Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2017;39(11):622-631
Preeclampsia, a multifactorial disease with pathophysiology not yet fully understood, is a major cause of maternal and perinatal morbidity and mortality, especially when preterm. The diagnosis is performed when there is an association between arterial hypertension and proteinuria or evidence of severity. There are unanswered questions in the literature considering the timing of delivery once preterm preeclampsia has been diagnosed, given the risk of developingmaternal complications versus the risk of adverse perinatal outcomes associated with prematurity. The objective of this systematic review is to determine the best timing of delivery for women diagnosed with preeclampsia before 37 weeks of gestation.
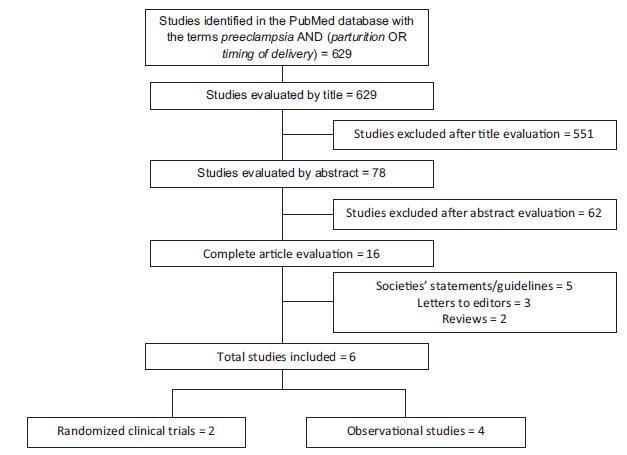
Systematic literature review, performed in the PubMed database, using the terms preeclampsia, parturition and timing of delivery to look for studies conducted between 2014 and 2017. Studies that compared the maternal and perinatal outcomes of women who underwent immediate delivery or delayed delivery, in the absence of evidence of severe preeclampsia, were selected.
A total of 629 studies were initially retrieved. After reading the titles, 78 were selected, and their abstracts, evaluated; 16 were then evaluated in full and, in the end, 6 studies (2 randomized clinical trials and 4 observational studies) met the inclusion criteria. The results were presented according to gestational age range (< 34 weeks and between 34 and 37 weeks) and by maternal and perinatal outcomes, according to the timing of delivery, considering immediate delivery or expectant management. Before 34 weeks, thematernal outcomeswere similar, but the perinatal outcomes were significantly worse when immediate delivery occurred. Between 34 and 37 weeks, the progression to severe maternal disease was slightly higher among women undergoing expectant management, however, with better perinatal outcomes.
When there is no evidence of severe preeclampsia or impaired fetal wellbeing, especially before 34 weeks, the pregnancy should be carefully surveilled, and the delivery, postponed, aiming at improving the perinatal outcomes. Between 34 and 37 weeks, the decision on the timing of delivery should be shared with the pregnant woman and her family, after providing information regarding the risks of adverse outcomes associated with preeclampsia and prematurity.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2009;31(6):279-284
DOI 10.1590/S0100-72032009000600003
PURPOSE: to evaluate the effect of delivery type and usual obstetric procedures on the neurologic condition of a sample of consecutive term and healthy neonates, in the first 48 hours of life, using the Neurologic Adaptative Capacity Score (NACS) system. METHODS: cohort prospective study with 313 neonates, from a neonatology unit: Unidade de Neonatologia e Alojamento Conjunto. The variables analyzed were obstetric variables; clinical outcome: low neurologic vigor phase, evaluated by NACS, at 4, 24 and 48 hours of life. The data have been assessed twice: once with the whole sample and the other comparing the Vigorous Group, whose neonates kept a score of 35 or more during the three evaluations, and the Low Vigor Group, with less than 35 scores during the three consecutive evaluations. Bivariate and multivariate analyses have been done. Possible associations between low neurologic vigor phase and the type of delivery, as well between the low neurologic vigor phase and obstetric variables have been searched. RESULTS: in the bivariate analysis, the delivery type and the obstetric variables were not associated with the low neurologic vigor phase. Nevertheless, the association between the amniotic fluid and the low neurologic vigor phase reached values very close to significance and, then, it was included in the multivariate analysis. In the multivariate analysis, the only variable associated with low neurologic vigor was the presence of meconium stained amniotic fluid, which has shown to be 8.1 times more risky for the neurologic scoring, when Vigorous Group and Low Vigor Group were compared. In the analysis of the whole sample, the same risk was 1.7. CONCLUSIONS: neither the delivery type, nor the usual obstetric procedures were associated with low neurologic vigor phase. This is useful information, clinically or legally speaking, mainly for obstetricians. According to this sample data, when the term neonate is healthy, the delivery type and the usual obstetric procedures have no impact in the neurologic condition.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 1999;21(2):99-104
DOI 10.1590/S0100-72031999000200007
Purpose: to study the actual conditions of medical assistance and types of delivery and factors contributing to their indication in Uberaba, MG. Method: the data of 4,294 puerperas who gave birth in the period from April 15, 1992 to April 14, 1993 in 7 maternities in Uberaba were studied. Results: it was seen that the Teaching Hospital had a greater participation in deliveries attending the younger population, probably the poorest and most unprepared regarding pregnancy. It was the only Hospital in which cesarean section rates were near those accepted by the who. Medical assistance in Uberaba was predominantly through Social Security (SUS), private health insurance and physicians representing a lower proportion. It was also verified that cesarean section frequency increased with age and type of medical assistance and the groups with private coverage presented a higher number of cesarean sections. Conclusion: it may be perhaps justified to consider the social factor as interfering with the indication of type of delivery.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 1999;21(9):519-525
