Summary
Revista Brasileira de Ginecologia e Obstetrícia. 1998;20(6):357-360
DOI 10.1590/S0100-72031998000600009
Bilateral ectopic pregnancy is the most unusual twin gestation considering that less than 250 cases have been reported in the literature. Our case fulfills the diagnostic criterion determined by Norris9 which requires demonstration of chorionic villi in each fallopian tube. We report the case of a 36-year-old multiparous woman who had an hemorrhagic acute abdomen. A laparotomy performed under general anesthesia revealed hemoperitoneum of 1.8 liters and both swelled tubes with laceration of their walls, besides two embryos with 2,7 and 3,0 cm in length free in the intra-abdominal blood. A literature review on bilateral ectopic pregnancy is presented.

Summary
Revista Brasileira de Ginecologia e Obstetrícia. 1998;20(3):127-135
DOI 10.1590/S0100-72031998000300002
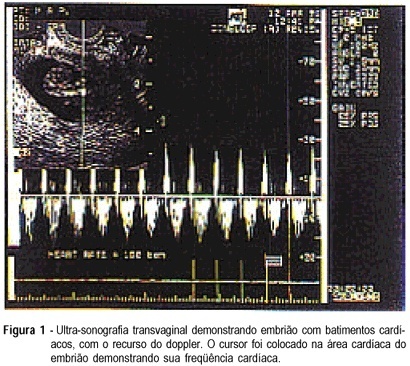
A prospective study was performed with 42 patients with unruptured ectopic pregnancy, which intended to elaborate an index to orient the systemic treatment with the administration of a single intramuscular dose of methotrexate (50 mg/m²). Patients were monitored with beta-hCG titers on days 1, 4 and 7 after the methotrexate. When the titers of beta-hCG declined more than 15%, between days 4 and 7 after methotrexate, the patients were discharged and had an outpatient follow-up monitored with beta-hCG titers weekly until the titers were less than 5 mIU/ml, which represents success of the treatment. We prepared an index for the systemic treatment with methotrexate, with five parameters: (1) initial titers of beta-hCG; (2) aspects of the image at ultrasound (hematosalpinx, gestational sac, live embryo); (3) size of the mass; (4) free fluid in cul-de-sac; (5) collor doppler. Each parameter received a grade from 0 to 2. Grade 0 represented bad prognosis, favorable parameters received grade 2 and borderline parameters received grade one. The success rate with a single dose of methotrexate was 69.0% (29/42). The color doppler was performed in 20 of the 42 patients; in this group of 20 patients the success rate was 75.0% (15/20). In the 22 patients who were not submitted to the color doppler, the average grade of the score in the successful cases was 6.6, and in the unsuccessful it was 3.1. In the group who underwent the doppler (20 patients) the average was 7.9 in the successful cases and 4.2 in the cases that failed. In the present study the cut-off grade was 5, for most of the patients with grades above 5 had a successful treatment (15/16 - 93.75%), while grades equal or below 5 failed. The score will help to indicate the best cases for the medical treatment. We do not advise the treatment when the grade is equal or below 5. Therefore, we can predict a good evolution of the treatment when the grade is above five.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 1999;21(3):153-157
DOI 10.1590/S0100-72031999000300006
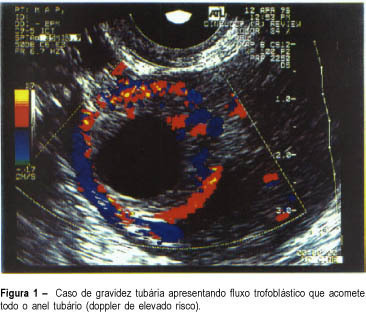
Purpose: to evaluate the efficacy of color Doppler in the prediction of results of the systemic treatment of unruptured ectopic pregnancy with a single dose of methotrexate. Methodology: twenty patients with a diagnosis of ectopic pregnancy were included in the study. The inclusion criteria were: hemodynamic stability, adnexal mass < 5.0 cm and decline of the titers of beta-hCG less than 15% in an interval of 24 h. The exclusion criteria were hepatic or renal disease and blood dyscrasias. Follow-up was by serial determinations of beta-hCG on days 4 and 7 after the beginning of the treatment, and weekly until the titers were negative. The patients were classified into 3 groups according to color Doppler: high risk (trophoblastic flow covering more than 2/3 of the mass), medium risk (when trophoblastic flow compromised 1/3 to 2/3 of tubal mass) and low risk (when trophoblastic flow covered less than 1/3 of the mass). Results: the success of the treatment with a single dose was 75% (15/20); when a second dose of MTX was used, the success rate was 85%. When comparing color Doppler with the results of the medical treatment, we had high risk in 4 patients and in all the treatment failed; medium and low risk in 16 patients, and in 15 the treatment was successful. Conclusion: color Doppler showing high risk indicated an unfavorable situation for the medical treatment with MTX, while medium and low risk in color doppler were favorable situations for the clinical treatment. However, these results should always be analyzed in association with the evolution curve of the beta-hCG titers.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 1999;21(6):347-350
DOI 10.1590/S0100-72031999000600008
Purpose: to evaluate safety and efficacy of intra-amniotic injection of methotrexate (MTX) for treatment of viable cervical pregnancy. Methods: four women with viable cervical pregnancy confirmed by ultrasound (US) were treated with transvaginal injection of MTX (1 mg/kg) under sonographic control. The follow-up was made with serial dosages of beta-hCG on days 1, 4 and 7 after injection and weekly until the titers were negative. Results: the patients were treated with success. The time for the titers of beta-hCG to become negative after the treatment was: 62 days (case 1), 84 days (case 2), 28 days (case 3) and 10 days (case 4). Conclusion: intra-amniotic injection of MTX can be used to avoid surgery in cases of viable cervical pregnancy.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 1999;21(8):465-470
