Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2007;29(3):120-125
DOI 10.1590/S0100-72032007000300002
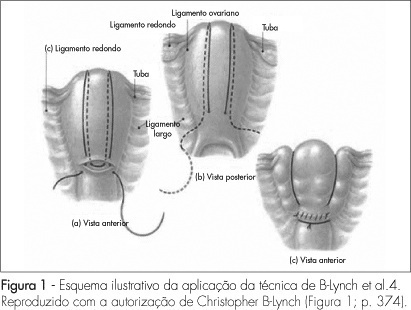
PURPOSE: to present a surgical technique for patients submitted to caesarean section, which evolves to medicine refractory hemorrhage. METHODS: a case report study, of which the including criteria were failure in the pharmacological treatment to control post-partum hemorrhage, and the patients' request to preserve their uterus. Four patients submitted to caesarean section which evolved to immediate post-partum hemorrhage, refractory to the use of ocytocin, ergometrine and misoprostol, were treated with the suture technique described by B-Lynch, without modification. The uterus was transfixed in six points according to the standard procedure, with chrome catgut-2 or polyglactine-1thread. After the assistant's manual compression of the uterus, the thread was pulled by its extremities by the surgeon, and a double knot followed by two simple knots were applied before performing the hysterorraphy. RESULTS: needled chrome catgut-2 thread was used in three cases and needled poluglactine-1 in one case. In the four cases there was immediate discontinuity of the vaginal bleeding, after the suture. The four patients did not present any complication during the procedure or along the immediate and late puerperal period. CONCLUSION: this technique represents a surgical alternative to deal with post-partum hemorrhage and may represent a reduction in the maternal morbidity and mortality in our country.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 1998;20(1):7-11
DOI 10.1590/S0100-72031998000100002
With the purpose of identifying the causes of maternal deaths, this study evaluated all cases of deaths of 10 to 49-years-old women which occurred in Recife, Pernambuco, Brazil, during 1992 and 1993. The data were obtained from 1013 death certificates and were complemented by medical and anesthetia records forms, nursing reports, necropsies and also interviews with physicians who took care of the women, or with their relatives. The main basic causes of maternal deaths identified were arterial hypertension (23.8%), infections (19.0%), abortion (11.9%), hemorrhage (9.5%), pulmonary embolism (4.8%) and anaesthetic accident (2.4%). About 70% of maternal deaths in Recife in the studied period were due to directo obstetrical causes.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 1998;20(1):13-18
DOI 10.1590/S0100-72031998000100003
The parpose of the present report was to determine the maternal mortality rate in São Paulo, the most frequent pathologies which caused death and the distribution of cases paccording to age. In thepresent retrospective study 179,872 death certificates from April 1993 to December 1995 of women from 10 to 49 years old. Were reviewed 761 death certificates were selected, in which the pregnancy state was either declared or presumed; pregnancy was confirmed in 291/761 cases and 53/761 cases are still under investigation. The data were tabulated, grouped and analyzed considering the age and cause of death, according to the 9th revised edition of ICD - International Classification of Diseases. Of the 291 positive cases, 82 (28.17%) did not show any reference to the pregnancy state in the death certificate (undernotification); 183/291 cases (62.89%) were direct maternal deaths and the main diseases leading to maternal death were: hemorrhage (47/183), preeclampsia-eclampsia (46/183) and abortion complications (43/183). Among the indirectly related causes of maternal death (79/291), cardiopaty was the most frequent (33/79). Hypertensive syndrome (preeclampsia-eclampsia and/or chronic arterial hypertension) were responsible for 58/291 cases (19.93%) of maternal deaths. This study allowed us to calculate the maternal mortality rate for São Paulo: 50.24:100,000 live births.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 1998;20(4):181-185
DOI 10.1590/S0100-72031998000400002
With the purpose of identifying the social, demographic, pregnancy-related and medical care factors associated with maternal death, this study evaluated all deaths of women aged 10 to 49 years occurring in Recife, Pernambuco, Brazil, during 1992 and 1993. The data were obtained reviewing 1,013 death certificates, with 42 cases of identified maternal deaths. The data of these deaths were complemented with information from medical records, autopsies and also interviews with physicians from the hospitals where the death took place, and with the dead women's relatives. Almost two thirds (62%) of maternal deaths occurred among women aged 20 to 29 years and more than half of them were single. There was a higher number of deaths among caesarean deliveries than among vaginal ones. The majority of deaths occurred within the first three days of hospitalization and approximately 90% of hospital charges were sponsored by the National Health System (SUS).
