You searched for:"Paulo César Giraldo"
We found (9) results for your search.Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2022;44(2):169-177
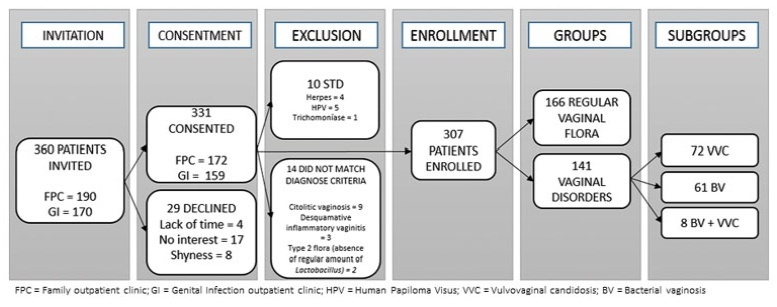
To evaluate genital hygiene among women with and without bacterial vaginosis (BV) and/or vulvovaginal candidiasis (VVC).
A cross-sectional study of reproductive-aged women who underwent gynecological and laboratory tests and fulfilled a genital hygiene questionnaire.
This study evaluated 166 healthy controls and 141 women diagnosed with either BV (n=72), VVC (n=61), or both (n=8). The use of intimate soap and moist wipes after urination was more frequent among healthy women (p=0.042 and 0.032, respectively). Compared to controls, bactericidal soap was more used by women with BV (p=0.05).
Some hygiene habits were associated to BV and/or VVC. Clinical trials should address this important issue in women’s health.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2020;42(10):634-641
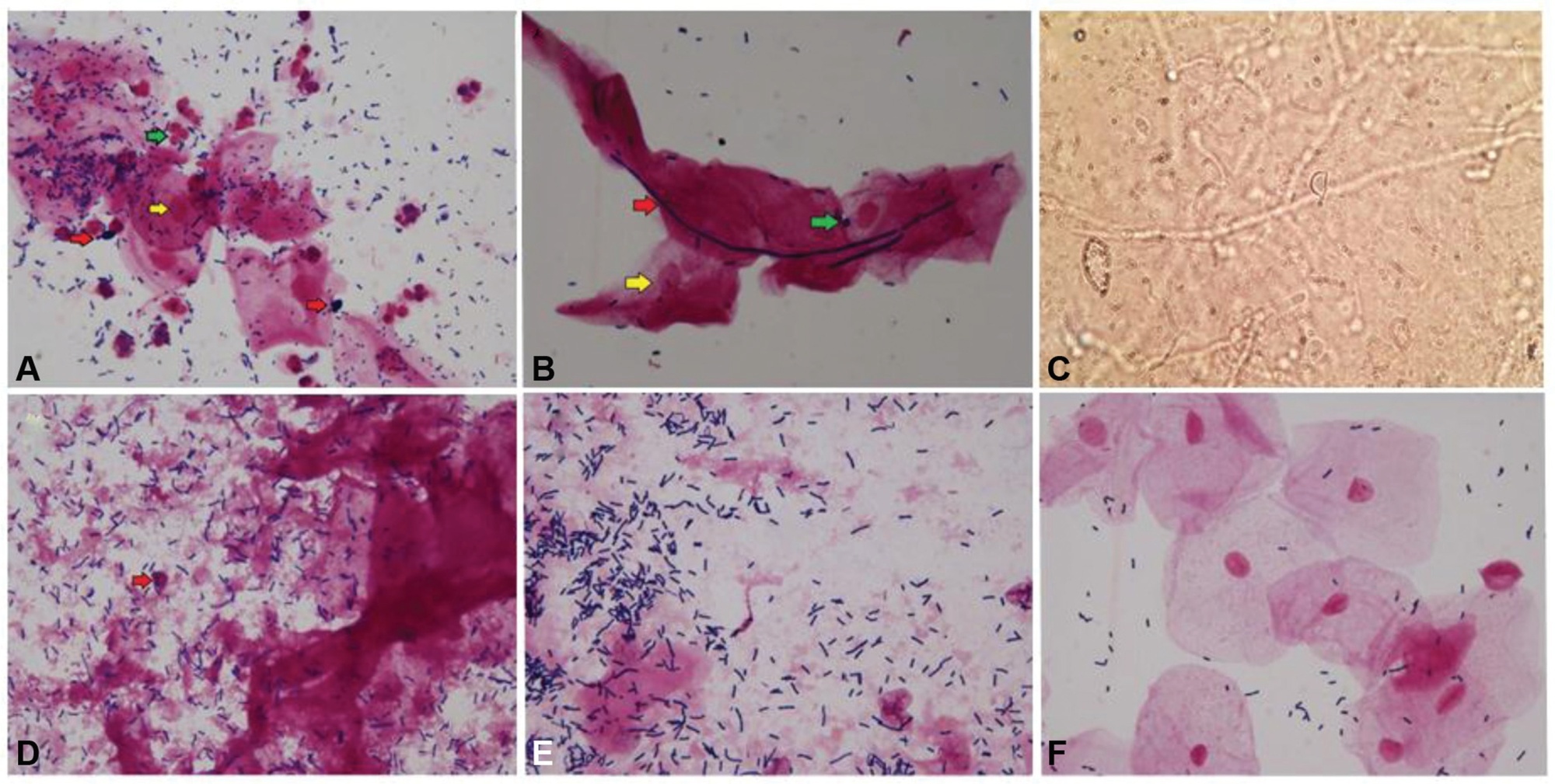
To identify clinical, microscopic, and biochemical characteristics that differentiate cytolytic vaginosis (CV) from vulvovaginal candidiasis (VVC).
The present cross-sectional study analyzed the vaginal contents of 24 non-pregnant women aged 18 to 42 years who were attended at the Genital Infections Clinic at Centro de Atenção Integral à Saúde da Mulher da Universidade Estadual de Campinas (CAISM-UNICAMP). They were diagnosed either with (CV = 8, VVC = 8) or without vulvovaginitis or vaginal dysbiosis (controls). The socio-demographic, clinical, and gynecological data were obtained from a detailed patient interview. Samples of the vaginal contents were collected for analysis of vaginal pH, gram stain, and specific fungal culture. The Kruskal-Wallis and Fisher exact tests were used to compare the differences between the groups. Odds ratios were used to compare the categorical variables. The significance level was considered at p < 0.05.
Both women with CV and VVC had a lumpy vaginal discharge (p = 0,002) and vaginal hyperemia (p = 0.001), compared with controls. The inflammatory process was more intense in the VVC group (p = 0.001). In the CV group, there was statistical significance for the lactobacillus amount (p = 0.006), vaginal epithelium lysis (p = 0.001), and vaginal pH (p = 0.0002).
Cytolytic vaginosis and VVC diagnoses rarely differ on clinical characteristics but have different laboratorial findings. The present study highlights the importance of conducting an accurate investigation through laboratory tests rather than clinical criteria to avoid misdiagnosis.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2017;39(5):235-248
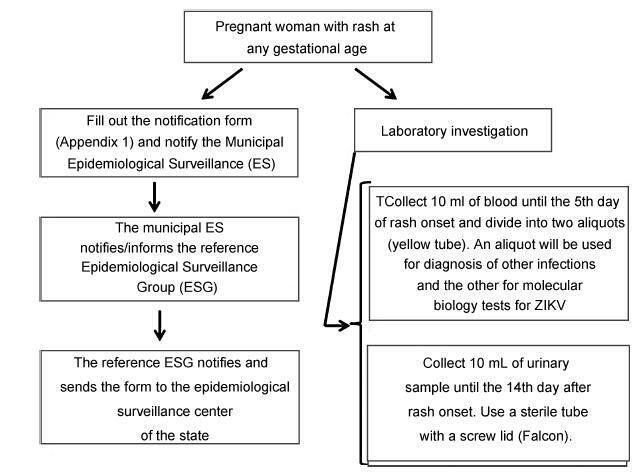
