Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2003;25(2):103-107
DOI 10.1590/S0100-72032003000200005
PURPOSE: to study the causes and associated factors of fetal death. METHODS: epidemiological descriptive study, composed of 190 cases of fetal loss amongst 11,825 pregnant women that gave birth at the two only hospitals (Casa de Saúde Divino Espírito Santo and Hospital Nossa Senhora Auxiliadora) of Caratinga City, in the State of Minas Gerais, Brazil, in the period from January 1, 1995 to April 30, 2000. The variables were the number of pregnancies, the timing of the pregnant women at the time of hospitalization, the occurrence of fetal death in relation to delivery and the cause of fetal death. Since there were no comparative groups, tables, percentages and arithmetical means were applied, following the guidelines of the Course of Statistics, of the "Universidade Federal de São Paulo". RESULTS: among the 189 pregnant women with fetal death, 77 were primigravidal and 76 had already been pregnant 2 to 5 times. The gestational age in 113 women was from 20 to 37 weeks. In relation to parturition, the fetal loss occurred during the antepartum period in 164 of 190 dead fetuses. The most frequently noticed death causes were: abruptio placentae in 35 cases, fetal anomaly in 12 cases, and hypertension syndrome in 8 cases. Nervertheless, there was no explanation for the etiology of 117 cases of fetal death. CONCLUSION: stillbirth has frequently been observed among the primigravidae (40.74%), in preterm period (59.79%), and in the antepartum period (86.31%). Among fetal death causes, the most frequent was a abruptio placentae (18.42%), and in 61.57% of the cases the fetal death could not be explained.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2001;23(5):283-287
DOI 10.1590/S0100-72032001000500003
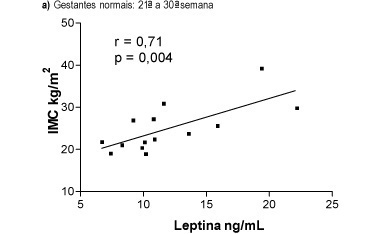
Purpose: to study in primigravid adolescents the behavior of serum leptin levels during the evolution of normal pregnancy, comparing the results with those obtained from preeclamptics. Methods: prospective, longitudinal study conducted in 15 normotensive pregnant adolescents and 5 preeclamptic adolescents. Serum leptin levels (ng/mL) were determined by radioimmunoassay. Blood pressure was measured by the oscilometric method by using DINAMAP 1846. Patients were evaluated in two different gestational periods: between the 21st and 30th week and between the 31st and 40th week. The ratio leptin/body mass index (BMI) was used to correct changes observed in BMI throughout gestation. Preeclamptic pregnant patients were diagnosed when the blood pressure was > or = 140/90 mmHg, proteinuria >300 mg/24 h and when arteriolar spasm was present in the optic fundi. Results: there was a trend towards an elevation of serum leptin at the end of pregnancy in both groups although more pronounced in preeclamptic patients. In pregnant normotensive patients serum leptin increased from 11.9±1.20 (21stto 30th week) to 13.9±2.23 ng/mL (31st to 40th week), and in preeclamptic from 11.9±1.20 to 17.6±4.565 ng/mL. In preeclamptic patients the BMI increased significantly in the period from the 21st to 30th week when compared to the period between the 31st and 40thweek: 21.5±0.8 vs 27.4±1.7 kg/m², p<0.05.In normotensive these values were maintained stable: 24.9±1.5 vs 25.1±1.00 kg/m². At the end of gestation the ratio leptin/BMI was significantly higher in preeclamptics: 0.56±0.06 (21stto 30thweek) vs 0.70±0.15, p<0.05. The values of the ratio leptin/BMI in normotensive pregnants varied from 0.44±0.02 between the 21st and 30th week to 0.41±0.04 between the 31st to 40thweek. In normal pregnants there was a direct and significant correlation between the levels of leptin and BMI in both periods of pregnancy: r = 0.7, p<0.004 (31st to 40th ) vs r = 0.94, p<0.0001 (31st to 40th week). These correlations were lost in preeclamptic patients in both gestational periods. Conclusion: the higher concentrations of leptin and leptin/BMI ratio observed when preeclamptics were compared with normotensive patients, in both gestational periods, suggest a leptin resistance pattern in preeclampsia.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2001;23(7):431-438
DOI 10.1590/S0100-72032001000700004
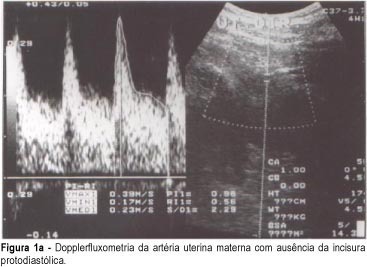
Purpose: to evaluate the association between the presence of diastolic notch in the maternal uterine arteries, and the histopathological changes of the uteroplacental vessels. Methods: transversal study of 144 women with single pregnancy interrupted by cesarean section between 27 and 41 weeks. In this sample, 84 had pregnancies complicated by preeclampsia and the other 60 were normal. In this group, Doppler study of both uterine arteries and placental bed biopsy was performed. Results: of the total of 144 patients, 88 patients (61%) had a biopsy fragment that was considered representative of the placental bed. The diastolic notch was present in 40 patients (70%) of the total of cases with inadequate physiologic alterations and absent in 28 patients (90%) of the total of cases with physiologic alterations (p=0.0000). The Doppler study showed 70% sensitivity, 90% specificity, 44% positive predictive value and 97% negative predictive value. The association between bilateral diastolic notch of uterine arteries and acute atherosis in the placental bed was also significant (24 out of 25 cases -- p=0.000). The Doppler study showed 96% sensitivity, 70% specificity, 26% positive predictive value and 99% negative predictive value, while for arteriolosclerosis its results were 80% sensitivity, 55% specificity, 17% positive predictive value and 96% negative predictive value. Conclusions: the diastolic notch in the maternal uterine is a safe indicator of pathological vessel alteration in the placental bed. The adequate trophoblast migration into the myometrium, revealed by physiologic changes, results in the absence of bilateral diastolic notch of the maternal uterine arteries.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2002;24(8):555-559
