Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2004;26(10):781-786
DOI 10.1590/S0100-72032004001000005
PURPOSE: to assess the obstetric and perinatal outcomes in cases of term newborns in breech presentation, in patients with previous vaginal deliveries, comparing them to term newborns in vertex presentation. METHODS: 8,350 deliveries retrospectively from March 1998 to July 2003 were analysed. Of 419 deliveries (5.1%) in breech presentation, 58 cases were selected for the study (breech group), according to the following criteria: patients who had had one or more babies through vaginal delivery, gestational age ³37 weeks, no fetal malformation, no complications in the current pregnancy, birth weight between 2,500 and 3,750 g, and no previous cesarean section. The breech group was matched to 1,327 newborns in vertex position from pregnant women with no previous cesarean section (vertex group). Maternal age, parity, gestational age, delivery way, birth weight, meconium-stained amniotic fluid, 1- and 5-min Apgar score, need of neonatal intensive care unit, and small- and big-for-gestational age newborns were analyzed. Statistical analysis was performed by the c² test and by Student's t test, with the level of significance set at p<0.05. RESULTS: when breech and vertex groups were compared, they showed significant differences regarding the following variables: birth weight (3,091±538 g vs 3,250±497 g; p<0.01), vaginal delivery (63.8 vs 95.0%; p<0.0001), cesarean section (36.2 vs 5.0%; p<0,0001), and 1-min Apgar score (p<0.0001), respectively. CONCLUSIONS: we conclude that in term fetuses in breech position from pregnant women with previous vaginal deliveries, birth weight, delivery way, and 1-min Apgar score were different compared to fetuses in vertex position from women with the same characteristics.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2004;26(10):791-798
DOI 10.1590/S0100-72032004001000006
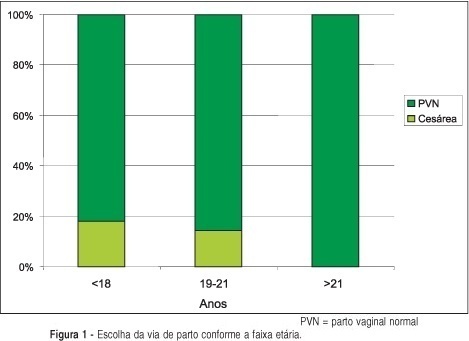
PURPOSE: to find out the preference in regard to the way of delivery among primigravidae, as well as the reasons for their choice, in order to improve the quality of the doctor-patient relationship. METHODS: a qualitative-type study was conducted through analysis of the collective subject, including primigravidae attended from September to November 2003 at the emergency rooms of the hospital of the "Faculdade de Medicina de Jundiaí". A questionnaire, specially developed to accomplish the proposed objectives was applied. An informed and free consent, signed by the pregnant woman and one of the researchers in charge was obtained. This questionnaire was based on doubts of patients attended at this hospital some months before the trial. For the purpose of sample standardization, the patients' selection followed some inclusion criteria: age above 16, primigravidae that were receiving prenatal assistance and a post-informed and free consent. Mental disorders and clinical and/or obstetric pathologies that could interfere in the patient's choice were considered exclusion criteria. RESULTS: the studied population had as prevailing profile women in the third quarter of gestation, above 21 years of age, white, married and with completed school. Most of the women (90%) preferred vaginal delivery for the following main reasons: ease to be done (94%) and the fear of suffering and pain during the postpartum period caused by cesarean section. There was a relationship between older and married women and the preference for vaginal delivery, with no significant difference between races. CONCLUSION: these results show an enormous contrast between women's preference and the high cesarean section rates in Brazil. We conclude that there may be a lack of information and dialogue between the health professionals and patients about the possible difficulties, doubts and anxieties that involve the women's choice for a specific way of delivery. From an ethical point of view, we conclude that obstetricians should question every cesarean section indication and take into account the women's right to choose, without ignoring clinical criteria, when making the medical decision about the way of delivery.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2004;26(9):703-707
DOI 10.1590/S0100-72032004000900005
