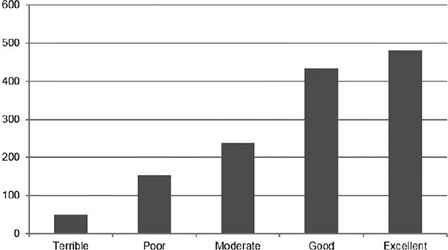
Pain is the primary limitation to performing hysteroscopy. We aimed to evaluate the predictive factors of low tolerance to office hysteroscopic procedures. Methods Retrospective cohort study of the patients who underwent office hysteroscopy from January 2018 to December 2020 at a tertiary care center. Pain tolerance to office-based hysteroscopy was subjectively assessed by the operator as terrible, poor, moderate, good, or excellent. Categorical variables were compared with the use of the Chi-squared test; an independent-samples t-test was conducted to compare continuous variables. Logistic regression was performed to determine the main factors associated with low procedure tolerance.
A total of 1,418 office hysteroscopies were performed. The mean age of the patients was 53 ± 13.8 years; 50.8% of women were menopausal, 17.8% were nulliparous, and 68.7% had a previous vaginal delivery. A total of 42.6% of women were submitted to an operative hysteroscopy. Tolerance was categorized as terrible or poor in 14.9% of hysteroscopies and moderate, good, or excellent in 85.1%. A terrible or poor tolerance was more frequently reported in menopausal women (18.1% vs. 11.7% in premenopausal women, p = 0.001) and women with no previous vaginal delivery (18.8% vs. 12.9% in women with at least one vaginal birth, p = 0.007). Low tolerance led more often to scheduling a second hysteroscopic procedure under anesthesia (56.4% vs. 17.5% in reasonable-to-excellent tolerance, p < 0.0005).
Office hysteroscopy was a well-tolerated procedure in our experience, but menopause and lack of previous vaginal delivery were associated with low tolerance. These patients are more likely to benefit from pain relief measures during office hysteroscopy.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2017;39(7):344-349
To evaluate the trends in definitive contraception in a ten-year interval comprising the years 2002 and 2012.
Retrospective analysis of the tubal sterilization performed in our service in 2002 and2012,analyzingthedemographiccharacteristics,personalhistory,previouscontraceptive method, definite contraception technique, effectiveness and complications.
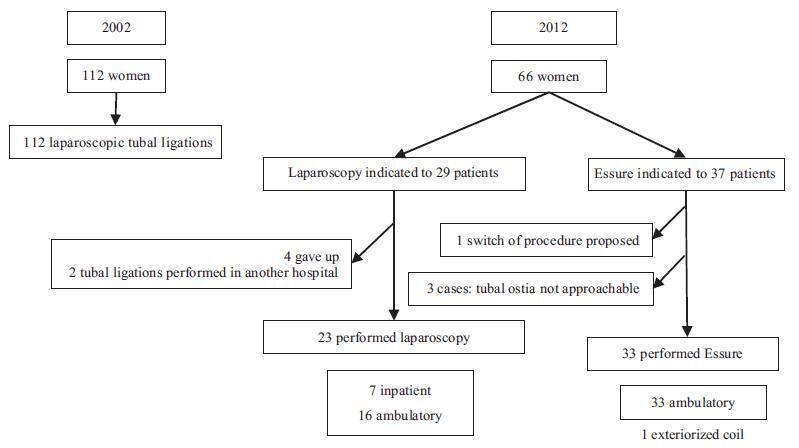
Definitive contraception was performed in 112 women in 2002 (group 1) and in 60 women in 2012 (group 2). The groups were homogeneous regarding age, parity, educational level and personal history. The number of women older than 40 years choosing a definitive method was more frequent in group 1, 49.1% (n = 55); for group 2, the rate was 34.8% (n = 23) (p = 0.04). The time between the last delivery and the procedure was 11.6±6.2 and 7.9±6.4 years (p = 0.014) in 2002 against 2012 respectively. In 2002, all patients performed tubal ligation by laparoscopic inpatient regime. In 2012, the bilateral placement of the Essure (Bayer Corporation, Whippany, NJ, US) device was suggested to 56.1% (n = 37) of the patients, while laparoscopy was suggested to 43.9% (n = 29) of them. All women who underwent laparoscopic sterilization had the procedure successfully completed using silastic rings. The overall bilateral device placement rate for the Essure was 91.6%, with only one complication reported. All Essure procedures were performed in an outpatient setting; for the laparoscopy, this rate was 79% (n = 15). No intentional pregnancies occurred until this date.
There is a trend in the decrease in definitive contraception over the years in our institution, maybe as a result of the development of long-acting reversible contraceptives. The hysteroscopic procedure has become a frequent option, as it is performed in an office setting without anesthesia, being a well-tolerated, minimal invasive method.