You searched for:"Antônio Fernandes Moron"
We found (34) results for your search.Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2000;22(5):281-286
DOI 10.1590/S0100-72032000000500005
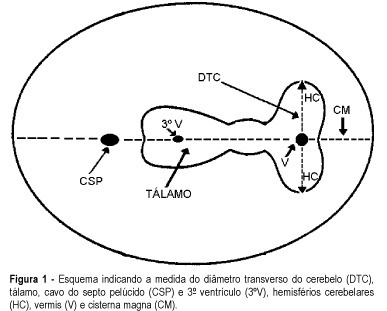
Purpose: to evaluate the effectiveness of the transverse cerebellar diameter (TCD), by ultrasonography, in the evolution of the fetal growth, and to relate it to gestational age, biparietal diameter (BPD), head circumference (HC), abdominal circumference (AC) and femur length (FL). Method: a prospective and longitudinal study was performed on 254 pregnant women considered of low risk, with a gestational age from 20 to 40 weeks. Only 55 pregnant women were included in the study, according to inclusion and exclusion criteria. All the examinations, 217 ultrasonographic evaluations, were done by the author (LN), at least three and at most six examinations for each pregnant woman being accomplished at an interval of one to five weeks. Normality patterns were established between the 10 and 90 percentiles for each gestational age and confirmed postnatally. Results: the transverse cerebellar diameter presented a good correlation with the gestational age either as a dependent variable (R² = 0.90) or as an independent variable (R² = 0.92). A significant relationship was found in the evaluation of the fetal growth between the TCD and the several fetal parameters: BPD and HC (R² = 0.92), FL (R² = 0.90) and AC (R² = 0.89). Conclusions: the transverse cerebellar diameter is a parameter that should be used in the follow-up of development and of fetal growth because of the ascending pattern of its growth curve. Any up- or downward alteration in the growth curve can be useful for the detection of deviations of fetal growth.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2004;26(8):641-647
DOI 10.1590/S0100-72032004000800008
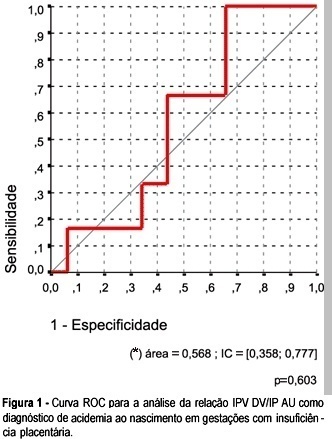
OBJECTIVE: to investigate whether it is possible to predict acidemia at birth in pregnancies with placental insufficiency using venous-arterial indices: pulsatility index for vein (PIV) of the ductus venosus (DV) over PI of the middle cerebral artery (MCA) and PIV of the DV over PI of the umbilical artery, and establish cut-off values for this prediction. PATIENTS AND METHODS: this was a prospective cross-sectional study involving forty-seven patients with placental insufficiency (umbilical artery resistance and pulsatility indices above the 95th percentile for gestational age) who were submitted to Dopplervelocimetry in the last 24 hours before delivery. All pregnancies were singleton, over 26 weeks of age and without structural or chromosome anomalies. Arterial cord blood was obtained for gasometry immediately after birth. Acidemia was defined as umbilical arterial pH < 7.20 in the absence of uterine contractions and pH < 7.15 in the presence of contractions. Metabolic or mixed acidemia at birth were considered pathological. A ROC curve was calculated for the venous-arterial indices: PIV DV/PI umbilical artery (UA) and PIV DV/PI MCA. A cut-off value was established and sensitivity, specificity, accuracy, positive and negative predictive values and positive and negative likelihood ratios were calculated. RESULTS: The DV/UA PI index was not a good predictor of acidemia at birth. The DV/MCA PI index was related to acidemia at birth (area under the curve 0,785, p = 0,004). The cut-off value was: 0,582, sensitivity 66,7%, specificity 77,1 and accuracy 74,5%. CONCLUSION: the PIV DV/PI MCA ratio is adequate for predicting acidemia at birth in pregnancies with placental insufficiency. The cut-off value was: 0,582.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2004;26(7):527-533
DOI 10.1590/S0100-72032004000700004
PURPOSE: to evaluate the diagnostic accuracy of hysterosalpingography (HSG) and transvaginal sonography (TVS) in terms of detecting uterovaginal anomalies in women with a history of recurrent miscarriage. METHODS: eighty patients who presented two or more consecutive miscarriages were submitted to HSG, TVS and hysteroscopy (HSC). The following diagnoses were considered separately: uterine malformations, intrauterine adhesions and polypoid lesions. Hysteroscopy was the gold standard. The matching among the different methods was evaluated by the kappa coefficient and its significance was tested. The significance level was 0.05 (alpha=5%). Sensitivity, specificity, positive and negative predictive values, with 95% of statistical confidence interval, were calculated. RESULTS: uterovaginal anomalies were detected in 29 (36.3%) patients: 11 (13.7%) were uterine malformations, 17 (21.3%) intrauterine adhesions and one (1.3%) a polypoid lesion. The global matching between HSG and HSC was 85.5%, while between TVS and HSC it was only 78.7%. The best accuracy of HSG appeared to be for the diagnosis of uterine malformations and intrauterine adhesions (diagnostic accuracy of 97.5 and 95%, respectively). For the diagnosis of polypoid lesions, HSG had a diagnostic accuracy of only 92.5%, due to the low rate of positive predictive value (14.3%). TVS had a worse accuracy for all diagnoses, 93.7% for the diagnosis of uterine malformations and 85% for intrauterine adhesions, due to low sensitivity. CONCLUSIONS: histerosalpingography showed a good diagnostic accuracy for the diagnosis of uterine cavity diseases. TVS had good specificity, but with low sensitivity.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2004;26(5):349-354