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 1998;20(7):395-403
DOI 10.1590/S0100-72031998000700005
Purpose: to establish a list of diseases promoting maternal death according to frequency. Methods: In 1996, 65,406 deaths were recorded in the City of São Paulo, 26,778 of which were of women. Of these, 4591 were within the 10-49 year age bracket. We analyzed the latter group, regarding at the field "Cause of Death" in the Death Certificate, trying to establish some correlation between the described pathology, and the pregnancy-puerperium cycle. We separated for a further study 293 Death Certificates, from which we selected, after hospital survey and/or home visits, a total of 119 positive cases for maternal death. The positive cases for maternal death were then tabulated, grouped and analyzed according to age and pathology, using the great medical care groups. Results: as regards the 119 positive cases for maternal death, we did not find any reference to the pregnancy-puerperium state in 53 of them (that is, 40.54% subnotifying). The cases were grouped according to pathology, where we found a predominance of eclampsia/pre-eclampsia cases (18.02%), followed by cases resulting from hemorrhagic complications in the third quarter and puerperium (12.61%), abortion complications (12.61%), puerperal infection (9.91%) and cardiopathies (9.91%). Conclusions: for the first time, we are publishing the Late Maternal Mortality Coefficient for the City of São Paulo, which was 51.33/100,000 born alive. However, we used for the official publication the Maternal Mortality Coefficient for death within up to 42 days of puerperium, which was, 48.03/100,000 born alive for the city of São Paulo. We should bear in mind that no correction factor should be applied to these figures since we have made an active search of cases.
Summary
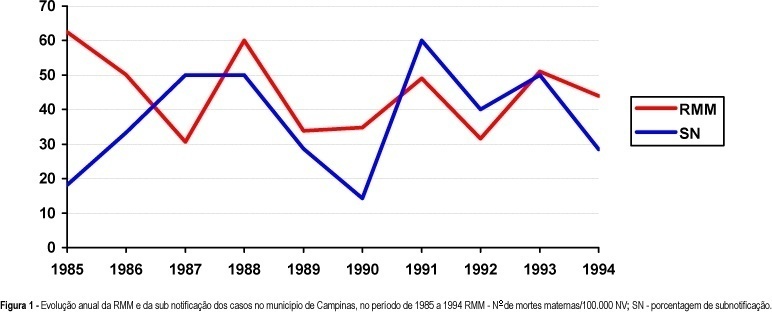
Revista Brasileira de Ginecologia e Obstetrícia. 1999;21(4):227-232
DOI 10.1590/S0100-72031999000400008
Purpose: to identify and investigate the causes of maternal death that occurred in Campinas from 1992 to 1994. Methods: a total of 204 death certificates (DC) whose causes of death were maternal (declared and/or presumed) were selected among the 1032 DC's of 10 to 49 year-old women. A complementary investigation was performed consulting hospital records, Death Survey Units, and households. Results: a total of 20 maternal deaths were confirmed, corresponding to a maternal mortality ratio of 42.2 deaths per 100,000 live births. The direct obstetrical causes were responsible for 85% of the deaths (17 cases). Abortion complications were the main causes of death (7 cases), followed by hemorrhage (4 cases), preeclampsia (3 cases) and puerperal infection (3 cases). Conclusions: despite the apparent progress concerning the reduction in deaths due to hypertensive syndromes during pregnancy, that were the main causes in earlier periods, there was no improvement in the maternal mortality ratio for this studied period. Unfortunately, this lack of progress was due to abortion complications. A better coverage and efficiency of family planning programs, besides the need for implementation of a real epidemiological surveillance of maternal deaths, as well as a better social protection of the pregnant woman, the mother, and the newborns, could reduce their occurrence and specially those due to abortions.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2006;28(7):380-387
DOI 10.1590/S0100-72032006000700002