PURPOSE: to analyze the association between modes of consecutive deliveries of 714 adolescents attended at the Maternity sector of the Hospital das Clínicas da Universidade Federal de Pernambuco (Federal University of Pernambuco), from January to December 2001. PATIENTS AND METHODS: according to a prospective, analytic, transversal, and incidence type study, the sequence of delivery modes was analyzed from the first to the fourth parturition of 714 pregnant adolescents, aged from 13 to 19 years (mean17.2±1.5 years). Every day, after identifying the adolescents who delivered, by the parturition room register, they were invited to participate in this study. Those who agreed, after signing a free informed consent answered a structured questionnaire with 65 direct questions with precodified closed options, among which were delivery mode and number of gestations. RESULTS: it was found that 527 (73.8%) adolescents had only one delivery, 149 (20.9%) two deliveries, 35 (4.9%) three deliveries, and 3 (0.4%) had had four deliveries. Among the 273 cesarean sections, 207 (75.8%) occurred in primiparae, 65 (23.8%) in secundiparae and one (0.4%) in a multipara. There was a statistically significant association between the first and the second deliveries for 83 (55.7%) adolescents who had transvaginal delivery, as well as for 41 (27.5%) by cesarean section. There was also coincidence about the second and third deliveries, regarding transvaginal delivery of 23 (65.7%) adolescents, as well as cesarean section of 10 (28.6%) adolescents. CONCLUSION: a tendency to coincidence of subsequent delivery modes was identified for adolescents until the third parturition.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2004;26(9):709-714
DOI 10.1590/S0100-72032004000900006
PURPOSE: to study the relationship between previous cesarean section and abruptio placentae. METHODS: a retrospective study reviewed 6495 deliveries between April 2001 and January 2004. The adopted inclusion criteria were: clinical diagnosis of abruptio placentae confirmed by placental examination after delivery, single pregnancy, birth weight >500 g, gestational age >22 weeks and no history of abdominal trauma. Five controls were selected for each abruptio placentae case and were matched for the following parameters: parity, gestational age (< or > 30 weeks), maternal arterial hypertension during pregnancy, presence of nonobstetrical uterine scar, premature rupture of membranes and polyhydramnios. Statistical analysis of continuous variables was perfomed by Student's t test. Statistical significance of the comparisons of categorical variables was evaluated by the chi2 test or by the Fisher exact test. p values <0.05 were considered to be significant. RESULTS: thirty-four cases of abruptio placentae were included (incidence 0.52%). The control group included 170 cases that fulfilled the matching criteria. The incidence of previous cesarean section in the abruptio placentae group was 26.5% (9 cases) and in the control group it was 21.2% (36 cases). No significant difference was found between the groups (p=0.65, OR=1.34, CI 95%=0.53-3.34). CONCLUSION: the present study was not able to demonstrate association between abruptio placentae and previous cesarean section.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2004;26(8):633-639
DOI 10.1590/S0100-72032004000800007
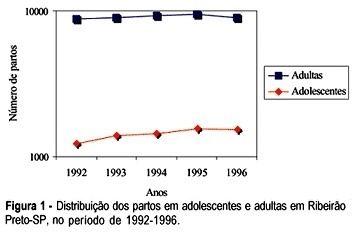
PURPOSE: to check whether there were differences in some social indicators between adolescent and adult pregnant women in the city of Ribeirão Preto, from January 1992 to December 1996. METHODS: the information was obtained from hospital discharge forms and was analyzed at the Hospital Data Processing Center of the FMRP-USP. The analyzed parameters were: number and types of deliveries, category of hospital admission, occupation, and obstetric diagnosis. The 6.04a text processor Epi-Info System, a data bank and statistics of epidemiology produced by the Centers of Disease Control and Prevention (Atlanta, GA, USA), and Dbase IV were used to process the information. The association between variables was tested by the chi² test, with level of significance set at 5%, using the GraphPad Prism version 2.0, 1995 software. RESULTS: a total of 43,253 deliveries occurred during this period, among which 7,134 (16.5%) corresponded to adolescent deliveries, while 36,119 (83.5%) to adult deliveries. The number of deliveries by adolescent girls increased 25.5% along this period. The proportion of adolescent deliveries in the unified health system category of admission increased, and it was higher than that of the adults'. Only 14.1% of the adolescents belonged to the economically active population, comparing with 34.8% of the adults. Only 6.8% of the adolescents were students, while 79.0% were house-workers or had a nonpaid occupation. In the analyzed period, the ratio of vaginal delivery increased among the adolescents, as compared to that of the adults. The ratio of cesarean delivery persisted stable and higher among the adults. Premature delivery and false labor were significantly more frequent among the adolescents. CONCLUSION: the number of deliveries increased among the adolescents, and most of them were normal. The ratio of admission by the unified health system category and that of vaginal delivery were higher among the adolescents. There were more adolescents without an economically active work. Thus, we recommend strategies to prevent adolescent pregnancy, mainly among the poor population.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2003;25(10):739-744
DOI 10.1590/S0100-72032003001000007