DOI 10.1590/S0100-72031999000800007
SUMMARY Objective: to evaluate the inclusion parameters in the selection of cases of (tubal) ectopic pregnancy for expectant management and to assess the results. Methods: a prospective study was carried out in 70 patients with unruptured (tubal) ectopic pregnancy, with the objective to carry out an expectant management. The main inclusion criteria in this study were the diameter of the tubal mass, that should be equal or inferior to 5,0 cm, reduced titles of beta-hCG (beta fraction of the chorionic gonadotropic hormone) as compared to the initial value within an interval of 48 h, hemodynamic stability, wishes for future pregnancy and a written permission to participate in the study. All patients were observed in the hospital and when reduction in beta-hCG titles was observed, the patients were discharged from the hospital and followed in the outpatient department, with weekly determinations of beta-hCG until levels lower than 5 mIU/ml were reached, that were considered successful. Results: of the 70 patients who underwent expectant management, only one needed a surgical intervention, because of tubal rupture. The initial values of beta-hCG of the patients ranged from 27 mIU/ml to 41,000 mIU/ml. The average diameter of the tubal mass was 2.9 cm. The presence of free liquid in the peritoneal cavity was observed in 50 patients, small amount in 26 patients, moderate in 16 and large in 8 patients. The ultrasonographic resolution of hematosalpinx occurred in 58 patients and tubal ring was visualized in 12 patients. On color Doppler, 52 were at low risk and 18 at medium risk. Conclusions: the expectant management should be applied with safety in the cases that respect the inclusion criteria, the index of success of this study being 98.6%.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 1999;21(10):611-615
DOI 10.1590/S0100-72031999001000009
Term abdominal pregnancy with live fetus is an obstetrical rarity with high fetal and maternal morbidity and mortality. The authors present a case of abdominal pregnancy in a 43-year-old woman. The diagnosis was made only at term (37 weeks) by clinical findings and echography. Exploratory laparotomy was performed and a living female newborn weighing 2,570 g was extracted. Apgar scores were 3, 6 and 8 at the 1st, 5th and 10th minutes, respectively. Placenta was inserted in the omentum and was removed without complications. Postoperative course was uneventful and both mother and child were discharged healthy.

Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2004;26(9):741-743
DOI 10.1590/S0100-72032004000900011
Ectopic pregnancy is the implantation and development of the ovum outside the uterine cavity; it needs a quick diagnosis and an urgent treatment. The presence of the corpus luteum in the ovary that is contralateral to the ectopic pregnancy is presumptive evidence for ovum transmigration, which may be the cause of ectopic pregnancy. In 1994, a multinational clinical trial proved the superiority of levonorgestrel over the existing emergency contraceptive products. In the present study, we describe the case of a 27-year-old woman with ectopic pregnancy and a contralateral corpus luteum after use of hormonal emergency contraception (levonorgestrel), because of failure of the used contraception method (condom). The patient was treated with laparoscopic surgery that was successful.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2004;26(6):471-475
DOI 10.1590/S0100-72032004000600008
OBJECTIVE: to evaluate the correlation between the beta-human chorionic gonadotropin (beta-hCG) serum levels and the measurement of the endometrial thickness, in patients under treatment of ectopic pregnancy with methotrexate. METHODS: a prospective study in which the levels of beta-hCG as well as the largest measurement of the endometrial thickness on the uterine longitudinal axis through transvaginal ultrasound were evaluated at 24-48 h intervals in thirty-eight patients with hemodynamic stability, ectopic pregnancy, diameter <3.5 cm, and increased beta-hCG levels. All the patients got methotrexate in a single-dose therapy (50 mg/m² im). We compared the mean values of beta-hCG and endometrial thickness of cases that evolved successfully versus the poor responders using the Student t-test. Afterwards we analyzed the difference of the beta-hCG mean serum values related to the endometrial thickness(<10.0 mm and >10.0 mm) independently of the response to treatment employing the Student t-test. RESULTS: the mean values of beta-hCG and endometrial thickness in patients with successful treatment (28 cases) were 1936.2 mIU/ml and 6.4 mm, respectively, significanlty lower than the mean values for insuccessful cases: 6831.3 mIU/ml and 11.7 mm, respectively (p<0.05). The mean values of beta-hCG in women with endometrial thickness <10.0 mm were 2008.7 mIU/ml, significantly lower than the ones with endometrium >10.0 mm, whose mean values were 6925.9 mIU/ml (<0.05). CONCLUSIONS: the measurement of the endometrial thickness through ultrasound is under the beta-hCG serum values influence, and it showed to be a valuable additional factor to suggest medical treatment with methotrexate in the non-disrupted ectopic pregnancy.