Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2004;26(1):53-58
DOI 10.1590/S0100-72032004000100008
PURPOSE: to correlate endometrial thickening diagnosed by ultrasonography with hysteroscopic findings in postmenopausal women. METHODS: a transversal study with hysteroscopic evaluation was performed in 121 postmenopausal women, with endometrial thickening diagnosed through transvaginal ultrasonography. In 98 women there was no history of hormonal replacement therapy, while the remaining 23 received different types of hormone; 55 patients complained of vaginal bleeding and the remaining did not present this condition. The endoscopic examinations were performed in the outpatient clinic, using a 4 mm rigid hysteroscope. For uterine cavity distention carbon dioxide (CO2) was used. Biopsy was performed in all patients, with a 3 mm Novak type curette, and the collected material was submitted to a histopathological study. RESULTS: endometrial thickening varied from 6 to 38 mm, with a mean of 10.7 ± 5.3 mm. The hysteroscopic findings were: polypoid lesion in 51 patients (42.1%); atrophic endometrium in 15 patients (12.4%); senile synechia in 15 patients (12.4%), focal thickening in 13 patients (10.7%); cerebroid lesion in 6 patients (5.0%); proliferative endometrium in 5 patients (4.1%); mucus in 5 patients (4.1%); myoma in 4 patients (3.3%); secreting endometrium in 3 patients (2.5%); endometrial hyperplasia in 3 patients (2.5%); and cystic atrophy in 1 patient (0.8%). Correlation between hysteroscopic findings and cytopathology was observed in 30 of 51 cases of polypoid lesion, in 12 of 15 cases of atrophic endometrium and in all cases in which the diagnosis of endometrial hyperplasia or adenocarcinoma was suspected. CONCLUSION: in the majority of the patients, the hysteroscopic examinations revealed that there was no genuine endometrial thickening but rather other types of lesion in the uterine cavity.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2003;25(7):519-523
DOI 10.1590/S0100-72032003000700009
PURPOSE: to analyze the accuracy of sonohysterography for the evaluation of the uterine cavity in patients with an implantation failure, at the first attempt of an in vitro fertilization cycle. METHODS: in a prospective double blind study, the authors analyzed patients previously submitted to at least one embryo transfer, who presented implantation failures. The patients were submitted to a sonohysterographic examination followed by a diagnostic hysteroscopic examination, carried out by different professionals each of whom was not aware of the results of the other. The results were recorded and only interpreted after the end of the trial. Sonohysterography was performed by the introduction of a urethral catheter 8 into the uterine cervix followed by infusion of physiological saline. The anechoic interface shown by the physiological saline can reveal abnormalities, like uterine polyps or submucosal myomas. Hysteroscopy was performed with a Karl Storz equipment, 4 mm 30º rigid telescope, and infusion of physiological saline for uterine cavity distention. RESULTS: twenty-eight of the 33 originally selected patients for this study were analyzed. Sonohysterography detected abnormalities in 8 patients, five with endometrial polyps (62.5%), two with endocervical polyps (25.0%), and one with submucosal myoma (12.5%). Hysteroscopy (gold standard) detected abnormalities in 7 patients, two with endometrial polyps (28.6%), two with cervical polyps (28.6%) and one with submucosal myoma (14.2%). Sonohysterography, when compared with diagnostic hysteroscopy, presented 71.4% sensibility, 85.7% specificity, 62.5% positive predictive value, and 90% negative predictive value of. CONCLUSION: due to its low positive predictive value, the authors suggest confirmation of the sonohysterography result by diagnostic hysteroscopy. Because sonohysterography presents a good level of specificity and a favorable low negative predictive value, the authors suggest that after a normal sonohysterography diagnostic hysteroscopy to evaluate the uterine cavity before in vitro fertlization is not necessary. This study leads to the conclusion that sonohysterography is a good screening method for the detection of polypoid lesions of the uterine cavity, which could be responsible for implantation failures in in vitro fertilization cycles.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2003;25(4):237-241
DOI 10.1590/S0100-72032003000400003