PURPOSE: to evaluate all maternal deaths that occurred between 1927 and 2001, among 164,161 patients admitted to the Maternidade Therezinha de Jesus, the obstetrical service of the "Universidade Federal de Juiz de Fora", Brazil. METHODS: a retrospective study of 144 maternal deaths that occurred in the maternity hospital in 75 years, with 131,048 live births in the same period of time, analyzing all patients's records regarding their clinical history and data from death certificates. Autopsies were not performed. Data obtained were age, parity, gestation length, complications, moment, and causes of death. The index of maternal mortality (IMM) period 100 thousand live births was utilized. For statistical analysis the chi2 test and the exponential smoothing technique were used (alpha=0.05). RESULTS: IMM decreased from 1544 in the period 1927-1941 to 314 (p<0.001) between 1942 and 1956 and from 1957 to 1971 it was reduced to 76.4 per 100 thousand live births (p<0.001). Nevertheless, since 1972 there was no further significant improvement (IMM=46 in the last 15 years, p=0.139). Maternal mortality was more frequent in the 15 to 39 years age group, in nulliparous patients with term pregnancies and mostly in the immediate postpartum period (53%). Direct obstetric causes occurred in 79.3% and indirect causes in 20.7% of the cases. Analyzing the evolution of the causes of death, it was found that in the first period of time the most frequent direct obstetric causes in descending order were puerperal infection, eclampsia and uterine rupture, while in the second period they were prepartum hemorrhage and eclampsia, and from 1977 to 2001 hemorrhage, abortion and preeclampsia. Analysis of the past 15 years showed the absence of maternal deaths by either preeclampsia or puerperal infection and the main causes were peripartum hemorrhage, abortion and indirect obstetrical causes. Relating maternal mortality to the type of delivery by the relative risk between cesarean section and vaginal delivery, it was found that when the indication of cesarean section is inevitable its risk is lower (relative risk = 0.6) than through vaginal delivery. CONCLUSIONS: despite the reduction along the 75 years of study, maternal mortality of 46 per 100,000 live births is still very high, and there was no significant decrease since 1972. Many deaths are avoidable. Hemorrhage is at present the most frequent cause of maternal death, the decision to intervene should be fast, and a proper indication for a cesarean section is a safe option. Maternal mortality caused by abortion is increasing alarmingly and family planning is essential.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2006;28(5):310-315
DOI 10.1590/S0100-72032006000500008
Maternal mortality rate (MM) is a health quality indicator that is directly influenced by the economic, cultural and technological level of a country. Official data of MM in Brazil, although underestimated, point to the lack of quality in pregnancy, childbirth and puerperium care services. This characteristic is common in developing countries, where poorer pregnant women as well as those facing greater difficulty to quality care access are found. Prenatal care cannot prevent major childbirth complications, which are important causes of MM; however, some interventions during the prenatal period can favor maternal prognosis and prevent MM. In this setting, this study brings a scientifically based update concerning effective interventions for maternal mortality prevention during the prenatal period. The most important strategies consist of a tripod with specific interventions related to maternal health promotion, risk prevention and assurance of nutritional support during gestation, in addition to criteria to investigate gestational risk and inclusion of the pregnant woman in the basic component of the prenatal care model. It ends with the definition of priorities in the prevention of MM related to eclampsia/preeclampsia and reinforces the importance of normalization of reference systems for obstetric emergency cases.