DOI 10.1590/S0100-72032004000500002
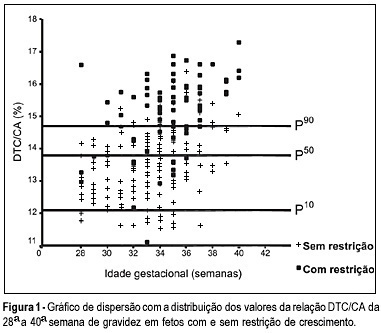
OBJECTIVE: to evaluate the accuracy of both the transverse diameter of the cerebellum (TDC) and of the transverse diameter/abdominal circumference (TDC/AC) ratio in the detection of fetal growth restriction (FGR), in high-risk pregnancies. METHOD: a prospective cross-sectional study was carried out in 260 patients with gestational age between 28 and 40 weeks. The TDC and AC of fetuses were measured through ultrasound and the fetuses with TDC below the 10th percentile or TDC/AC ratio above the 90th percentile (>14.6) were classified as FGR suspects. After birth, the accuracy of the TDC and TDC/AC was evaluated using the neonatal diagnosis of FGR as the gold standard (birth weight <10th percentile). RESULTS: after birth, 79 newborns (30.4%) were classified as small for gestational age. The TDC was appropriate in 74 (93.7%) of these fetuses and small in only 5 (6.3%). The sensitivity (SE), specificity (SP), positive (PPV) and negative (NPV) predictive values and accuracy of the TDC in the prediction of FGR were 6.3, 93.4, 29.4, 69.5, and 67%, respectively. The TDC/AC >14.6 correctly identified 59 of the 79 growth-restricted fetuses, with 27 false-positives and 20 false-negatives, SE of 74.5%, SP of 85.1%, PPV of 68.6%, NPV of 88.5% and 81.9% accuracy. CONCLUSION: the TDC is not a good screening parameter for the detection of FGR while the TDC/AC ratio above the 90th percentile is effective in this detection.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2004;26(3):193-200
DOI 10.1590/S0100-72032004000300004
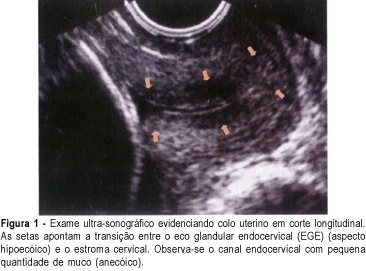
PURPOSE: to verify the prevalence of two sonographic findings, the cervical gland area (CGA) feature and the cervical length of less than 20 mm, and to compare these with the risk for premature delivery in pregnant women between 21 and 24 weeks' gestation. METHOD: this was a prospective, cross-sectional study in which 361 women were consecutively examined by transvaginal ultrasonography. Müllerian or other malformations, multiple gestations, fetal death, olygo- or polyhydramnios, marginal placenta previa, and conization, cerclage, amputation or other surgical procedures in the cervix, prior to or during pregnancy, were exclusion criteria. After the abdominal ultrasonographic morphological examination, we used transvaginal ultrasonography to measure the cervical length and to observe the presence of hyper- or hypoechoic area next to the endocervical canal, a feature characteristic of endocervical epithelium glands which is called CGA (cervical gland area). Qualitative variables are expressed as absolute and relative frequency. Quantitative variables are expressed as mean, median, standard deviation, minimum, and maximum values. Association between qualitative variables was detected by the c² test or by the Fisher exact test. For each variable, the relative risk and the 95% confidence interval (CI) were calculated. Logistic regression analysis was used to calculate the predictive values for premature delivery. Significance level was 95% (alpha = 5%), with descriptive (p) values equal or lower than 0.05 considered significant. RESULTS: spontaneous preterm delivery occurred in 5.0% of the patients. Cervical length was up to 20 mm in 3.3% of all studied patients and in 27.8% of those who delivered spontaneously before the end of the pregnancy. Absence of the CGA was detected in 2.8% of all patients and in 44.4% of the women who eventually developed spontaneous preterm labor. There was a statistically significant association of absence of CGA with short cervical length (p<0.001). Absence of CGA was strongly associated with spontaneous preterm delivery (relative risk of 28.57, 95% CI 14.40-56.68). CONCLUSION: the absent CGA feature is a new morphological ultrasonographic parameter that is useful in the prediction of spontaneous preterm delivery in single gestations. Our results show that the parameter can be used as an indicator of risk for premature delivery, to be confirmed by future research.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2004;26(1):15-20
DOI 10.1590/S0100-72032004000100003