PURPOSE: to investigate the accuracy of hysteroscopy as a method for the evaluation of the uterine cavity in women with postmenopausal bleeding. METHODS: a cross-sectional study that consisted of the evaluation of 78 women with postmenopausal bleeding submitled to histeroscopy and directed biopsy in the period from January 2000 to June 2002 in the Bahia State Oncology Center. Hysteroscopy findings were classified as benign (leiomyoma, polyp, atrophy, normal) and suspect (hyperplasia, thickening, cancer) and the histopathologic findings as benign (leiomyoma, polyp, non-atypical hyperplasia, atrophy) and malignant (cancer and atypical hyperplasia). The results of hysteroscopy were compared with the pathologic findings. RESULTS: in relation to the suspect results (thickening, hyperplasia and cancer) hysteroscopy sensitivity and specificity were 85.7 and 88.7%, respectively. Positive and negative predictive values were 42.83 and 98.4%. Likelihood ratios of positive and negative tests were 7.6 and 0.16. Accuracy was 88.4% and kappa index, 0.5. CONCLUSION: hysteroscopy alone did not show an acceptable accuracy in the study, reinforcing the idea that its main advantage is to direct the biopsy, and it must always be associated with the histological diagnosis.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2003;25(4):229-235
DOI 10.1590/S0100-72032003000400002
PURPOSE: to determine the association between ultrasonographic, hysteroscopic and histopathologic findings in women with postmenopausal uterine bleeding. METHODS: a retrospective, cross-sectional study was conducted enrolling 156 women with postmenopausal bleeding attended at the Diagnostic Center - IMIP during the period of January 1995 to December 2001. According to the results of the endometrial examination (ultrasound), the patients were classified as having an abnormal or normal finding depending on the cutoffs of 4 or 5 mm. The most common histologic and hysteroscopic findings were studied and classified as premalignant/malignant lesions (hyperplasia/endometrial cancer) or benign findings. These results were compared using the kappa index, to establish the agreement between these techniques. RESULTS: the frequency of endometrial thickening was 75.0 and 67.3% according to cutoffs of 4 mm and 5 mm, respectively. Hysteroscopic findings were atrophic endometrium in 59 (37.8%), endometrial polyp in 56 (35.9%), endometrial hyperplasia in 17 (10.9%), cancer in 16 (10.3%), still active endometrium in 1 (3,2), and other findings in 3 (1.9%). The two most frequent histopathologic findings were also atrophic endometrium (31.4%) and endometrial polyps (26,.3%), followed by scanty material (16.0%), endometrial cancer (10.9%), endometrial hyperplastic changes (9.0%), and others (6.4%). A good agreement between hysteroscopic and histopathologic findings was observed (kappa = 0.61). CONCLUSIONS: the frequency of endometrial thickening was 75.0 and 67.3% according to cutoffs of 4 mm and 5 mm, respectively. No premalignant or malignant lesions were missed when an endometrial cutoff of 4 mm was used. The most frequent hysteroscopic and histopathologic findings were atrophic endometrium and endometrial polyps and a good agreement between these findings was encountered.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2000;22(10):619-625
DOI 10.1590/S0100-72032000001000004
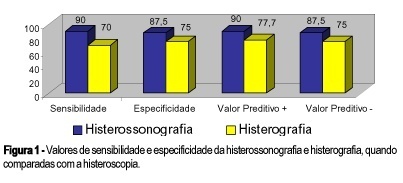
Purpose: to compare the methods used to investigate the endouterine cavity by testing the sensitivity and specificity of X-ray hysterography and sonohysterography compared with hysteroscopy (gold standard). Methods: we carried out a prospective study with 18 patients who, due to symptoms such as irregular menstrual cycles, unexplained postmenopausal uterine bleeding and ultrasound disturbance, were candidates for uterine cavity investigation by X-ray hysterography, sonohysterography and hysteroscopy. Results: sonohysterography sensitivity and specificity were 90 and 87.5%, respectively. Positive and negative predictive values were 90 and 87.5%. For X-ray hysterography, sensitivity, specificity, positive and negative predictive values were 70, 75, 77.7 and 75%, respectively. Conclusion: the use of saline instilation into the endometrial cavity in order to enhance the acuracy of the vaginal ultrasonography seems reliable as a mean to distinguish lesions in the uterine cavity, thereby facilitating the identification of candidates for diagnostic or operative hysteroscopy. X-ray hysterography produces results inferior to hysterosonography.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2000;22(8):495-502
DOI 10.1590/S0100-72032000000800005
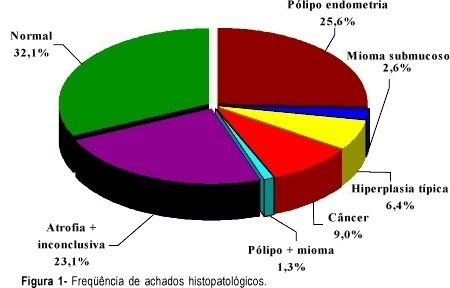
Purpose: to critically evaluate the histopathologic findings and the cost/benefit relation of dilatation and uterine curettage (D&C) in the evaluation of the abnormal uterine bleeding (AUB). Method: retrospective analysis of the histopathological findings in 542 D&C performed for AUB in the Department of Gynecology of the Faculdade de Ciências Médicas da Universidade do Estado do Rio de Janeiro (FCM-UERJ), between January 1984 and January 1994. The patients were divided into two groups: Group 1 - patients <=50 years (385 D&C) and Group 2 -- patients >50 years (157 D&C). Cases of urgency curettage were excluded from the study. All the curettages were accomplished under narcosis. The mean hospitalization lenght was three days. A histopa-thological finding of proliferative, secretory, atrophic or iatrogenic type endometrium was considered a negative pathological result. The term iatrogenic refers to the endometrium under possible influence of hormonal medication. When the histopathological