DOI 10.1590/S0100-72032002000800009
The hemolytic - uremic syndrome (HUS) presents with a triad of acute renal failure, microangiopathic hemolytic anemia and thrombocytopenia associated with high morbidity and mortality. On the differential diagnosis, other entities must be considered like preeclampsia, HELLP syndrome, acute fatty liver of pregnancy and thrombotic thrombocytopenic purpura. We report a case of HUS occurring in the immediate postpartum period in a patient initially diagnosed as having preeclampsia. The differential diagnosis was based on abrupt renal failure, blood pressure increase and clinical and laboratorial evidence of hemolysis. Attention is directed to investigation, clinical management and prognosis based on review of the literature.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2002;24(8):527-533
DOI 10.1590/S0100-72032002000800005
Purpose: to analyze the perinatal results of patients submitted to a 100 g oral glucose tolerance test (OGTT) during prenatal care at the Instituto Materno-Infantil de Pernambuco (IMIP), according to three different criteria. Methods: a cross-sectional study was conducted involving 210 pregnant patients attended at the IMIP, who were tested by a 100 g OGTT and had a singleton, topic pregnancy, without history of diabetes or glucose intolerance before pregnancy, and who delivered at the IMIP. The patients were classified into one of the following categories according to the levels found by OGTT: controls, mild hyperglycemia, Bertini's group, Carpenter's group and the National Diabetes Data Group (NDDG). These classes were then compared and association between the categories and preeclampsia, large for gestational age (LGA) newborns, rate of cesarean delivery, stillbirth, and mean birth weight was investigated. Results: the frequency of gestational diabetes was 48.1, 18.1, and 9% according to Bertini's, Carpenter and Coustan's and NDDG criteria, respectively, and mild hyperglycemia was present in 10.5%. Age of patients increased with a higher degree of carbohydrate intolerance. The groups did not differ regarding frequency of LGA, C-section, stillbirths, and birth weight. There was an increased frequency of preeclampsia among women with hyperglycemia and gestational diabetes according to Carpenter and Coustan's criteria. Conclusions: prevalence of gestational diabetes varied between 9 and 48% according to the different criteria, but maternal and perinatal results did not differ significantly among the groups. Strict diagnostic criteria can determine overdiagnosis without improvement of perinatal outcome.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2002;24(1):09-13
DOI 10.1590/S0100-72032002000100002
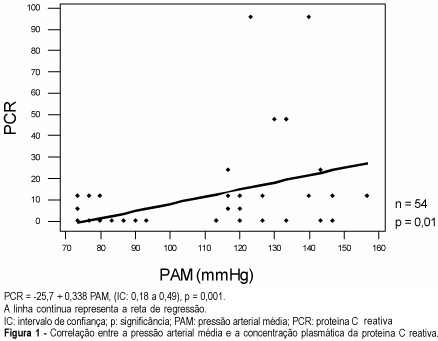
Purpose: to investigate the association between serum C-reactive protein concentration and preeclampsia occurrence, as well as its relation to the disease severity. Patients and Methods: twenty-seven preeclamptic pregnant women and 27 pregnant women with no clinical intercurrences, in the third trimester of pregnancy, were evaluated in a transversal case-control study. Serum C-reactive protein dosage, besides clinical examination and laboratory tests for the diagnosis of the disease, were performed in the antenatal period. The association between C-reactive protein and the presence of preeclampsia, and the correlation between plasma protein values and blood pressure values were investigated. The chi² significance test and regression analysis through the square minimum technique were used, and the results were considered to be statistically significant when p<0.05. Results: the preeclamptic pregnant women presented mean blood pressure levels higher than their controls (129.9±12.1 and 87.2±6.5 mmHg, respectively) and significantly higher C-reactive protein mean values than the normotensive women (18.9±4.9 and 1.56±0.8 mg/L, respectively). There was a significant association between the C-reactive protein concentration increase and preeclampsia occurrence (p<0.0001, odds ratio: 20.1). It was also observed that the mean arterial pressure and proteinuria presented a direct correlation with the circulating C-reactive protein in maternal blood (p=0.001 and p<0.001, respectively). Conclusion: C-reactive protein is an effective marker of preeclampsia occurrence and significantly correlates with the disease severity. The use of this test for the differential diagnosis of pregnant women in several hypertensive situations and its utilization as a marker of preeclampsia prognosis deserve further studies.