Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2017;39(2):66-71
To investigate the association between the intensity of climacteric symptoms and sexual dysfunction in women aged 40 to 65 years.
Observational, analytic, cross-sectional study conducted with 63 women aged 40 to 65 treated at the gynecology outpatient clinic of a public hospital in northeastern Brazil. A questionnaire was used to collect identification data, clinical information, gynecological-obstetric data, lifestyle traits and information on chronic diseases. Climacteric symptoms and sexual function were evaluated by means of the Blatt-Kupperman index and the Female Sexual Function Index (FSFI) respectively. The association between the two indices was investigated using the chi-squared test; the difference in mean scores on the FSFI as a function of menopausal status was evaluated by Student's t-test. The significance level was set to p < 0.05.
The mean value of the Blatt-Kupperman index was 26.42 (standard deviation [SD]: 4.52); 36.51% of the women exhibited severe symptoms. The mean score on the FSFI was 21.84 (SD: 4.11). More than half of the analyzed women (58.73%) exhibited sexual dysfunction (FSFI ≤ 26.5). Regarding the association between the Blatt- Kupperman index and the FSFI, the greater the intensity of the climacteric symptoms (Blatt-Kupperman), the higher the frequency of sexual dysfunction (FSFI). Sexual dysfunction was exhibited by 100% of the participants with severe climacteric symptoms, 70.59% of those with moderate symptoms, and only 9.09% with mild symptoms (p < 0.001).
The application of the Blatt-Kupperman index and of the FSFI allowed the detection of an association between the severity of climacteric symptoms and the prevalence of sexual dysfunction.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2016;38(7):317-324
Cardiovascular disease (CVD) is the leading cause of death in post menopausal women, and inflammation is involved in the atherosclerosis process.
to assess whether dietary pattern, metabolic profile, body composition and physical activity are associated with low-grade chronic inflammation according to highsensitivity C-reactive protein (hs-CRP) levels in postmenopausal women.
ninety-five postmenopausal participants, with no evidence of clinical disease, underwent anthropometric, metabolic and hormonal assessments. Usual dietary intake was assessed with a validated food frequency questionnaire, habitual physical activity was measured with a digital pedometer, and body composition was estimated by bioelectrical impedance analysis. Patients with hs-CRP ≥ 10 mg/L or using hormone therapy in the last three months before the study were excluded from the analysis. Participants were stratified according to hs-CRP lower or ≥3 mg/L. Sedentary lifestyle was defined as walking fewer than 6 thousand steps a day. Two-tailed Student's t-test, Wilcoxon-Mann-Whitney U or Chi-square (x 2) test were used to compare differences between groups. A logistic regression model was used to estimate the odds ratio of variables for high hs-CRP.
participants with hs-CRP ≥ 3 mg/L had higher body mass index (BMI), body fat percentage, waist circumference (WC), triglycerides, glucose, and homeostasis model assessment of insulin resistance (HOMA-IR) (p = 0.01 for all variables) than women with hs-CRP <3 mg/L. Also, women with hs-CRP ≥3 mg/L had a higher glycemic load diet and lower protein intake. Prevalence of sedentary lifestyle (p < 0.01) and metabolic syndrome (p < 0.01) was higher in women with hs-CRP ≥3 mg/L. After adjustment for age and time since menopause, the odds ratio for hs- CRP ≥3 mg/L was higher for sedentary lifestyle (4.7, 95% confidence interval [95%CI] 1.4-15.5) and carbohydrate intake (2.9, 95%CI 1.1-7.7).
sedentary lifestyle and high-carbohydrate intake were associated with low-grade chronic inflammation and cardiovascular risk in postmenopause.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2016;38(6):266-272
Some studies have investigated the influence of hormonal deficits and menopausal status in muscle disorders of women. However, it has not been investigated the relationship of both climacteric symptoms and the perception of quality of life with physical performance.
To evaluate the correlation of menopausal symptoms and quality of life with physical performance in middle-aged women.
This cross-sectional study was performed from April to November 2013 in the municipality of Parnamirim, in the Brazilian state, Rio Grande do Norte. The sample was composed of 497 women aged 40-65 years. The Menopause Rating Scale (MRS) and the Utian Quality of Life (UQOL) questionnaire were used to evaluate menopausal symptoms and quality of life respectively. Measures of physical performance included handgrip strength, knee extensor and flexor strengths (using an isometric dynamometer), gait speed, and chair stand test. The correlation between menopausal symptoms and quality of life with physical performance was assessed by Pearson's correlation coefficient with significance set at p< 0.05 and a confidence interval of 95 %.