DOI 10.1590/S0100-72031999000900004
Purpose: to present the perinatal outcomes resulting from the use of a protocol for assistance to diabetic pregnant women used at the Center for Integral Assistance to Women's Health (CAISM), of the University of Campinas. Methods: ninety diabetic pregnant women, who were assisted at the institution with this protocol, were compared with two control grups: the first consisted of 180 pregnant women with equal number of gestations and same age (control A) and the second consisted of 180 randomly selected pregnant women (control B). The study variables were route of delivery, indication for cesarean section, gestational age, Apgar score at first and fifth minute, weight, adequacy of weight for gestational age and perinatal morbidity and mortality. For the statistical analysis Student's t-test and the chi2 test were used. Results: there was a higher incidence of cesarean sections, prematures and large to gestational age (LGA) babies among diabetic women, as well as higher occurrence of neonatal morbidity such as hypoglycemia, hypocalcemia, hyperbilirubinemia, respiratory distress and neonatal depression. The incidence of low Apgar score and perinatal mortality was significantly higher than in the randomly selected group, but the same as in the group matched regarding age and number of pregnancies. Conclusions: although this protocol intends to obtain a perfect metabolic control among diabetic pregnant women, the perinatal outcomes are still unfavorable in comparison to nondiabetic pregnant women.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2004;26(9):703-707
DOI 10.1590/S0100-72032004000900005
PURPOSE: to analyze the association between modes of consecutive deliveries of 714 adolescents attended at the Maternity sector of the Hospital das Clínicas da Universidade Federal de Pernambuco (Federal University of Pernambuco), from January to December 2001. PATIENTS AND METHODS: according to a prospective, analytic, transversal, and incidence type study, the sequence of delivery modes was analyzed from the first to the fourth parturition of 714 pregnant adolescents, aged from 13 to 19 years (mean17.2±1.5 years). Every day, after identifying the adolescents who delivered, by the parturition room register, they were invited to participate in this study. Those who agreed, after signing a free informed consent answered a structured questionnaire with 65 direct questions with precodified closed options, among which were delivery mode and number of gestations. RESULTS: it was found that 527 (73.8%) adolescents had only one delivery, 149 (20.9%) two deliveries, 35 (4.9%) three deliveries, and 3 (0.4%) had had four deliveries. Among the 273 cesarean sections, 207 (75.8%) occurred in primiparae, 65 (23.8%) in secundiparae and one (0.4%) in a multipara. There was a statistically significant association between the first and the second deliveries for 83 (55.7%) adolescents who had transvaginal delivery, as well as for 41 (27.5%) by cesarean section. There was also coincidence about the second and third deliveries, regarding transvaginal delivery of 23 (65.7%) adolescents, as well as cesarean section of 10 (28.6%) adolescents. CONCLUSION: a tendency to coincidence of subsequent delivery modes was identified for adolescents until the third parturition.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2003;25(4):255-260
DOI 10.1590/S0100-72032003000400006
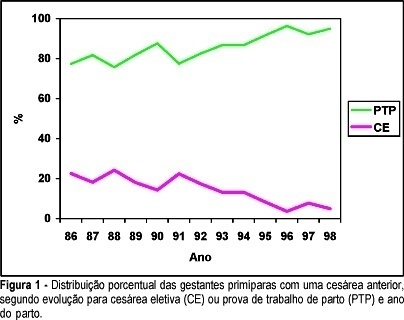
PURPOSE: to compare maternal morbidity, neonatal results and some clinical and epidemiological characteristics among primiparous women who had one previous cesarean section, according to the performance of elective cesarean (EC) section or trial of labor (TL) during the second delivery. PATIENTS AND METHODS: this is a retrospective cross-sectional study on the second delivery of women who previously had a cesarean section and were assisted at the Center for Integral Assistance to Women's Health (CAISM/UNICAMP), from 1986 to 1998. Data were collected from 2068 clinical records corresponding to 322 cases of EC and 1746 of TL. Data analysis was performed through percentage distribution of the EC and TL cases and also the distribution of variables between these two groups, using the chi2, chi2 for trend and Fisher exact tests to evaluate the statistical difference, with a significance level of 95%. RESULTS: the indication of EC decreased progressively with time, from 22.6% in 1986 to 5% in 1998. Maternal morbity was similar and low in both groups (1.24% and 1.21%). There was no significant difference between groups regarding Apgar score and stillbirths, but there was a significantly higher proportion of premature newborns and with birth weight below 2.500 g and above 4.000 g in the group who underwent EC. The prevalence of EC was significantly higher in women 35 or more years old, with previous or current history of hypertensive disorder, diabetes or with a first dead child, as well as with changes in the volume of amniotic fluid. CONCLUSIONS: performing TL progressively increased during this period of thirteen years, without any increase of maternal and/or neonatal morbidity. The indication for EC followed medical criteria related to unfavorable maternal and/or fetal clinical conditions for vaginal delivery.