Summary
Revista Brasileira de Ginecologia e Obstetrícia. 1999;21(6):341-345
DOI 10.1590/S0100-72031999000600007
Objectives: to analyze the medical and legal aspects in order to contribute to the study and standardization of this obstetrical surgery in Brazil. Methods: our study was based on 11 cases of cesarean section performed in the imminence of maternal death or just after death. These cases were attended at UNIFESP - EPM from 1988 to 1998. Results: there were 7 live births, five of them with a gestational age over 26 weeks. Most deaths occurred within the first 48 hours after admission. The predominant age range was the third decade. Conclusions: although postmortem cesarean section is indicated to save the fetus, it is rarely performed. The conditions for its indication involve knowledge of the technique as well as of the ethical and legal principles.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2005;27(9):548-553
DOI 10.1590/S0100-72032005000900008
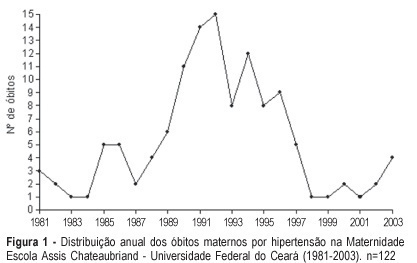
PURPOSE: to study maternal mortality caused by hypertension during pregnancy, determining the mortality rate and the profile of those patients. METHODS: a retrospective study of maternal mortality caused by hypertension at the Maternidade Escola Assis Chateaubriand of the Universidade Federal do Ceará, from 1981 to 2003. General maternal mortality rate (MMR) and specific maternal mortality rate due to hypertension were evaluated, as well as these patients' epidemiological and clinical data. RESULTS: two hundred and ninety six cases of maternal death and 184,672 of live births were recorded, with a MMR of 160.28/100.000 live births. The most frequent cause of death was hypertension (41.2%); with 122 cases and an annual average of 5.3 deaths, and hypertension MMR of 60.10/100,000 live births. The women's age range varied from 13 to 42 years with an average of 26 years. Most of the patients came from the interior of the state. Deaths occurred predominantly in the first 24 hours after admission to the hospital (50.9%). Deaths were predominant in the first pregnancy (40.3%) and in women with 31 to 38 weeks gestational age (48.2%). Eclampsia occurred in 73 patients (64.1%) and was predominant along the gestational period (53.4%). There were 101 deaths in the puerperium. Cesarean section (62.3%) and general anesthesia (45.1%) prevailed. A high percentage of patients (61.4%) had no prenatal care. CONCLUSIONS: General MMR and hypertension MMR were high, the latter being the main cause of death in our maternity hospital.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2005;27(10):627-634
DOI 10.1590/S0100-72032005001000010
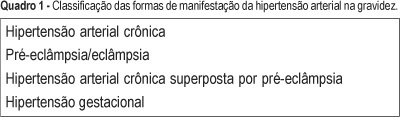
Arterial hypertension is one of the most frequent causes of maternal death. The most important types found in pregnancy are gestational hypertension, clinically defined by increased arterial pressure after the 20th week of pregnancy, and preeclampsia associated with proteinuria. In the initial phase, the disease is asymptomatic, but when not treated or when the pregnancy is not interrupted, it naturally progresses to serious forms such as eclampsia and HELLP syndrome. Eclampsia is defined by one or more generalized tonic-clonic seizures or coma in a pregnant woman with gestational hypertension or preeclampsia, and without neurological disease. It may occur during pregnancy, labor, and immediately after delivery. It is often preceded by signs and symptoms of imminent eclampsia (central nervous system, visual and gastric disorders). Its association with hemolysis, low platelet count, and hepatic dysfunction had already been reported in the literature of the 1950's. In 1982, Weinstein grouped these alterations as a syndrome under the acronym of HELLP, meaning hemolysis (H), elevated liver enzyme levels (EL), and low platelet (LP) count. The literature differs in relation to the parameter values that define the syndrome. Sibai et al. (1986) proposed a system of laboratory and biochemical diagnosis standards which has been adopted by the Brazilian Health Ministry. Clinical manifestations are sometimes imprecise; common complaints are epigastric pain, general malaise, loss of appetite, nausea, and vomiting. Early diagnosis is exclusively by laboratory tests and should be systematically investigated in women with serious preeclampsia/eclampsia or pain in the superior right abdominal quadrant. Differentiating HELLP syndrome from others with similar clinical or laboratory manifestations is not easy. Differential diagnosis is particularly difficult regarding diseases such as thrombotic thrombocytopenic purpura, hemolytic-uremic syndrome, or acute fatty liver of pregnancy, due to poor clinical history, and similar physiopathological aspects. An understanding of preeclampsia physiopathology, early diagnosis, and precise action at the right moment in situations complicated by eclampsia or HELLP syndrome, allows a better maternal and perinatal prognosis.