Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2021;43(2):107-112
To evaluate the obstetric and sociodemographic characteristics of gestational diabetic women who maintained hyperglycemia in the postpartum period (6-12 weeks postpartum).
This is a longitudinal cohort study with women who have had gestational diabetes and/or macrosomic children between March 1st, 2016 and March 1st, 2017. Between 6 and 12 weeks after birth, women who had gestational diabetes collected fasting glycemia, glucose tolerance test, and glycated hemoglobin results. The data were collected from medical records and during an interview in the first postpartum consultation. A statistical analysis was performed using frequency, percentage, Chi- Squared test, Fisher exact test, Mann-Whitney test, and multivariate Poisson regression. The significance level adopted for the statistical tests was 5%.
One hundred and twenty-two women were included. Most of the women were younger than 35 years old (70.5%), white, multiparous, and with no history of gestational diabetes. Thirteen percent of the participants developed persistent hyperglycemia. A univariate analysis showed that maternal age above 35 years, being overweight, having grade 1 obesity and weight gain under 5 kg was related to the persistence of hyperglycemia in the postpartum period.
Maternal age above 35 years, obesity and overweight, and the diagnosis of gestational diabetes in the first trimester of pregnancy are associated with hyperglycemia during the postpartum period.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2020;42(1):19-25
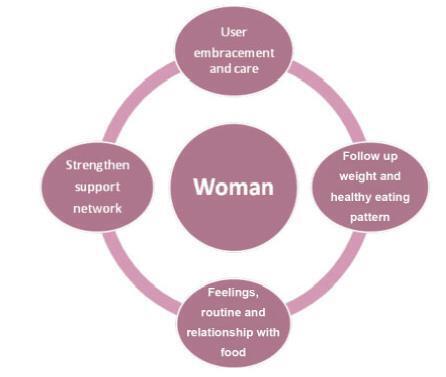
To explore the experiences of women with obesity regarding self-care and the care provided by their families and health team after childbirth.
A clinical qualitative study performed at the Postnatal Outpatient Clinic of Hospital da Mulher, Universidade Estadual de Campinas, Brazil. The sample was selected using the saturation criteria, with 16 women with obesity up to 6 months after childbirth.
The analysis comprised three categories: 1) postnatal self-care; 2) family support for woman after childbirth; and 3) postnatal health care service for women with obesity.
Women with obesity need support from the health team and from their families after childbirth, when they are overwhelmed by the exhausting care for the newborn. The present study reveals how important it is for health care professionals to broaden their perception and care provided after childbirth for women with obesity so they may experience an improvement in their quality of health and of life.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2019;41(12):682-687
The present study aims to understand to what extent obesity is related to adversematernal, obstetrical, and neonatal outcomes in a Portuguese obstetrical population.
A retrospective case-control study was conducted at the Department of Obstetrics of a differentiated perinatal care facility. The study compared 1,183 obese pregnant womenwith 5,399 normal or underweight pregnantwomen for the occurrence of gestational diabetes, hypertensive pregnancy disorders, and preterm birth. Mode of delivery, birthweight, and neonatal intensive care unit (ICU) admissionswere also evaluated. Mean blood glucose values were evaluated and compared between groups, in the first and second trimesters of pregnancy. Only singleton pregnancies were considered.
The prevalence of obesity was 13.6%. Obese pregnant women were significantly more likely to have cesarean sections (adjusted odds ratio [aOR] 2.0, p< 0.001), gestational diabetes (aOR 2.14, p< 0.001), hypertensive pregnancy disorders (aOR 3.43, p< 0.001), and large-for-gestational age ormacrosomic infants (aOR 2.13, p< 0.001), and less likely to have small-for-gestational age newborns (aOR 0.51, p< 0.009). No significant differences were found in terms of pretermbirths, fetal/neonatal deaths, low birthweight newborns, and neonatal ICU admissions among cases and controls. Maternal obesity was significantly associated with higher mean blood glucose levels, in the first and second trimesters of pregnancy.
Obesity is associated with increased risks of adverse pregnancy and neonatal outcomes. These risks seem to increase progressively with increasing body mass index (BMI) class. Female obesity should be considered a major public health issue and has consequences on maternal-fetal health.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2019;41(5):280-290
To evaluate and compare the prevalence of structural congenital anomalies (CAs) according to maternal body mass index (BMI).
The present cross-sectional study involved pregnant women with fetuses diagnosed with structural CAs through morphological ultrasonography between November 2014 and January 2016. The nutritional status of the pregnant women was classified according to the gross value of the body mass index. The pregnant women were categorized into four groups: low weight, adequate weight, overweight, and obesity. Statistical analysis was performed using Stata/SE version 12.0 (Stata Corporation, College Station, TX), with values of p ≤ 0.05 considered statistically significant.
A total of 223 pregnant women had fetuses diagnosed with CAs. The prevalence of structural CAs in pregnant women with lowweight was of 20.18%, of 43.50% in pregnant women with adequate weight, of 22.87% in pregnant women with overweight, and of 13.45% in pregnant women with obesity. The prevalence of central nervous system (CNS) anomalies and of genitourinary systemanomalieswas high for the four groups of pregnant women. A positive association was observed between multiple anomalies in pregnant women with adequate weight (prevalence ratio [PR] = 1.65; p ≤ 0.004) and between anomalies of the lymphatic system in obese pregnant women (PR = 4.04, p ≤ 0.000).
The prevalence of CNS and genitourinary systemanomalies was high in all of the BMI categories. Obese pregnancies were associated with lymphatic system anomalies. Therefore, screening and identification of the risk factors for CAs are important, regardless of the maternal BMI. Our findings reinforce the importance of discussing with pregnant women maternal nutrition and its effect on fetal development and on neonatal outcome.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2018;40(5):251-259
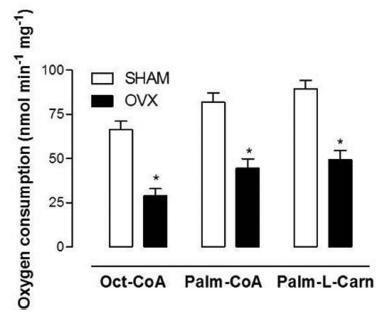
The aim of this work was to evaluate the changes caused by estrogen deficiency in lipid metabolism.
This study encompassed direct measurements of plasma biochemical analyses, liver lipid contents, and assessments of the mitochondrial β-oxidation capacity as well as an evaluation of the liver redox status in an animal model of estrogen deficiency.
When compared with control mice, the livers of ovariectomized (OVX) mice presented considerable accretions in their lipid contents, which were accompanied by increased levels of lipid peroxidation in liver homogenates andmitochondria from OVX groups and decreased reduced glutathione (GSH) contents. In isolated mitochondria, estrogen deficiency inhibited mitochondrial β-oxidation of fatty acids irrespective of their chain length. The liver mitochondrial and peroxisomal H2O2 generations in OVX mice were increased. Additionally, the activities of all antioxidant enzymes assessed were decreased.
These data provide one potential explanation for the increased susceptibility to metabolic diseases observed after menopause.