finding evidenced some lesion, this was considered a positive pathological result. Results: in Group 1 there was a negative pathological result in 50.2% of the cases, positive pathological result in 39.7% of the cases, and insufficient material for diagnosis (IMD) in 10.1% of the cases. Endometrial polyp and submucosal leiomyoma were found in only 5.5% and 4.4%, respectively. Cancer was an uncommon observation in that group, endometrial adenocarcinoma (EAC) (five cases) being found in only 1.3% of the cases, in a relation of 77 D&C to one EAC. In Group 2, a negative pathological result was observed in 38.3% of the cases, positive pathological result in 38.1% of the cases and IMD in 23.6% of the cases. Endometrial polyp and submucosal leiomyoma were found only in 5.1% and 0.6%, respectively. Malignant lesions were found in 12% of the cases EAC being 9.5% (15 cases), showing a relation of one EAC to 10 D&C. Conclusions: according to the current knowledge on the etiology of AUB, this study showed that traditional diagnostic D&C has low accuracy in the evaluation of AUB and a cost/benefit relation incompatible with current medicine. Therefore, it should not be the examination of first choice. Considering, however, that EAC was found in one of each 10 D&C in women >50 years with a complaint of uterine bleeding, D&C can be indicated with more liberality in that group, if hysteroscopy with directed biopsy is not available. Nowadays, D&C does not play such a significant a role in the diagnosis of AUB as it did some years ago. However, the procedure is still indicated in some situations and it cannot be abandoned, and its indication should obey restricted criteria.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2001;23(6):371-376
DOI 10.1590/S0100-72032001000600005
Purpose: to evaluate the results of the first 104 hysteroscopic polypectomies in a teaching hospital. Methods: a retrospective descriptive study was designed. Medical records of the first 136 operative hysteroscopies - 104 of which polypectomies - were reviewed. Patient characteristics such as age, parity, period of reproductive function and symptoms; number and size of polyps and results concerning complications and symptom relief were evaluated. Results: the average age of patients was 52.7 years. Three quarters of them were multiparous. Fifty-seven percent of the patients were menopaused. About half of the patients had symptoms related to polyps. Abnormal bleeding was the most frequent symptom (47.1%). In 16.3% of the patients more than 1 polyp were detected and 84% of the polyps were larger than 1 cm. The only immediate complication was a uterine perforation. Late complications were rare and mild. The follow-up period was 9 months on average. In 82% of teh patients the symptoms were controlled. Hysterectomy was necessary in 8.2% of the patients, all of them with other uterine diseases such as leiomyomas, adenomyosis and atypical endometrial hyperplasia in one patient). Conclusion: hysteroscopic polypectomy is a simple, safe and effective method for the treatment of endometrial polyps. Selection of patients must be rigorous to avoid further operative procedures.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2002;24(4):233-239
DOI 10.1590/S0100-72032002000400004
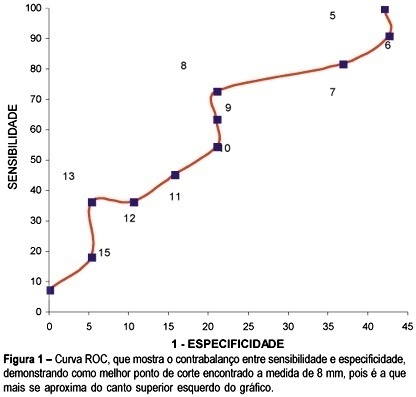
Purpose: to analyze sensitivity, specificity, positive and negative predictive values and the likelihood ratio of transvaginal ultrasound and hysteroscopy when compared with the histopathologic examination of the endometrium in women with breast cancer who have been treated with tamoxifen. Methods: transversal study with 30 women in whom transvaginal ultrasound evaluated the echogenic pattern of endometrial echo and its thickness. Hyteroscopy was performed and described as normal (normal or atrophic endometrium) or abnormal (thickening, polyps, leiomyoma, synechia). Material for histopathology was obtained from endometrial biopsy and the findings were considered normal (irregular endometrial maturation and/or atrophy) or abnormal (polyps, simple or complex hyperplasia, leiomyoma or endometrial carcinoma). Results: the general diagnosis of endometrial modifications was present in 36.6% of patients. The most frequent results were cystic atrophy (46.6%) and endometrial polyps (26.6%). Through the ROC curve the best cutoff of 8 mm of endometrial thickness measure was determined. This measure showed sensitivity of 72.7%, specificity of 72.9%, positive predictive value of 66.6%, negative predictive value of 83.3% and likelihood ratio of 3.4. Hysteroscopy showed sensitivity of 90.9%, specificity of 68.4%, positive predictive value of 62.5%, negative prediction value of 92.8% and likelihood ratio of 2.8. Conclusions: the most frequent endometrial modifications were cystic atrophy followed by polyps. Transvaginal ultrasound showed a higher rate of false-positive (42.1%), when the cutoff for the thickness of the endometrium was 5 mm; however acuracy improved when the measure of 8 mm was used. The cutoff of 8 mm was determined through the ROC curve.