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2005;27(6):357-365
DOI 10.1590/S0100-72032005000600011
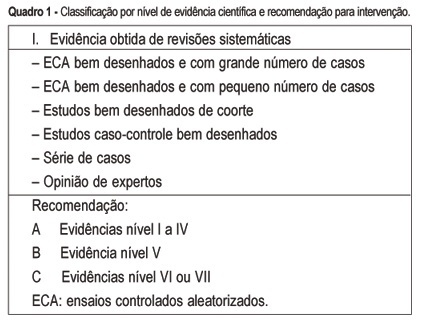
The multiple factors involved in maternal complications and maternal mortality make the task of their long-term control difficult and time-consuming. Professional care for pregnant women and/or those in labor certainly represents a key point for obtaining good outcomes, either maternal or perinatal. From the starting point that an adequate professional medical care for delivery has the capacity of decreasing the occurrence of complications associated with maternal morbidity and mortality, the evidence regarding some interventions included in this care is summarily presented. The evidence derived from studies performed with a strong methodological and scientific approach, mainly randomized controlled trials, on interventions to reduce complications and maternal mortality. These main interventions basically refer to: institutional care to is focused delivery, skilled professional care, use of traditional birth attendants in some contexts, use of appropriate technologies including partograph, place of birth, position for delivery, use of episiotomy, type of delivery, use of oxytocin during the active phase of labor, performance of push efforts during the second stage, active management of the third stage, and prophylaxis for post-partum hemorrhage. Although the effect of avoiding maternal death is difficult to be evaluated due to its low frequency, its rational and standardized use, through manuals and guidelines for intervention care, has a positive effect on the quality of care for childbirth. This is part of the human and technical context of the right that every woman has to the best possible care in this so special moment of her life.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2000;22(1):27-32
DOI 10.1590/S0100-72032000000100005
Purpose: to identify and quantify the underreporting of maternal mortality, from death certificates (DC) in Campinas, São Paulo, from 1992 to 1994. Methods: a total of 216 DC whose causes of death were maternal (declared and/or presumed) were selected among the 1032 DC of 10 to 49-year-old women. A complementary investigation was performed on hospital records, at the death verifying units, and in households. Results: eight additional maternal deaths were identified among the 204 DC with presumed maternal death. This corresponded to an underreporting rate of 40% or to a correction factor of 1.67 for the official MMR. The first cause of underreporting was abortion (71.5% or 05/07) and indirect maternal deaths represented the second cause (66.6% or 02/03). Conclusions: the death certificate cannot be considered the only source to identify maternal death. Complementary investigation of the presumable causes of maternal death should be performed. Legislation, social and religious factors might influence the underreporting of abortion as the cause of maternal death.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2000;22(1):13-17
DOI 10.1590/S0100-72032000000100003