From the discovery of the Zika virus (ZIKV) in 1947 in Uganda (Africa), until its arrival in South America, it was not known that it would affect human reproductive life so severely. Today, damagetothe central nervous system is known to be multiple, and microcephaly is considered the tip of the iceberg. Microcephaly actually represents the epilogue of this infection’s devastating process on the central nervous system of embryos and fetuses. As a result of central nervous system aggression by the ZIKV, this infection brings the possibility of arthrogryposis, dysphagia, deafness and visual impairment. All of these changes of varying severity directly or indirectly compromise the future life of these children, and are already considered a congenital syndrome linked to the ZIKV. Diagnosis is one of the main difficulties in the approach of this infection. Considering the clinical part, it has manifestations common to infections by the dengue virus and the chikungunya fever, varying only in subjective intensities. The most frequent clinical variables are rash, febrile state, non-purulent conjunctivitis and arthralgia, among others. In terms of laboratory resources, there are also limitations to the subsidiary diagnosis. Molecular biology tests are based on polymerase chain reaction (PCR)with reverse transcriptase (RT) action, since the ZIKV is a ribonucleic acid (RNA) virus. The RT-PCR shows serum or plasma positivity for a short period of time, no more than five days after the onset of the signs and symptoms. The ZIKVurine test is positive for a longer period, up to 14 days. There are still no reliable techniques for the serological diagnosis of this infection. If there are no complications (meningoencephalitis or Guillain-Barré syndrome), further examination is unnecessary to assess systemic impairment. However, evidence is needed to rule out other infections that also cause rashes, such as dengue, chikungunya, syphilis, toxoplasmosis, cytomegalovirus, rubella, and herpes. There is no specific antiviral therapy against ZIKV, and the therapeutic approach to infected pregnant women is limited to the use of antipyretics and analgesics. Anti-inflammatory drugs should be avoided until the diagnosis of dengue is discarded. There is no need to modify the schedule of prenatal visits for pregnant women infected by ZIKV, but it is necessary to guarantee three ultrasound examinations during pregnancy for low-risk pregnancies, and monthly for pregnant women with confirmed ZIKV infection. Vaginal delivery and natural breastfeeding are advised.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2017;39(4):169-174
Vaginal pessary is used as a conservative treatment for pelvic organ prolapse (POP). Some studies have shown that common complaints of its use may include vaginal discomfort and increased vaginal discharge. Scant information is available about the microflora status after using this device.
To determine if the usage of vaginal pessary can interfere with the vaginal environment.
