Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2020;42(11):717-725
To compare the type of management (active versus expectant) for preterm premature rupture of membranes (PPROM) between 34 and 36 + 6 weeks of gestation and the associated adverse perinatal outcomes in 2 tertiary hospitals in the southeast of Brazil.
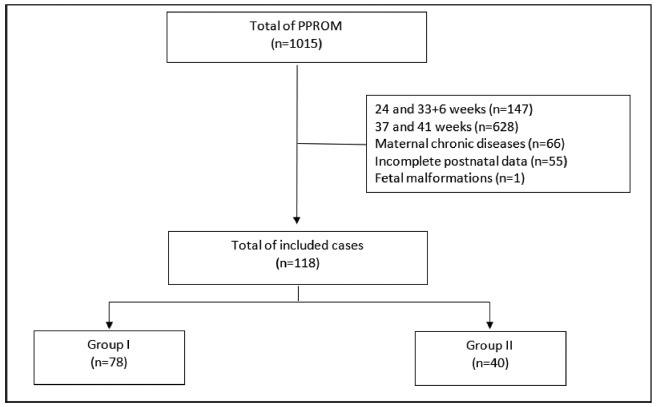
In the present retrospective cohort study, data were obtained by reviewing the medical records of patients admitted to two tertiary centers with different protocols for PPROM management. The participants were divided into two groups based on PPROM management: group I (active) and group II (expectant). For statistical analysis, the Student t-test, the chi-squared test, and binary logistic regression were used.
Of the 118 participants included, 78 underwent active (group I) and 40 expectant management (group II). Compared with group II, group I had significantly lower mean amniotic fluid index (5.5 versus 11.3 cm, p = 0.002), polymerase chain reaction at admission (1.5 versus 5.2 mg/dl, p = 0.002), time of prophylactic antibiotics (5.4 versus 18.4 hours, p < 0.001), latency time (20.9 versus 33.6 hours, p = 0.001), and gestational age at delivery (36.5 versus 37.2 weeks, p = 0.025). There were no significant associations between the groups and the presence of adverse perinatal outcomes. Gestational age at diagnosis was the only significant predictor of adverse composite outcome (x2 [1] = 3.1, p = 0.0001, R2 Nagelkerke = 0.138).
There was no association between active versus expectant management in pregnant women with PPROM between 34 and 36 + 6 weeks of gestation and adverse perinatal outcomes.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2020;42(11):712-716
To determine whether there was any difference in neonatal and maternal outcomes between breech vaginal delivery and cephalic vaginal delivery.
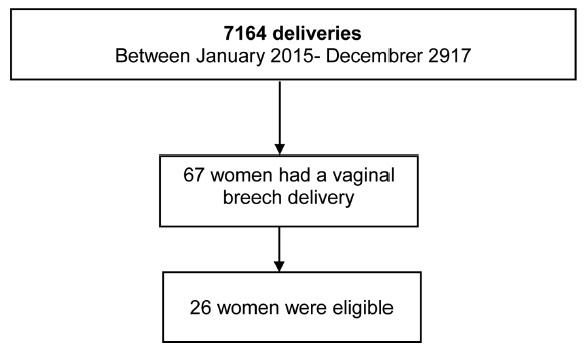
A retrospective, case-control study was conducted between January 2015 and December 2017 in a Portuguese hospital. A total of 26 cases of breech vaginal delivery were considered eligible and 52 pregnant women formed the control group.
Induced labor was more frequent in the breech vaginal delivery group (46% versus 21%, p = 0.022). Episiotomy was more common in the breech vaginal delivery group (80% versus 52%, p = 0.014), and one woman had a 3rd degree perineal laceration. Newborns in the study group had a lower birthweight (2,805 g versus 3,177 g, p < 0.001). There was no significant difference in the neonatal outcomes.
The present study showed that breech vaginal delivery at term compared with cephalic presentation was not associated with significant differences in neonatal and maternal morbidity. It also suggests that breech vaginal delivery remains a safe option under strict selection criteria and in the presence of an experienced obstetrician.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2020;42(1):61-64
Premature delivery often complicates multifetal pregnancies, placing neonates at risk of seriousmorbidity andmortality. In select cases, pretermbirth of one sibling may not require delivery of the remaining fetus(es), which may remain in utero for a delayedinterval delivery, consequently improving neonatalmorbidity andmortality. Currently, there is no consensus on the best protocol for the optimalmanagement of these cases. We report one case of delayed-interval delivery of a dichorionic pregnancy assisted in our center. In this case, prophylactic cerclage, tocolytic therapy and administration of broad-spectrum prophylactic antibiotics enabled delivery at 37 weeks, corresponding to 154 days of latency, which is, to our knowledge, the longest interval described in the literature. The attempt to defer the delivery of the second fetus in peri-viability is an option that should be offered to parents after counseling, providing that the clinical criteria of eligibility are fulfilled. The correct selection of candidates, combined with the correct performance of procedures, as well as fetal and maternal monitoring and early identification of complications increase the probability of success of this type of delivery.