Purpose: to determine magnesium sulfate effectiveness to prevent eclamptic seizures in pregnant women diagnosed with preeclampsia. Methods: a case-control study involving 489 pregnant patients admitted to the Hospital de Clínicas de Porto Alegre (HCPA) with the diagnosis of hypertension between January 1990 and January 1997. The patients were divided into two groups: those who received magnesium sulfate (Group I) and those who did not (Group II). All patients were treated according to the hospital's standard protocol for the treatment of hypertensive pregnant women. The following variables were assessed: maternal age, race, number of seizures, number of seizures in patients receiving magnesium sulfate, period of magnesium sulfate administration, before and after delivery, maternal mortality, need of ICU care, need of mechanical ventilation and length of hospital stay after delivery. Data were assessed with Epi-Info 6.0 statistical package, using multivariate analysis. The main outcome measure was magnesium sulfate use. Results: no differences were found between the two groups in terms of maternal age, race or gestational age. Women who received magnesium sulfate had a higher mean systolic and diastolic blood pressure. Women in the intervention group had a longer hospital stay and a greater need of ICU care. Need of mechanical ventilation and maternal mortality were similar in the two groups. Twenty-two out of 353 women had one or more seizures before admission to the hospital. Six women (27.3%) had one or two additional seizures after magnesium sulfate administration. No subjects had three or more seizures after receiving magnesium sulfate. Conclusion: the results show that eclamptic seizures can be prevented by routine prophylactic magnesium sulfate administration.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2005;27(4):197-203
DOI 10.1590/S0100-72032005000400006
PURPOSE: to apply a severity score to cases of severe maternal morbidity (SMM) and to compare the classification criteria. METHODS: a control-case study was performed as a secondary analysis of cases of SMM in a tertiary level maternity unit for a period of 12-month. A specific score for assessing the degree of severity was applied to cases identified as SMM. Twenty cases of near miss maternal morbidity (higher severity) were compared to 104 control cases (lower severity) of other severe morbidities, regarding risk factors, primary determinants and assistance requirements. Analyses were performed with means and proportions, using Student's t, Wilcoxon and chi2 statistical tests, and estimations of OR and 95% CI. RESULTS: the higher severity (near miss) was identified in 16.1% of cases and the history of abortion was the only factor statistically associated with it (OR=3.41, 95% CI 1.08-10.79). In fact, the indices of assistance complexity were more frequent in the near-miss morbidity group, which also presented less hypertension (30% against 62.5%) and more hemorrhage (35.5% against 10.6%) as primary determinant factors of severe morbidity. CONCLUSIONS: the higher severity of maternal morbidity was associated with a history of abortion and with hemorrhage as a cause. The applied score was able to identify a higher severity subgroup (near miss), which needs more complex professional and institutional care in order to avoid the occurrence of death.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2004;26(2):89-96
DOI 10.1590/S0100-72032004000200002
PURPOSE: to evaluate knowledge, opinion and practice of gynecologists/obstetricians regarding induction of abortion. Method: a pretested, structured questionnaire was sent to gynecologists/obstetricians affiliated to FEBRASGO. They were asked to answer and return the questionnaire in a self-addressed, prepaid envelope, without identification of the respondent so as to preserve anonymity. Knowledge about the legal situation of abortion in Brazil, opinion about it and practice if confronted with abortion requests were questioned. RESULTS: approximately 90% of the respondents believed that abortion is legal for pregnancy resulting from rape or in case of risk to a woman's life and for 31.8% in case of severe fetal malformation. In their opinion abortion should be permitted in the case that pregnancy is a risk for a woman's life (79.3%), fetal malformation (77.0%) and after rape (76.6%), added to 9.9% who expressed that abortion should be permitted in all circumstances. Two thirds wrongly thought that a judicial order is required to practice a legal abortion and only 27.4% knew that a written request by the woman is required. Confronted with unwanted pregnancy, 77.6% of female gynecologists/obstetricians and 79.9% of partners of male respondents had an abortion, 40% would help a client and 48.5% a relative in the same situation. CONCLUSION: gynecologists/obstetricians lack knowledge on the legal situation of abortion although their opinion and practice are favorable.