Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2008;30(12):594-601
DOI 10.1590/S0100-72032008001200002
PURPOSE: to evaluate factors associated with women's dyslipidemia during menopause. METHODS: case-control study of prevalent cases and controls selected from a dedicated outpatient clinic. From recent biochemical parameters found in patients' files, women have been grouped in 'case' and 'control'. Women who presented any alteration in the blood levels of total cholesterol, LDL-cholesterol, triglycerides and/or HDL-cholesterol were considered as case, and the ones who presented normal levels of them, as control. Data concerning socioeconomic situation, physical activity, etilism and tabagism, anthropometric measurements and food ingestion have been collected and then compared between the groups. Ratios have been compared by the χ2, Fisher's exact test and/or t-Student test, depending on the distribution type. The crude relationship between each factor and the presence of dyslipidemia has been estimated by logistic regression. RESULTS: data have been collected from 84 women aged from 42 to 59 years, as 45 of them were grouped as case (dyslipidemic) and 39 as control (non-dyslipidemic). Age average of cases and controls was 52.1±4.2 and 52.2±4.7 years old, respectively. The sample showed to be homogeneous for the socioeconomic characteristics (income, occupation and schooling), physical activity practice, etilism and tabagism, and food ingestion, with no significant correlation with dyslipidemia. The groups presented an income up to two minimal wages, low schooling level (up to the fourth grade of lower school), and the housewife occupation. Smoking and drinking alcohol was not very frequent. Practicing physical activity was non-existent, thus characterizing a sedentary population. Food ingestion was adequate for carbohydrates, protein, lipids, but not for cholesterol (excessive) and fibers (insufficient), in both groups. Concerning the anthropometric evaluation, there has been an association with dyslipidemia, as the body mass index (BMI) and the waist circumference (WC) were significantly larger in case than in control. The waist-hip ratio has been similar in both groups. Weight excess has been found in most of the cases (73.3%) as almost half of them (44%) presented WC >88 cm, which represents a very increased risk. CONCLUSIONS: it is possible to conclude that, in the studied sample, only the anthropometric measurements have been considered as risk factors associated with dyslipidemia, during post-menopause.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2008;30(9):459-465
DOI 10.1590/S0100-72032008000900006
PURPOSE: to evaluate the effect of maternal, socioeconomic and obstetric variables, as well the presence of artery incisions in the 20th and 24th weeks on the fetal weight estimated at the end of pregnancy (36th week) in pregnant women attended by Programa Saúde da Família, in an inland town of the northeast of Brazil. METHODS: a longitudinal study including 137 pregnant women, who have been followed up every four weeks in order to assess clinical, socioeconomic and obstetric conditions, including their weight. The uterine arteries were evaluated by Doppler in the 20th and 24th weeks, the fetal weight and the amniotic fluid index (AFI), determined in the 36th week. The initial maternal nutritional state has been determined by the body mass index (BMI), the pregnant women being classified as low weight, eutrophic, over weight and obese. Weight gain during gestation has been evaluated, according to the initial nutritional state, being classified at the end of the second and third trimester as insufficient, adequate and excessive weight gain. Analysis of variance was performed to evaluate the association of the fetal weight in the 36th week with the predictor variables, adjusted by multiple linear regression. RESULTS: an association between the fetal weight estimated in the 36th week and the mother's age (p=0.02), mother's job (p=0.02), initial nutritional state (p=0.04), weight gain in the second trimester (p=0.01), presence of incisions in the uterine arteries (p=0.02), and AFI (p=0.007) has been observed. The main factors associated to the fetal weight estimated in the 36th week, after the multiple regression analysis were: BMI at the pregnancy onset, weight gain in the second trimester, AFI and tabagism. CONCLUSIONS: in the present study, the fetal weight is positively associated with the initial maternal nutritional state, the weight gain in the second trimester and the volume of amniotic fluid, and negatively, to tabagism.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2007;29(10):511-518
DOI 10.1590/S0100-72032007001000004
PURPOSE: to analyze the association between maternal pre-gestational nutritional status and maternal outcomes - hypertensive disorders of pregnancy, gestational diabetes, vitamin A deficiency, and anemia - and the newborn outcome - low birth weight. METHODS: cross-sectional study, with 433 adult puerperal women (> 20 years old) and their newborns, attending the Maternidade Escola of Universidade Federal do Rio de Janeiro (UFRJ). Data was collected through interviews and access to their medical records. Maternal pre-gestational nutritional status was established through pre-gestational body mass index according to the cut-offs for adult women defined by the World Health Organization (WHO), in 1995. The association between gestational outcomes and pre-gestational nutritional status was estimated through odds ratio (OR) and a 95% confidence interval (95%CI). RESULTS: frequency of pre-gestational weight deviation (low weight, overweight and obesity) was 31.6%. Considering the pre-gestational nutritional status, overweight and obese women presented a lower weight gain than eutrophic and low-weight women (p<0.05). Women with pre-gestational obesity presented a higher risk of developing hypertensive disordens of pregnancy (OR=6.3; 95%CI=1.9-20.5) and those with low pre-gestational weight were more likely to give birth to low birth weigh infants (OR=7.1; 95%CI=1.9-27.5). There was no evidence of the association between pre-gestational nutritional status and the development of anemia, vitamin A deficiency and gestational diabetes. The mean weight gain among overweight and obese pregnant women was significantly lower when compared to eutrophic and low-weight pregnant women (p=0.002, p=0.049, p=0.002, p=0.009). CONCLUSIONS: the high number of women with pre-gestational weight deviation reinforces the importance of a nutritional guidance that favors a good nutritional state and reduces the risks of maternal and newborn adverse outcomes.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2007;29(3):126-133
DOI 10.1590/S0100-72032007000300003
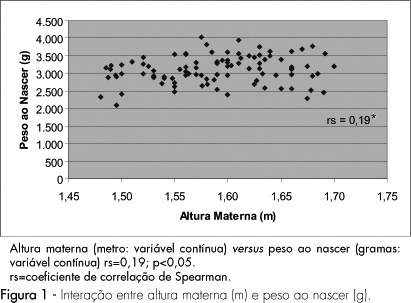
PURPOSE: to evaluate the impact of the nutritional status of pregnant adolescents on the birth weight. METHODS: a cohort study including 97 adolescents and their respective newborns, evaluated from May to June, 2004. Pregnant women from 10 to 19 years old in labor were included in the study, and those with multiple pregnancies, complications, less than 37 weeks gestation, and incomplete data records were excluded. Maternal nutritional status evaluation included height, body mass index (BMI) before pregnancy, gestational weight gain (GWG) and caloric-proteic intake, obtained by habitual food intake recordatory by the end of the third gestational trimester. The association between maternal variables (height, pre-gestational BMI, GWG and intake) and the newborn weight was analyzed by Spearman's correlation test. Statistical significance was assumed when p<0.05. RESULTS: the mean age was 17.8±1.12 years old. Most adolescents (66%) started pregnancy with adequate weight, 29% had low weight and 5% overweight. Most adolescents showed inadequate GWG, caloric and proteic intake. Low birth weight was recorded in 7% of the newborns and insufficient weight was recorded in 37% of them. Maternal height and GWG showed positive and significant BW relation. Pre-gestational BMI and protein intake showed statistically significant inverse correlation with birth weight. No correlation between caloric intake and BW was demonstrated. CONCLUSION: maternal height and GWG influence the newborn nutritional status.