PURPOSE: to analyze the values of Doppler ultrasound for blood flow velocity in the ductus venosus between the 10th and the 14th week of gestation, during the different phases of the cardiac cycle: ventricular systole (wave S), ventricular diastole (wave D), atrial systole (wave a), and angle-independent indexes. METHODS: Doppler was used in this prospective cross-sectional study to examine 276 single pregnancies. Fetus malformations, abnormal nuchal translucency, and women with clinical pathologies were excluded. A Toshiba SSH-140 ultrasound equipment was used. The derivation of Doppler frequency spectra was carried out according to standardized measurement procedures: less than 30ºinsonation angle and 50-70 Hz high-pass filter. The ductus venosus was identified in a median sagittal and ventral plane with the presence of color aliasing due to increase in blood flow velocity. The sample volume (1-2 mm³) was placed immediately at the origin of the ductus venosus. At least three clearly and subsequent waves were available for measurement of standard values. The Levene test and the Bonferroni method were used for statistical analysis. RESULTS: increase in blood flow velocity from 29 cm/s to 37 cm/s (p=0.013) was observed during ventricular systole between the 10th and the 14th week of gestation. Similarly, increase in blood flow velocity was recorded during the ventricular diastole (from 25 cm/s to 32 cm/s, p=0.026). There were no changes in wave a, pulsatility index, and S/a ratio in this period. CONCLUSION: the reference ranges established by this study may serve as the basis for Doppler ultrasound follow-up in a normal patient population. Further studies are required to determine the validity of these parameters and, in particular, for the fetus at risk.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2003;25(7):475-479
DOI 10.1590/S0100-72032003000700003
PURPOSE: to study the effects of low-dose oral hormonal contraceptives (OHC) (<30 mg of ethynylestradiol) on the intraerythrocytic folate levels. METHODS: this was a prospective transversal study with 95 patients treated in the Family Planning Clinic of UNIFESP (Federal University of São Paulo). The control group (Condom group) consisted of patients using condom as their exclusive contraceptive method during the last 12 months, and the study groups consisted of patients using low-dose oral hormonal contraceptives, in the following way: OHC 3 group (three to six months of use), OHC 6 group (six to twelve months of use) and OHC 12 group (more than twelve months of use). Intraerythrocytic folate was determined by the ionic capture method. Analysis of variance and c² test were used for statistical analysis. RESULTS: the Condom group showed a rate of 44% of patients with folate lower than 186.0 ng/mL and the users of low-dose oral contraceptives showed a rate of 32% (OHC 3 group), 16% (OHC 6 group) and 31% (OHC 12 group). We did not find in the group using low-dose oral contraceptives a significant reduction in the average level of intraerythrocytic folate compared to the control group and there was no statistically significant difference (p=0.28) regarding time of use. CONCLUSION: we observed reduced levels of intraerythrocytic folate in a significant number (44%) of patients not using low-dose oral hormonal contraceptives. Their rates were similar to the lower limit considered to be normal by most authors, which points to a basal folate deficiency in the studied group. We did not observe any alteration in the level of intraerythrocytic folate in patients using low-dose oral hormonal contraceptives.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2003;25(6):425-430
DOI 10.1590/S0100-72032003000600007
PURPOSE: to determine whether prenatal sonographic findings and uterine contractions can predict neonatal motor outcome in fetuses with open spina bifida. METHODS: we evaluated retrospectively 53 fetuses with open spina bifida from 1993 to 2001. These fetuses were born and followed-up at the fetal medicine units of the Hospital São Paulo ("Universidade Federal de São Paulo") and the "Hospital Santa Joana". The influence of the alterations observed through ultrasound scan on neonatal muscular strength (macrocrania, microcrania, level of the spinal column opening, clubfoot and type of fetus position) was evaluated. The influence of uterine contractions on neonatal motor outcome was also evaluated. All deliveries were made through cesarian section. c² and Fisher tests were used for categorical comparisons. A p<0.05 was considered significant. RESULTS: Fifty-three cases of isolated open spina bifida were studied. Alterations of the cranial circumference size and the level of the lesion did not interfere in the neonatal motor perfomance. However, clubfoot and breech position showed to be predictors of an unfavorable neurological prognosis (p<0.05). Twenty-tree (43%) infants had clubfoot. Eighteen (78.3%) of these had abnormal leg movements. No infant in breech presentation (n=10) showed normal motor function. The presence of uterine contractions and the premature membrane rupture, observed in 13 fetuses (87%), were also linked to the alteration of neonatal muscular strength (p<0.05). CONCLUSION: clubfoot and breech presentation are ultrasonographic findings useful in predicting neurological neonatal outcome. Uterine contractions and premature membrane rupture are associated with poor motor neonatal outcome.