PURPOSE: to verify the contribution of maternal age, parity, twin pregnancy, hypertensive syndrome, and premature rupture of membranes as risk factors for cesarean section. METHODS: after approval by the Ethics in Research Committee of the "Maternidade Professor Monteiro de Morais" - Recife, PE - Brazil, for a case control study, the authors analyzed data from 3919 pregnant women, without two or more prior cesarean sections, who gave birth to alive newborns with gestational age equal to or more than 28 weeks, weighing at least 1,000 g, on cephalic presentation, from September 1, 1999 to August 31, 2000. The case group included women submitted to cesarean section and the control group included women submitted to vaginal delivery. With the data collected from obstetric and neonatal reports, the authors performed multivariate analysis by logistic regression to determine a mathematical equation that associates cesarean probability due to more than one independent variable acting as risk factor, determining odds ratio with a confidence interval of 95% (95% CI), for the variables: maternal age, parity, twin pregnancy, hypertensive syndrome, and premature rupture of membranes. RESULTS: the chances for cesarean section significantly increased 8.3 times in twin pregnancy (OR = 8.3; 95% CI: 3.7-19.1), 3.4 in hypertensive syndrome (OR = 3.4; 95% CI: 2.9-4.0), 1.9 in primiparity (OR = 1.9; 95% CI: 1.8-2.0), 1.5 in maternal age over 34 years (OR = 1.5; 95% CI: 1.2-1.8), and 1.2 in the presence of premature rupture of membranes (OR = 1.2; 95 %CI: 1.0-1.4). CONCLUSIONS: the risk for cesarean section was greater in the presence of premature rupture of membranes, maternal age greater than 34 years, primiparity, hypertensive syndrome, and twin pregnancy.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2003;25(6):431-436
DOI 10.1590/S0100-72032003000600008
PURPOSE: to analyze maternal death cases that occurred at the "Hospital de Clínicas de Porto Alegre", a reference university hospital for high-risk pregnancies in the state of Rio Grande do Sul, Brazil. METHODS: we carried out a retrospective study of medical records of 10- to 49-year-old women who died at the hospital between 1980 and 1999. Deaths related to pregnancy and puerperium were analyzed independently of the kind and duration of pregnancy. The causes were classified into direct obstetric, indirect obstetric and nonobstetric, according to their association with pregnancy, delivery and puerperium disorders. RESULTS: a total of 81 patients with a mean age of 28.5 years were studied. The maternal mortality rate was 109 per 100,000 live births. Direct obstetric causes made up 61.7% of deaths. Indirect causes made up 23.5% of deaths. Nonobstetric causes made up 15.0% of the total. Among direct obstetric causes, arterial hypertension (18.5%), post-cesarean infection (16%), and septic abortion (12.3%) were the most prevalent. The main maternal mortality events among indirect obstetric causes were cardiopathy (8.6%), acute fatty liver disease (3.5%), and systemic lupus erythematosus (2.5%). Among the nonobstetric causes, malignant neoplasia (7.4%) and AIDS (3.7%) were the most important. CONCLUSIONS: the prevailing causes of maternal death have not changed in the last two decades. The main cause is still hypertension. There is an expressive number of deaths related to cesarean section and infections. The high prevalence of direct obstetric causes shows the low maternal mortality prevention capacity of our health care system.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2003;25(3):155-161
DOI 10.1590/S0100-72032003000300003
PURPOSE: the morbidity in HIV-positive patients due to puerperal fever was studied and correlated to the method and duration of labor, the duration of premature rupture of the membranes, CD4+ cell count and the viral load (VL) at peridelivery. METHODS: a total of 207 HIV-positive women with prenatal examinations and deliveries between May 1997 and December 2001 were enrolled. Of these, 32 had natural childbirth and 175 had a cesarean section. Of the total of enrolled patients, 62.8% were submitted to elective cesarean section. The average age of the group was 27.4 years, and 25.6% were nulliparous and 26% were primiparous. At the moment of the delivery the average gestational age was 37.8 weeks. At the end of pregnancy the average of the CD4+ cell count was approximately 481 cells/mm³ and the viral load 49,100 copies/mL. RESULTS: puerperal morbidity occurred in 34 patients, with 33 after cesarean section and one after natural childbirth. The most usual intercurrent post-cesarean infection was that of the surgical wound (13% of the infection cases). Analyzed factors, such as delivery duration, duration of rupture of the membranes, number of CD4+ cells or the viral load at peridelivery, did not interfere in puerperal morbidity. CONCLUSIONS: puerperal morbidity was 16.8% and occurred more frequently after cesarean sections (18.9%) than after vaginal deliveries (3.1%). The other factors did not present a significant effect on puerperal morbidity.