A cross-sectional study was performed from March of 2014 to July of 2015 including 90 women with POP. The study group was composed of 45 women users of vaginal pessary and 45 nom-users. All enrolled women answered a standardized questionnaire and were subjected to a gynecological exam to collect vaginal samples for microbiological evaluation under optic microscopy. Clinical and microbiological data were compared between study and control groups.
Vaginal discharge was confirmed in 84% of the study group versus 62.2% in the control group (p< 0.01); itching was reported in 20 and 2.2%, respectively (p< .05); genital ulcers were only found in the pessary group (20%). There was no difference with regard to the type of vaginal flora. Bacterial vaginosis was prevalent in the study group (31.1% study group versus 22.2% control group), (p=.34).
Women using vaginal pessaries for POP treatment presented more vaginal discharge, itching and genital ulcers than non-users.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2013;35(10):453-457
DOI 10.1590/S0100-72032013001000005
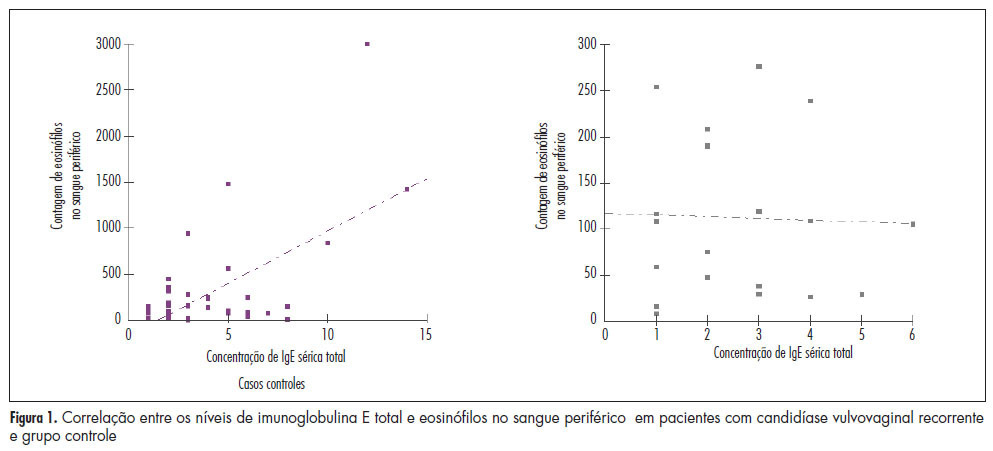
PURPOSE: To quantify the number of defense cells and immunoglobulin E (IgE) levels in peripheral blood sampled from women with recurrent vulvovaginal candidiasis. METHODS: A cross-sectional study was conducted on 60 women, 40 with vulvovaginal candidiasis and 20 controls. The defense cells were identified using an impedance system combined with flow cytometry and total and specific IgE was measured by chemiluminescence. The Mann-Whitney test was used for nominal variables and the Spearman test was used to determine the correlation of IgE concentration and eosinophils in peripheral blood. RESULTS: The number of eosinophils in peripheral blood from patients with recurrent vulvovaginal candidiasis, 302.60 (±253.07), was significantly higher compared to control, 175.75 (±109.24) (p=0.037). Serum levels of total and specific IgE were similar in the groups of women with and without recurrent vulvovaginal candidiasis (p=0.361). However, there was a moderate positive correlation between eosinophils and total serum IgE in the candidiasis group (r=0.25). CONCLUSION: Women with recurrent vulvovaginal candidiasis are more likely to have eosinophils in peripheral blood.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2011;33(12):408-413
DOI 10.1590/S0100-72032011001200006
PURPOSE: To evaluate the influence of physical activity on the quality of life of middle-aged women. METHODS: A population-based cross-sectional study was conducted on 370 women aged 40 to 65 years-old recruited from a population-based sample. Enrollment took place in Basic Health Units in each health district of the city (North, South, East, and West) from June to September 2011. According to the Municipal Health Department of the City, 20,801 women were assisted at the Basic Health Units during a one-year period. The sample size calculation was stratified by district