There was a significant negative correlation between handgrip strength and somatic MRS score (p= 0.002) and total MRS score (p= 0.03). There was a significant correlation between knee flexor strength and sit-to-stand time and all menopausal symptom areas (p< 0.05), except psychological symptoms. There was a positive correlation between physical performance of the knee flexors and quality of life items including occupational (p= 0.001), emotional (p= 0.005), and total UQOL (p= 0.01) , but a negative correlation with sit-to-stand time and all quality of life domains (p< 0.05).
A greater intensity of menopausal symptoms and worse quality of life were related with worse physical performance. Thus, preventive measures should be implemented to avoid adverse effects on physical performance at more advanced ages.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2016;38(5):210-217
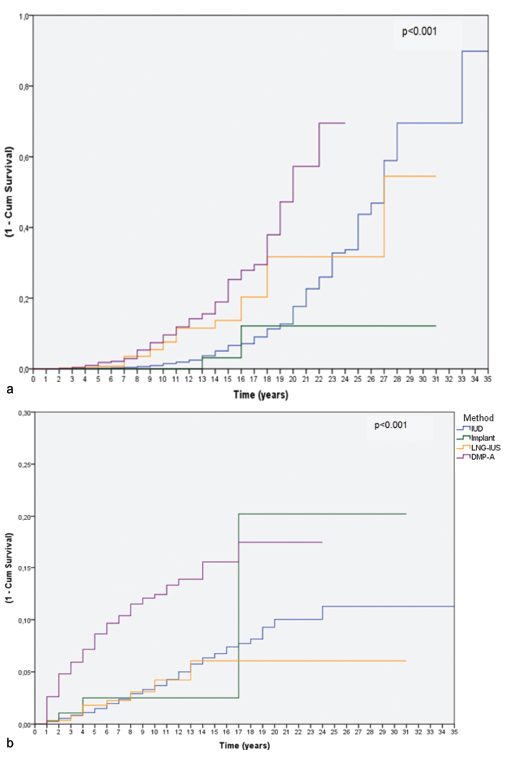
Women require effective contraception until they reach menopause. The long acting reversible contraceptives (LARC) and the depot-medroxyprogesterone acetate (DMPA, Depo-Provera(r), Pfizer, Puurs, Belgium) are great options and can replace possible sterilizations.
To assess the relationship between the use of LARCs and DMPA and terminations ascribed to menopause and sterilizations in a Brazilian clinic.
We reviewed the records of women between 12 and 50 years of age attending the clinic that chose to use a LARC method or DMPA. Cumulative termination rates due to sterilization or because the woman had reached menopause were computed using single decrement life-table analysis over 32 years. We also examined all records of surgical sterilization at our hospital between the years 1980-2012.
Three hundred thirty-two women had continuously used the same contraceptive until menopause, and 555 women had discontinued the method because they or their partners underwent sterilization. From year 20 to year 30 of use, levonorgestrel intrauterine-releasing system (LNG-IUS - Mirena(r), Bayer Oy, Turku, Finland; available since 1980), copper intrauterine device (IUD - available since 1980) and DMPA users showed a trend of cumulative higher discontinuation rates due to menopause when compared with the discontinuation rates due to sterilization. Over the study period, a steep decline in the use of sterilization occurred.
Over the past 15 years of research we have observed a trend: women usually preferred to continue using LARC methods or DMPA until menopause rather than decide for sterilization, be it their own, or their partners'. The annual number of sterilizations dropped in the same period. The use of LARC methods and DMPA until menopause is an important option to avoid sterilization, which requires a surgical procedure with potential complications.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2016;38(3):140-146
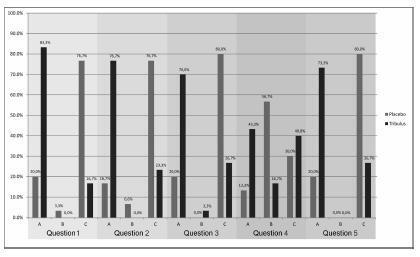
The aim of this study was to study the effects of Tribulus terrestris on sexual function in menopausal women.
This was a prospective, randomized, double-blind, placebo-controlled clinical trial that included 60 postmenopausal women with sexual dysfunction. The women were divided into two groups, placebo group and Tribulus group, and evaluated by using the Sexual Quotient-female version (SQ-F) and Female Intervention Efficacy Index (FIEI) questionnaires.
There was no significant difference between the groups in age, age at menopause, civil status, race, and religion. In the evaluation with the SQ-F questionnaire, there were significant differences between the placebo (7.6±3.2) and Tribulus (10.2±3.2) groups in the domains of desire and sexual interest (p d" 0.001), foreplay (3.3±1.5 versus 4.2±1.0) (p d" 0.01), arousal and harmonious interaction with the partner (5.7±2.1 versus 7.2±2.6) (p d" 0.01), and comfort in sexual intercourse (6.5±2.4 versus 8.0±1.9) (p d" 0.01). There was no significant difference between the placebo and Tribulus groups in the domains of orgasm and sexual satisfaction (p = 0.28). In the FIEI questionnaire, there was a significant improvement (p < 0.001) in the domains of vaginal lubrication during coitus and/or foreplay (20 versus 83.3%), sensation in the genitalia during sexual intercourse or other stimuli (16.7 versus 76.7%), sensation in the genital region (20 versus 70%), sexual intercourse and/or other sexual stimulations (13.3 versus 43.3%), and the ability to reach orgasm (20% versus 73.3%). There was no significant difference in adverse effects between the two groups.
After 90 days of treatment, at the doses used, we found Tribulus terrestris to be effective in treating sexual problems among menopausal women.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2015;37(4):152-158
DOI 10.1590/SO100-720320150005282
To determine the average age at the onset of menopause and to investigate menopausal symptoms in women in a metropolitan region in Southeastern Brazil.
A descriptive, exploratory, cross-sectional study was conducted with 749 women (a population-based household survey). The dependent variable was the intensity of menopausal symptoms assessed by th Menopause Rating Scale (MRS). The independent variables were sociodemographic data, health-related habits and problems, self-perception of health, and gynecological background. Statistical analysis was carried out by the χ2 test and Poisson regression using the backward selection criteria.
The mean age of the women was 52.5 (±4.4) years. With regard to menopausal status, 16% were premenopausal, 16% perimenopausal and 68% postmenopausal. The mean age at the onset of menopause was 46.5 (±5.8) years. The intensity of menopausal symptoms was defined according to the median MRS score and was considered severe for values above 8. Depression/anxiety (PR=1.8; 95%CI 1.5-2.2; p<0.01), rheumatic diseases (PR 1.5; 95%CI 1.2-1.7; p<0.01), self-perception of health as fair/poor/very poor (PR 1.4; 95% CI 1.2-1.7; p<0.01), history of abortion (PR 1.3; 95%CI 1.1-1.4; p<0.01), current or previous treatment for menopausal symptoms (PR 1.2; 95%CI 1.1-1.4; p<0.01), peri- or postmenopausal status (PR 1.4; 95%CI 1.1-1.7; p<0.01), number of normal deliveries >1 (PR 1.2; 95%CI 1.02-1.4; p<0.01) and asthma (PR 1.2; 95%CI 1.01-1.4; p<0.01) were associated with more severe menopausal symptoms. Older age (PR 0.96; 95%CI 0.96-0.97; p<0.01) was associated with less severe symptoms.