and based on a 95% confidence level with a power of 80%, as well as an error estimate of 5% and it was considered proportional to the number of patients classified as having adequate quality of life (indicator >26) in the general population. Data were collected while women waited for their routine appointment at the Health Unit. WHOQOL-Bref was used to evaluate the quality of life, and menopause rating scale (MRS) was used to determine climacteric symptoms. The level of physical activity was assessed by means of the International Physical Activity Questionnaire (IPAQ). To obtain the classification of PA levels, we used three categories: sedentary, moderately active, and very active. Statistical analysis was performed using the Minitab software, version 16. RESULTS: The mean age of the subjects was 49.8 years-old (±8.1) and they were predominantly Caucasian (72.7%), married (61.6%), non-smokers (93.5%), and had High School education (47.8%). Using the WHOQOL, mean scores were found to be significantly different between the groups (low, moderate, and vigorous physical activity), classified according to the domains of quality of life (p<0.01). Concerning physical activity and climacteric symptoms, significant differences were found for all domains: psychological (p<0.01), vegetative-somatic (p<0.01), and urogenital (p<0.01). CONCLUSIONS: Physical activity improves quality of life in middle-aged women.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2010;32(8):413-413
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 1998;20(8):437-441
DOI 10.1590/S0100-72031998000800002
Purpose:to compare the incidence of preterm labor and birth, premature rupture of membranes (PROM) and low birth-weight newborns (< 2,500 g) between two groups of pregnant women (with or without BV). To verify the adequacy of including a regular prenatal BV investigation. Methods:a total of 217 women between 28 and 32 weeks of pregnancy (35 with BV and 182 without BV) were studied. The diagnosis of BV was established according to Amsel's criteria. The data were analyzed by the chi² test, Fisher's test, Mann-Whitney test and the relative risk. Results:the incidence of preterm labor, preterm birth, PROM and low birth-weight was statistically higher in the group of women with BV than in the control group (29.4% vs. 3.8%; 28.6% vs. 3.3%; 22.9% vs. 10.4%; 20.0% vs. 3.3%; respectively). The means of gestational age and birth-weight were significantly lower in the newborns from mothers with BV (265.8 days vs. 279.9 days; 2,958 g vs. 3,294 g, respectively). Conclusion:all perinatal complications studied were significantly associated with the presence of untreated BV during pregnancy. Therefore, the diagnosis and adequate treatment should be included in the routine prenatal assistance at Brazilian Obstetrics Services. Such measure may be effective in the reduction of these perinatal complications.