The severity of menopausal symptoms was related to a wild range of factors, especially presence of chronic diseases, a larger number of pregnancies, use of hormone therapy, and worse self-rated health. A better understanding of these factors can help to reduce the impact of symptoms on quality of life, and to identify groups of women who are likely to need more care during and beyond menopause.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2014;36(10):467-472
DOI 10.1590/SO100-720320140005094
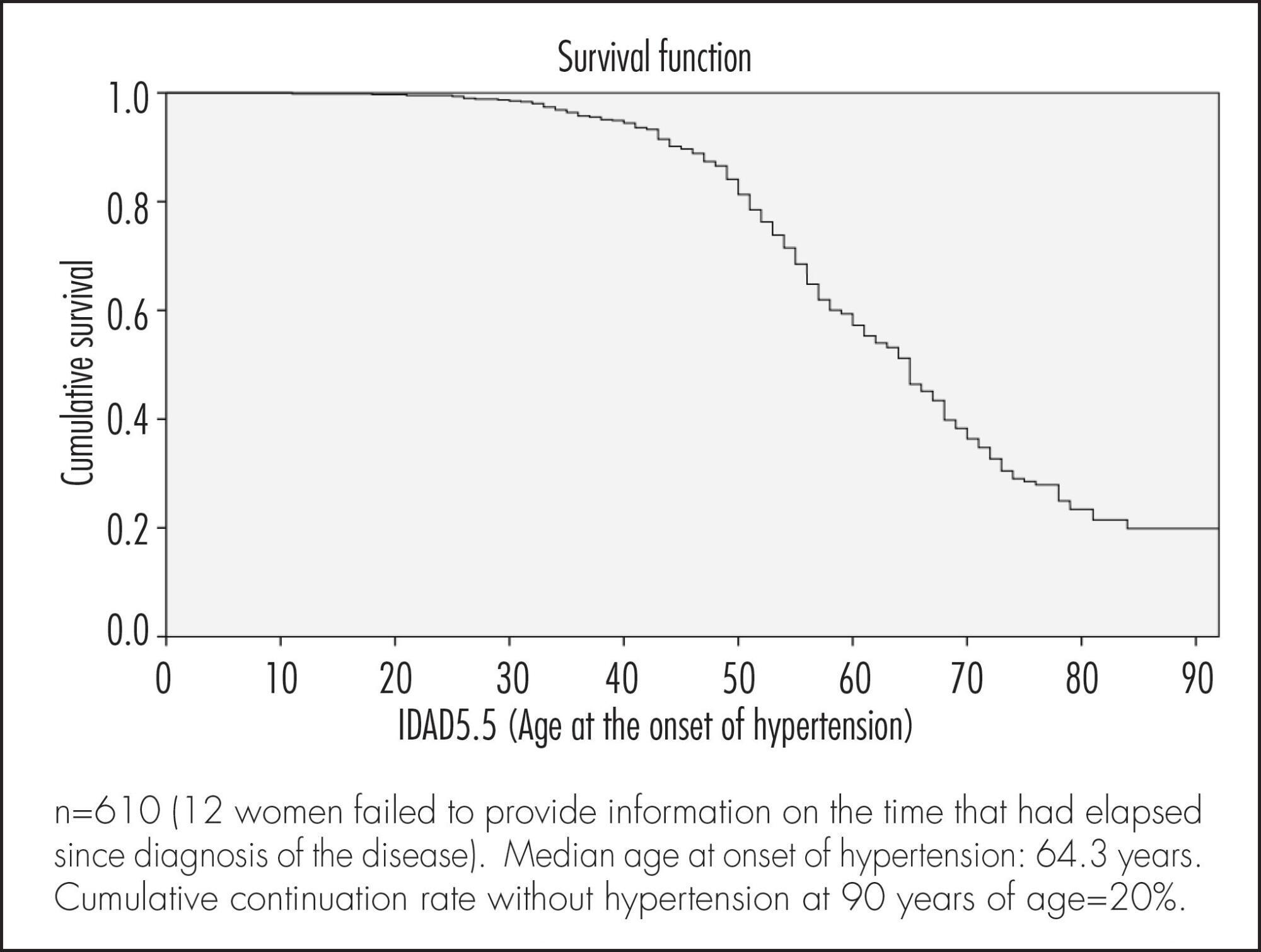
To evaluate factors associated with hypertension in Brazilian women of 50 years of age or more.
A cross-sectional population based study using self-reports. A total of 622 women were included. The association between sociodemographic, clinical and behavioral factors and the woman's age at the onset of hypertension was evaluated. Data were analyzed according to cumulative continuation rates without hypertension, using the life-table method and considering annual intervals. Next, a Cox multiple regression analysis model was adjusted to analyze the occurrence rates of hypertension according to various predictor variables. Significance level was pre-established at 5% (95% confidence level) and the sampling plan (primary sampling unit) was taken into consideration.
Median age at onset of hypertension was 64.3 years. Cumulative continuation rate without hypertension at 90 years was 20%. Higher body mass index (BMI) at 20–30 years of age was associated with a higher cumulative occurrence rate of hypertension over time (coefficient=0.078; p<0.001). Being white was associated with a lower cumulative occurrence rate of hypertension over time (coefficient= -0.439; p=0.003), while smoking >15 cigarettes/day was associated with a higher rate over time (coefficient=0.485; p=0.004).
The results of the present study highlight the importance of weight control in young adulthood and of avoiding smoking in preventing hypertension in women aged ≥50 years.